In 2015 the Tri-borough Clinical Commissioning Group (CCG) Commissioners of ‘Hammersmith and Fulham’, ‘Kensington and Chelsea’ and ‘Westminster’ together with clinicians designed the innovative virtual bed model to help with the issue of poor access to community rehabilitation. The Specialist Neurological Rehabilitation Service (SNRS) model was crafted so that the inpatient service and the virtual beds would be integrated as part of the same service. The SNRS service is made up of 19 beds in total. There are 15 hospital-based beds in Charing Cross Neurological Rehabilitation Unit (CNRU) where rehabilitation is provided to patients on the premises as in-patients. There are also a further 4 virtual beds where rehabilitation is provided to patients in their own homes. The virtual bed service is called the Specialist Neurological Rehabilitation Outreach Service (SNROS). The host provider for the SNRS is the Acute Trust which operationally manages the service via a series of service level agreements (SLA) with the other partners in the community to support the therapy input to the virtual beds.
Abstract
The total number of neurological cases in England was around 16.5 million in 2019 [2]. The Neurological Alliance estimates that at least 1 in 6 people live with one or more neurological condition(s) [3]. This figure will continue to rise in part due to the impact of an ageing population. Specialist rehabilitation has been proven to be highly cost-effective for all neurological conditions, producing substantial savings in ongoing care costs, especially in the most dependent patients [4]. Current issues highlighted by the ICS include long waiting lists particularly to get into level 1 rehabilitation units. In addition to this, there is a disparity in the provision of community rehabilitation across the UK. The lack of availability of community rehabilitation is often a key reason given by clinicians for their reluctance to discharge patients earlier from inpatient beds.
One of the main priorities of the Integrated Care Systems (ICS) is to expand the number of ‘virtual wards’ and deliver multidisciplinary care for patients closer to home. We present to you the Specialist Neurological Rehabilitation Service (SNRS) which has demonstrated over the last 7 years that intensive neurological rehabilitation can be delivered successfully in the patients’ own homes.
A novel commissioning model has been used in partnership with different NHS trusts to provide a unified neurorehabilitation service with both inpatient hospital beds and virtual beds in the patients’ own homes. While patients are on the virtual bed pathway, they remain under the care of the Consultant in Rehabilitation Medicine with support from the Clinical Nurse Specialist and have access to diagnostics/interventions and clinic reviews. The patients get daily intensive MDT therapy input from the skilled community team who provide the same frequency of therapy sessions at home (as they would get in a level 2 inpatient neurorehabilitation unit). This pathway is supporting the earlier discharge of patients from hospital. Additionally, the analysis of data from the virtual bed pathway shows that rehabilitation outcomes in patients’ own homes are similar to those of bedded units for this subset of patients with complex neurological needs. This illustrates that the virtual ward model can be successfully implemented in neurorehabilitation.
Introduction
One of the main priorities of the Integrated Care Systems (ICS) in 2022/23 was to expand the number of ‘virtual wards’ and deliver multidisciplinary care for patients closer to home [1]. The main focus was on preventing hospital admissions and facilitating early discharge. During the pandemic, there was considerable success in implementing virtual wards for managing ‘acute respiratory infections’ and ‘frailty’ [1]. However, we would like to demonstrate that the virtual ward / ‘Hospital at Home’ model also works well in neurological rehabilitation and can have the same benefits of reducing hospital admissions while providing patients with specialist rehabilitation in their own home. The Specialist Neurological Rehabilitation Service (SNRS) has been running a virtual ward successfully for the past 7 years. The service has demonstrated that by drawing on the expertise of the whole system, intensive neurological rehabilitation can be delivered effectively in the community.
Several patients during their inpatient rehabilitation will reach a stage where their medical and nursing needs can be managed safely at home. However, they continue to have complex rehabilitation needs with multi-disciplinary therapy goals. These patients can be discharged into the virtual beds with a package of care (if required) and additionally get the same frequency of therapy sessions as in the level 2 inpatient unit at home. Patients in the virtual neurological rehabilitation beds remain under the care of the Consultant in Rehabilitation Medicine, Clinical Nurse Specialist (CNS) and Multi-Disciplinary-Team (MDT) in the community.
