Abstract
Cognition is frequently damaged by acquired brain injury (ABI). Impaired thinking is both a symptom in its own right and also a barrier to recovery by impacting their insight and awareness and their engagement with rehabilitation. Here we consider the aims, mechanisms and contexts when the goal is to improve cognitive function in patients with ABI.
Key take home points:
- Before intervening we need to understand who the patient is. Holistic assessment using multiple methods of testing are necessary to establish this.
- The patient’s conceptualization of their relationships (social cognition) and how they view their own cognitive processes (metacognition) are both necessary targets for rehabilitation.
- Therapeutic strategies must involve: i) working with people in the patient’s social network; ii) building insight and awareness; iii) the time window for interventions should never close.
Cognitive rehabilitation and assessment of function
Cognitive rehabilitation involves the restoration of function in people who have experienced a change in their cognitive abilities. This is usually a return to participation in meaningful activities and improved quality of life. For the purposes of this short review, we will focus on those with cognitive under-functioning caused by acquired brain injury (ABI). Skilled assessment is essential if we want to quantify change, but it is fraught. In a sense, all cognitive tests are proxies of what they claim to measure and there is no standard battery that will adequately characterise all patients. Data from ‘off-line’ pen-and-paper tests, if possible, should be complimented with more practical assessments in function. Finally, as cognitive impairments are almost always relative, one needs to establish a reasonable estimation of a person’s pre-morbid function.
Mechanisms
It is helpful to think about this using the analogy of motor recovery. There are two key aspects: the first relates to what we are trying to change, the second to how we might change it.
What are we trying to achieve?
When looking at outcomes in the motor recovery literature, there is a clear distinction between restitution and compensation [1]. In the former, the manner of the repaired behaviour (e.g. drinking from a cup) is indistinguishable from the pre ABI state (the drinking movements are carried out in the same way as they were pre injury); in the latter, the same goal is achieved but the way that the task is completed is visibly different from before. Here, compensatory strategies are employed, i.e. new ways of doing old things. The gold standard for motor recovery is restitution rather than compensation, with some arguing that compensatory strategies should be discouraged as they limit the final ceiling of observable recovery [2]. Does this paradigm hold true for cognition? It is hard to tell as the measurable output (a given behaviour) can be produced by many different combinations of internal states and thought processes that themselves are hard to quantify (e.g. indistinguishable reading performance across subjects, can be driven by several very different patterns of cortical network activity [3[). Indeed, it is our view that almost all cognitive rehabilitation relies on some form of strategy-based process. For example, a major cause of frustration in supporting memory function in a patient going back to work may involve introducing them to what they believe to be novel and thus more effortful approaches, such as note taking, reminders and fatigue management. However, these explicit strategies are simply drawn from the common armoury of mental methods used in everyday functioning. Indeed, the patient will have used a different range of these to carry out tasks previously, but they will have become so ingrained as to feel effortless. The process of this type of rehabilitation is to facilitate patients to develop behaviours that they initially might resent, as it represents loss of their previous identity; yet with practice and habituation, these behaviours become implicit.
The behaviours that we are trying to change either relate to how patients interact with others (e.g. communication, social cognition, vocational rehabilitation) or how they view themselves (e.g. insight and awareness). The goal is to help the patient navigate toward these altered, recovering cognitive states, and maintain them.
How are we trying to achieve it?
In motor recovery, the general principle is mass practice with feedback, so the patient undergoes many hundreds or thousands of guided repetitions to reach their goal. Is the same true for cognition? Interventions targeting behaviour change generally do not follow a massed-practice approach, rather they require the patient to migrate from one behavioural state to another. This can occur, rarely, with a single event (one-shot) or single-session learning [4], but more often requires a series of tailored interventions which incrementally bridge the gap between the current state and desired goals. When helping a patient adjust their behaviour and/or world view, new problems may arise. For example, it is not uncommon for patients to experience a deterioration in their mood as therapists work on insight and awareness relating to the impact of their ABI and what this means for them. Therefore, psychological well-being needs to be assessed and treated throughout the patient pathway [5].
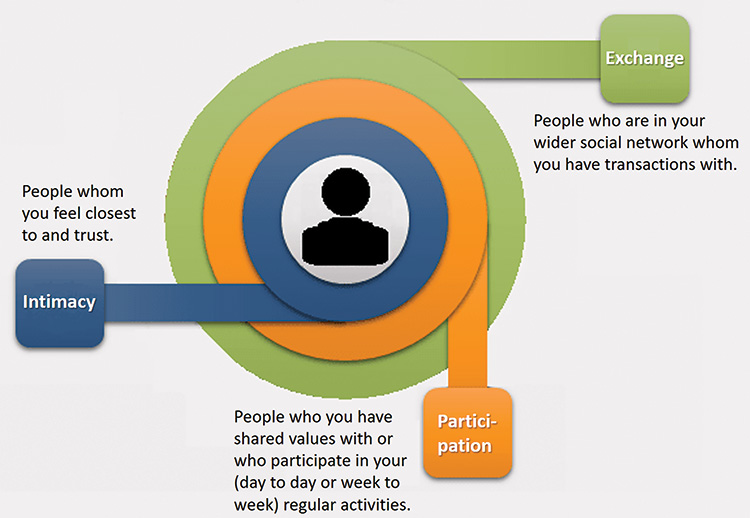
Techniques and approaches to improving patients’ cognitive functioning are legion but can be conceptualised along the following two key dimensions of complexity and social context (visualised with the individual at the centre and concentric rings representing carers and loved ones, then wider social contacts such as friends and colleagues). Simpler interventions include psychoeducation, which can be aimed at the person with ABI, their family or other people they interact with (e.g. helping work colleagues support the patient). Moving through the social contexts, more complex interventions include: 1) for the individual with ABI: increasing insight and awareness (see metacognition section below), working on individual cognitive impairments, adjustment and acceptance [6]; 2) for carers and loved ones: conversation partner training, couples or family therapy; 3) wider social contacts such as the workplace: facilitating communication, coaching, negotiating reasonable adjustments [7].