The SNROS virtual beds improve things in four key ways:
1. Direct transfer to the community setting for intensive rehabilitation: patients who are waiting for inpatient rehabilitation beds while on acute wards (for e.g. major trauma unit, neurology/neurosurgery services) can be discharged directly to the virtual beds, where their medical/nursing and therapy needs can be supported at home.
2. Optimising flow in the whole system: patients can be discharged from the inpatient rehabilitation unit or directly from acute wards to the virtual beds hence optimising flow in the whole system. Patients continue to have high intensity of therapy on discharge and no delay in waiting for community therapy.
3. Rehabilitation at home: patients are discharged into their own homes and get intensive rehabilitation (the same intensity as level 2 rehabilitation unit) at home. This allows patients to receive specific functional task training and enables problem solving in a familiar setting.
4. Continuity of care: the patient remains under the care of the Consultant in Rehabilitation Medicine who is in charge of the inpatient beds in the specialist neuro-rehabilitation unit. The SNROS therapists are also part of the wider Community Neurological Rehabilitation Service (CNRS). Hence when stepped down from the SNROS service, the same therapists will continue to treat the patient on the less intensive CNRS pathways. Unlike patients that receive Early Supported Discharge (ESD) care, patients on the SNROS pathway can access diagnostics/blood tests/clinic reviews etc more rapidly and, if necessary, via the Consultant and Clinical Nurse Specialist.
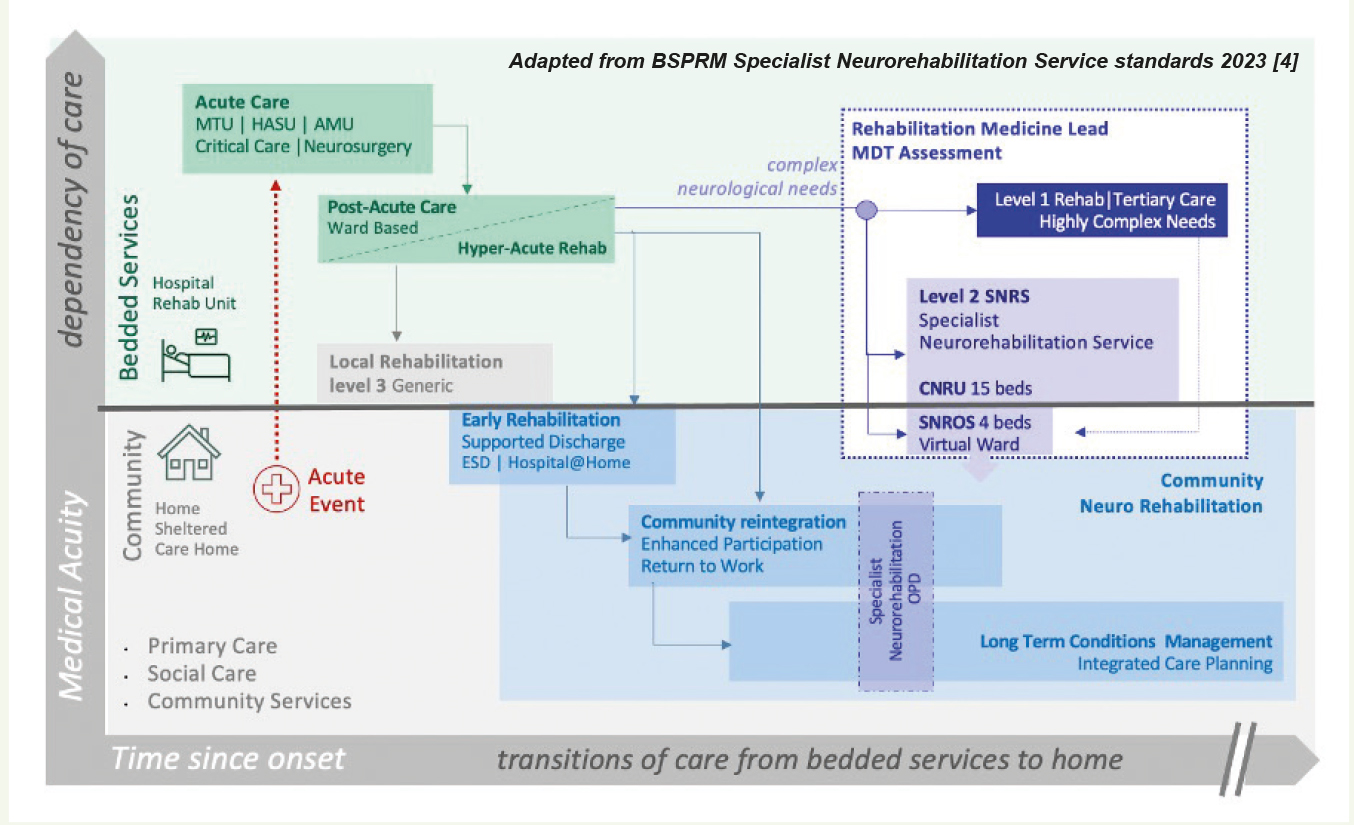
Figure 1: Figure adapted from BSPRM Specialist Neurorehabilitation Service standards 2023 [4] to illustrate the relationship between level 2 bedded and virtual ward neurorehabilitation services, as a means of providing specialist neurorehabilitation to patients with complex needs, directly from acute inpatient services into the community, as well as supporting the transition from level 1 and 2 bedded neurorehabilitation services back into their homes with a seamless transition of care into community neurorehabilitation pathways and long-term condition management. Ongoing specialist support is offered via multi-disciplinary-meetings/clinics/home visits on an outpatient basis to support long-term conditions e.g. spasticity management.
Innovative Commissioning – Sharing the expertise from where it already exists
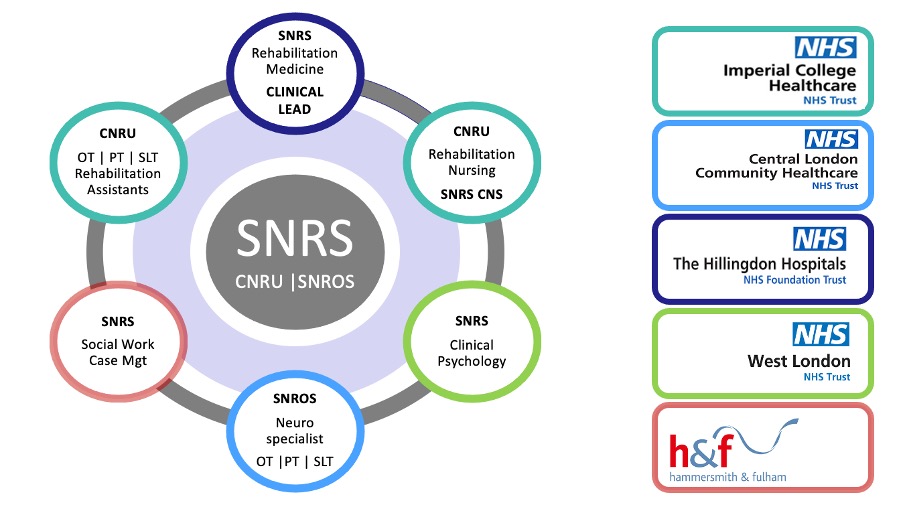
As previously mentioned, the SNRS service is comprised of hospital-based beds in CNRU and virtual beds in the patient’s own home (SNROS). The design of the SNRS service is novel. It is formed through partnerships between different organisations in order to obtain the expertise from where it already exists. The host partner is Imperial College Healthcare Trust where the inpatient CNRU beds are based. Imperial College Healthcare Trust employs the staff including the nursing and therapy team. The Rehabilitation Medicine consultant input comes from The Hillingdon Hospital Trust where there has been an established inpatient rehabilitation unit for over 25 years. Clinical psychology input for CNRU is provided through the West London Trust. The therapy input for the virtual beds is provided by the Central London Community Healthcare Trust (CLCH) which manages a flexible caseload covering services for Early Supported Discharge (ESD) for stroke, CNRS pathways (including less intensive MDT neurorehabilitation, disability management and rapidly progressive pathways) as well as our SNROS service.
Everyone at SNRS works through a Service Level Agreement (SLA) with Imperial College Health Care Trust. The staffing is based on British Society of Physical and Rehabilitation Medicine (BSPRM) ‘Specialised Neuro-rehabilitation Service Standands’ for level 2 rehabilitation unit [4].