Social context and social cognition
We all exist in a complex web of social relationships which both define our sense of place in the world and help us understand who we are. Social cognition has been defined as any cognitive process that involves other people either at a group level or on a one-to-one basis. ABI can have a devastating effect on social cognition which enables these meaningful interactions with others. Cognitive impairments and the effect brain injury has directly and indirectly on mood, affect these relationships, often putting them under intolerable strain [8]. Patients with brain injury find maintaining friendships difficult and harder still to acquire new ones, social webs can become eroded and therefore the responsibility of social support can fall on an ever reducing number of people. Positive outcomes for rehabilitation are closely linked to this support and interventions, therefore, need to be systemic and encompass the patient’s key relationships, which can include psychoeducation; however, the needs of the carer are often overlooked. This can be addressed by providing psychotherapeutic interventions that take account of the loss that they have suffered and their adjusted role(s). We have found that a group setting where relatives gather in a real or virtual ‘carers’ café’ to share their lived-experiences with each other and a Clinical Psychologist [9] can be powerful and authenticating.
Metacognition
Metacognition refers to the ability to reflect on, monitor and control other cognitive processes, often in the absence of feedback. In the most reductive form, behavioural therapies can be used to improve how people with ABI respond without requiring them to understand much about why their behaviour has changed. But for most of what takes place in cognitive rehabilitation, patients need to be able to mentalise themselves. Metacognition refers to this ability, to reflect on, monitor and control one’s own cognitive processes. Metacognitive impairments are very common after ABI, and like social cognition, are rarely formally assessed, perhaps because there is no agreement on which tools are best to do this [10]. Therapists often talk about patients’ readiness to change being associated with better outcomes, metacognitive awareness is part of this and supports learning in the undamaged brain [11]. Increasing self-awareness in patients with ABI encourages them to form a perspective of themselves outside of themselves. Methods to achieve this include sensitive sharing of assessment results, guided reflection using video recordings of the patient, supervised feedback from others (e.g. family members and/or work colleagues). Holistic interventions have also shown promise in improving ABI patients’ metacognitive abilities [12]. Shifts in self-awareness and subsequent consistent changes in behaviour often take time to be established. The implication of this is that the optimum timing of intensive rehabilitation may be distal to the brain injury. This necessitates that health care systems monitor and reassess patients with ABI throughout their lifespan.
References
1. Reinkensmeyer DJ, Burdet E, Casadio M, Krakauer JW, Kwakkel G, Lang CE, et al. Computational neurorehabilitation: modeling plasticity and learning to predict recovery. J Neuroeng Rehabil 2016;13(1):42. https://doi.org/10.1186/s12984-016-0148-3
2. Murata Y, Higo N, Oishi T, Yamashita A, Matsuda K, Hayashi M, et al. Effects of motor training on the recovery of manual dexterity after primary motor cortex lesion in macaque monkeys. J Neurophysiol 2008;99(2):773-86. https://doi.org/10.1152/jn.01001.2007
3. Kherif F, Josse G, Seghier ML, Price CJ. The Main Sources of Intersubject Variability in Neuronal Activation for Reading Aloud. Journal of Cognitive Neuroscience 2009;21(4):654-68. https://doi.org/10.1162/jocn.2009.21084
4. Fu V, Weatherall M, McPherson K, Taylor W, McRae A, Thomson T, et al. Taking Charge after Stroke: A randomized controlled trial of a person-centered, self-directed rehabilitation intervention. International journal of stroke : official journal of the International Stroke Society 2020;15(9):954-64. https://doi.org/10.1177/1747493020915144
5. Doogan C, Dignam J, Copland D, Leff A. Aphasia Recovery: When, How and Who to Treat? Curr Neurol Neurosci Rep 2018;18(12):90. https://doi.org/10.1007/s11910-018-0891-x
6. Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behav Res Ther 2006;44(1):1-25. https://doi.org/10.1016/j.brat.2005.06.006
7. Leary S, Hurford J, Shanahan N. An expert opinion: Vocational rehabilitation after stroke. Advances in Clinical Neuroscience and Rehabilitation 2020. https://doi.org/10.47795/OEAP6518
8. Marsh NV, Kersel DA, Havill JH, Sleigh JW. Caregiver burden at 1 year following severe traumatic brain injury. Brain injury 1998;12(12):1045-59. https://doi.org/10.1080/026990598121954
9. Klonoff PS. Psychotherapy after brain injury : principles and techniques. New York: Guilford Press; 2010. xiii, 288 p. p.
10. Al Banna M, Redha NA, Abdulla F, Nair B, Donnellan C. Metacognitive function poststroke: a review of definition and assessment. Journal of neurology, neurosurgery, and psychiatry 2016;87(2):161-6.
11. Fleming SM, Dolan RJ, Frith CD. Metacognition: computation, biology and function. Philos Trans R Soc Lond B Biol Sci 2012;367(1594):1280-6. https://doi.org/10.1098/rstb.2012.0021
12. Cicerone KD, Goldin Y, Ganci K, Rosenbaum A, Wethe JV, Langenbahn DM, et al. Evidence-Based Cognitive Rehabilitation: Systematic Review of the Literature From 2009 Through 2014. Archives of physical medicine and rehabilitation 2019;100(8):1515-33. https://doi.org/10.1016/j.apmr.2019.02.011