The day to day running of the service
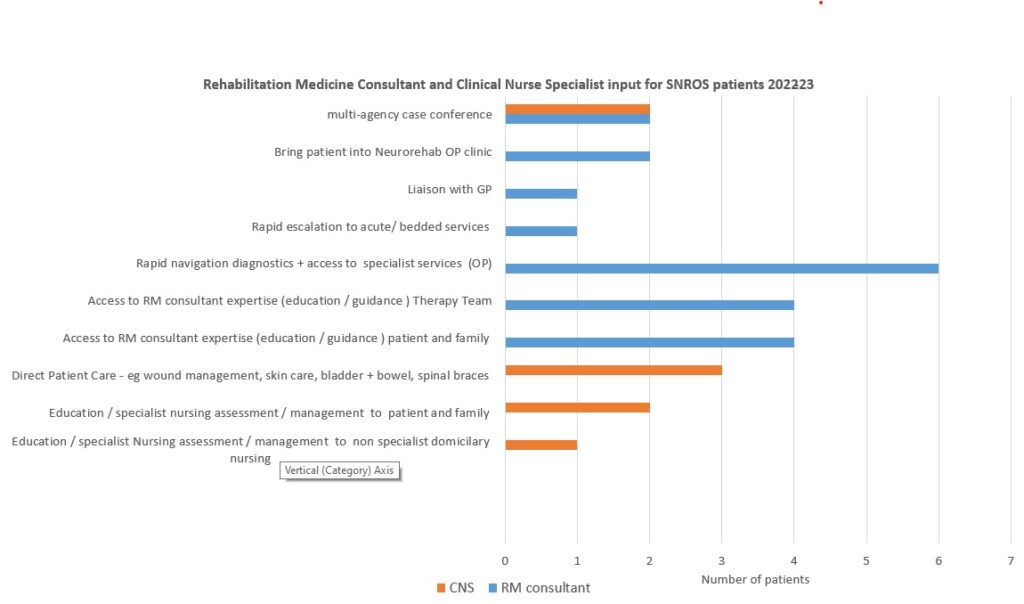
The SNRS service provides intensive level 2 neurorehabilitation through the inpatient beds CNRU and virtual beds in SNROS. The SNROS patients have complex (Category A+B needs) on The Patient Categorisation Tool (PCAT) [11] and have therapists going into their homes to deliver sessions. The SNROS team have a weekly multi-disciplinary team meeting with the Consultant in Rehabilitation Medicine, Clinical Nurse Specialist (CNS) and community therapy team from CLCH. All referrals to SNROS and every patient who is currently on the SNROS pathway is discussed. If there are medical and/or nursing issues arising, the team will consider the following options:
1. Liaise with the GP (e.g. to start medications for neuropathic pain)
2. Liaise with other specialties and diagnostics – Neurology/Neurosurgery/Stroke/Psychiatry/Neuroradiology (e.g. Anti-epileptic medication optimisation)
3. Bring patient into Rehabilitation Medicine Outpatient clinic (e.g. to review spasticity)
4. Arrange home visits (e.g. to review bladder and bowel complications)
5. Rapid escalation to acute/bedded services
There are also in-reach visits from the SNROS team into CNRU for joint sessions to help patients get to know their community therapists. This ensures that a thorough handover takes place and that there is a clear plan for rehabilitation prior to discharge. Referrals to the SNRS service are received through the London-wide referral management system ‘Badgernet’. Outcome measures for both inpatient and virtual beds are collected and submitted to the national database, which collates case episodes for rehabilitation: UK Rehabilitation Outcomes Collaborative (UKROC) [5]. Through the years, there has also been a trend of increasing referrals for stepping up to SNROS beds in patients already in the community. Hence preventing an inpatient rehabilitation admission.
Staffing
NHS staffing trends have shown that it is difficult to recruit to certain disciplines and there is poor retention and high attrition [7]. To help with this, the SNRS service has created rotational posts for physiotherapists, occupational therapists and speech and language therapists through the hospital and community. This variety in exposure has proven to be highly attractive for the retention of staff. In addition, the team becomes familiar with the whole pathway having worked in different sections of it. Other initiatives to educate and empower staff include SNRS networking and educational meetings.
Patient experience
CLCH uses patient stories to gain rich narrative feedback from patients. The following are quotes from patients on the SNROS pathway describing their experience of participating in level 2 specialist neurorehabilitation at home.
John was transferred directly to SNROS from Major trauma having sustained a traumatic brain injury secondary to a fall: ‘in hospital I dunno, not for me. Home was a better environment to do my rehab without a doubt’.
Mary, who sustained a brain injury on holiday and was repatriated back to CNRU to commence goal focused rehab fed back on the seamlessness of transfer between CNRU and SNROS: ‘I was impressed with the care I got. When I got discharged from Charing Cross, they said I would have therapy in the community but I didn’t expect it to be taken up so quickly.’
Benefits and outcomes
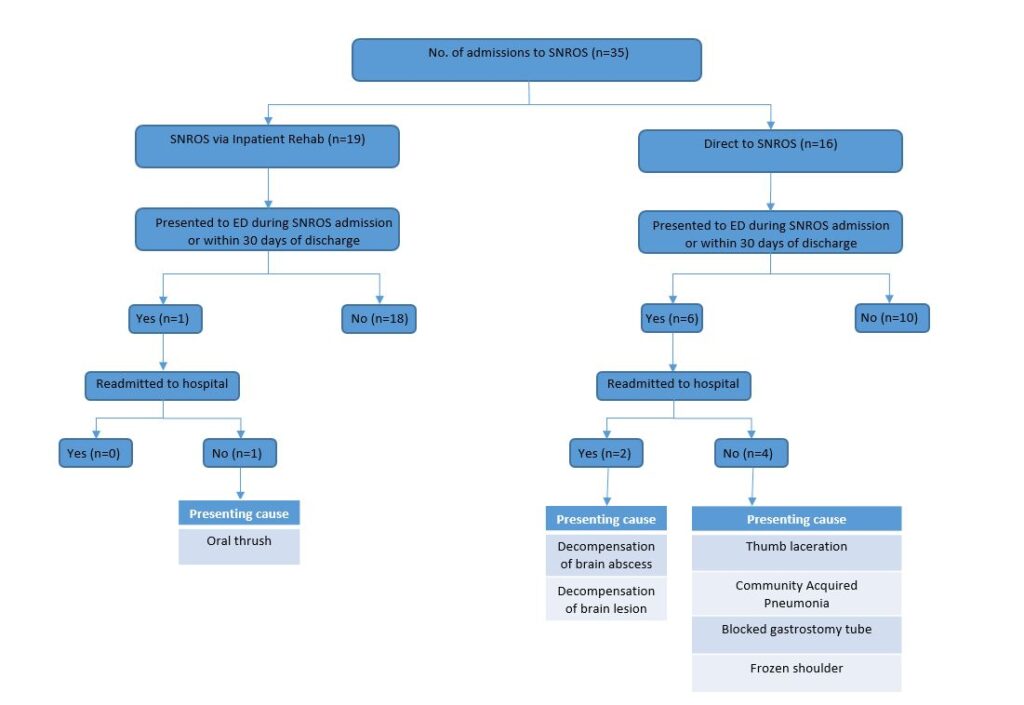
One of the primary outcomes of the SNROS pathway has been reducing Length of Stay (LOS) in inpatient rehabilitation. Data over the last 3 years demonstrates that our inpatient rehabilitation unit (CNRU) has a lower length of stay than the national average and another specialist level 2 unit in the same sector in London (Figure 3). This is largely due to having a seamless SNROS community service that patients can be discharged into.
The Patient Categorisation Tool (PCAT) is a wide-ranging tool for identifying patients with complex (category A and B) needs requiring rehabilitation in a Level 1 or 2 inpatient rehabilitation service [9]. The SNROS patients have a mean PCAT score of 28 which are category B needs [11]. This illustrates moderate complexity in the SNROS pathway comparable with level 2 inpatient neurorehabilitation services. However, complexity scores for patients on SNROS are greater for psychosocial, communication, mental capacity, vocational rehabilitation, rather than domains associated with medical risk and acuity.
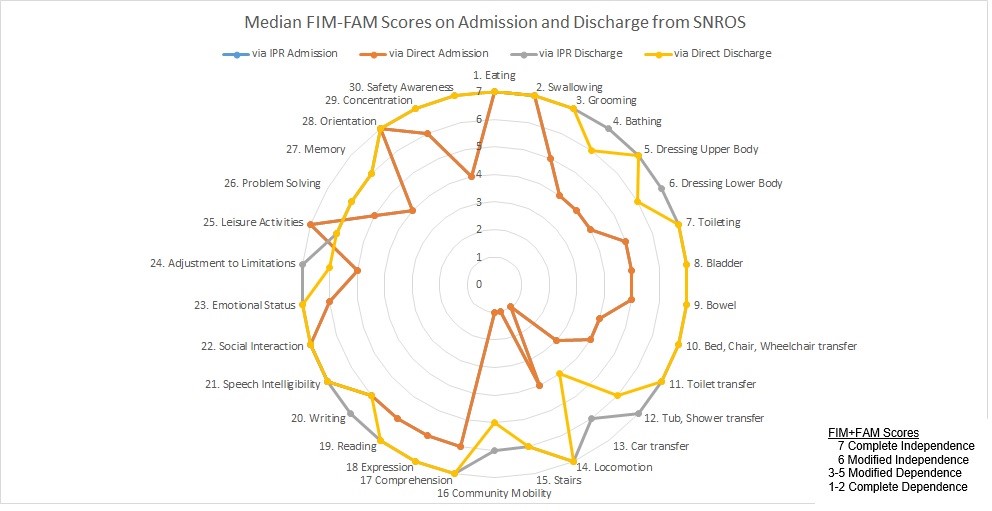
Figure 5 (below) demonstrates that on admission to SNROS; the patients have the same level of functional dependence regardless of whether they are admitted via an inpatient level 2 rehabilitation service or directly from an acute ward. On the diagram this is shown by dark orange (admitted from acute ward) being directly on top of blue (admitted from level 2 unit) as the admission scores for both groups were the same (hence only the dark orange line is visible). On discharge from SNROS patients made functional improvements across all domains with the majority achieving either scores of 6 or 7 (i.e. modified or complete independence), suggesting that the SNROS pathway is both supporting earlier discharge from bedded services and delivering the functional benefits expected from a high-intensity neurorehabilitation service.


Summary
A model and pathway for home-based care which enables rapid step down from bedded acute and rehabilitation services for people with complex (category A and B) neurological rehabilitation needs, has been developed and tested within this specialist neurorehabilitation service. By creating SNROS and integrating it with the inpatient bedded service; we have demonstrated the ability to streamline transitions of care and deliver intensive therapy, similar to that provided within an inpatient unit, at home. With access to skilled community therapy teams, Consultant in Rehabilitation Medicine assessments/reviews, monitoring and Clinical Nurse specialist (CNS) support, the outcomes for rehabilitation in the patient’s own home are comparable to bedded units for this subset of patients with complex neurological needs.
We would advocate for enhancing integrated specialist neurorehabilitation services with both acute and community teams to provide a flexible and responsive service for our patients who require neurological rehabilitation. This model is aligned with strategic objectives within the ICS, reducing demand on bedded services and increasing integration between services while providing access to specialist care.
References
- NHS England and NHS Improvement (NHSE/I) 2022/23 operational planning guidance
- National Neuro Advisory Group Impact Report 2019
- “Neuro Numbers 2019” – A report by the Neurological Alliance – March 2019
- British Society of Physical and Rehabilitation Medicine (BSPRM) Specialist neuro-rehabilitation services: providing for patients with complex rehabilitation needs 2010 (latest update May 2023)
- UK Rehabilitation Outcomes Collaborative – http://www.ukroc.org
- NHS England Digital 3.2 Emergency readmissions within 30 days of discharge from hospital – Specification version 1.4 March 2020.
- A critical moment: NHS staffing trends, retention and attrition 2019. The Health Foundation 2019
- Nayar M, Vanderstay R, Siegert RJ, Turner-Stokes L. The UK Functional Assessment Measure (UK FIM+FAM): Psychometric Evaluation in Patients Undergoing Specialist Rehabilitation following a Stroke from the National UK Clinical Dataset. PLoS One. 2016 Jan 29;11(1):e0147288. PMID: 26824696; PMCID: PMC4732596. https://doi.org/10.1371/journal.pone.0147288
- https://www.england.nhs.uk/virtual-wards/what-is-a-virtual-ward/
- A new community rehabilitation and reablement model Good practice guidance for integrated care boards (commissioners and providers NHS England September 2023
- Siegert RJ, Medvedev O, Turner-Stokes L. Dimensionality and scaling properties of the Patient Categorisation Tool in patients with complex rehabilitation needs following acquired brain injury. J Rehabil Med. 2018 May 8;50(5):435-443. PMID: 29582901. https://doi.org/10.2340/16501977-2327





