Abstract
Neurological conditions frequently affect hand activity impacting on independence in carrying out everyday tasks. Splinting is frequently completed in neurological rehabilitation to promote incorporation of the affected hand into everyday tasks and to prevent disability. Here we consider the evidence base, clinical reasoning, and application for functional splinting.
Key Points
- Functional Splinting is used to allow people with a neurological condition to successfully engage the affected upper limb in occupation [1].
- Functional splinting helps with either restoring impaired ability or compensating for lost activity.
- Analysis of activity and movement is central to the clinical reasoning that guides appropriate use of functional splinting
- Although there is limited research in the use of functional splinting, this must be balanced against the individual’s positive experience of goal attainment and re-engagement in activities of daily living.
Introduction
Our skill as therapists working with people with neurological conditions is in analysing activity to identify the underlying impairments that are preventing or limiting independence in everyday activities. One of the practical strategies to improve the use of hands within tasks is splinting. Splinting is defined as ‘the application of external devices designed to apply, distribute or remove forces to or from the body in a controlled manner, to perform one or both functions of control of body motion and alteration or prevention in the shape of the body tissue’ [2].
Three main aims of splinting in neurological conditions are: (i) to prevent and/or correct contractures (resting splints); (ii) to improve performance in training or exercise (exercise splints) for example, using a splint to block Metacarpophalangeal (MCP) joint extension to allow strengthening of lumbricals or a dynamic exercise splint e.g. saebo glove [3] and saebo flex [4] to strengthen extensors and lumbricals; (iii) enabling participation or optimising performance in a functional task such as eating, typing, writing (functional splints).
In this article, we focus on functional splinting since there is so little empircal evidence published on this topic. Available published expert opinion [1] states that the use of functional splints in clinical practice aim to address deficits in the activity and participation domains of the International Classification of Functioning, Disability and Health [5].
Approaches guiding functional splinting
Rehabilitation of the upper limb may adopt a restorative or a compensatory approach to achieve participation in an UL based task. The motor impairments associated with Upper Motor Neurone (UMN) syndromes are often described in terms of positive (e.g. spasticity) and negative (e.g. weakness or loss of dexterity). However, overall UL function is negatively affected by the interplay of the motor, sensorimotor and/or motor planning impairments e.g apraxia all of which contribute difficulty in fine motor dexterity in tasks e.g hand writing, feeding and dressing [6]. Restoration uses the principles of neuroplasticity and motor relearning to optimise motor recovery and enable engagement in upper limb tasks [7]. Functional splinting can be used to help achieve restoration by using the affected limb within tasks and increasing dose of repetition through non-compensatory movement training outside of therapy sessions. For example in early stroke rehabilitation, functional splints can provide support to allow an effective pinch. By making the hand useful within a task such as handwriting or typing, the muscles of the shoulder and the arm may then also be employed within the task. Without the splint, the person may use compensatory movements or in our clinical experience, may not use the arm at all. The strength and control of the upper arm may improve with repetition of desired movement patterns and this proximal stability and control of the shoulder has subsequent benefits in allowing the hand to move in a more controlled manner to engage in tasks.
A compensatory approach accepts that restoration (at impairment level) may not be possible but increased engagement in activity can be achieved. For example, early in progressive neuromuscular conditions encouraging typical grip patterns aims to delay over reliance on the stronger but functionally less efficient extrinsic hand muscles and encourages continued use of the intrinsic hand muscles within activities [8]. Where the negative features of UMN syndrome present [9], such as weakness, functional splinting can be used to compensate for weak muscles and joint instability, e.g. blocking thumb abduction and supporting opposition for an effective pinch grip.
In either approach, functional splints can reduce the amount of external physical and verbal guidance required whilst the arm is used in a meaningful task. This approach is less effort for the patient, increasing the opportunity for varied independent practice, which in turn can lead to more efficient, less compensatory, movement patterns and task mastery. Overall, the intention is that patients can engage in independent practice leading to a higher dose of training.
Evidence for functional splinting
Despite scarce research into the use of functional splinting in adult neurological conditions, it is a reasonably widely used intervention. In a 2013 survey of splinting practice of 420 UK therapists, 51% said they would splint to improve activities of daily living [10]. However, in a review of splinting practice in a rehab unit over a 2 year period, it was reported that less than 5% were functional splints, in comparison to resting splint [1]. In people with neuromuscular conditions and spinal cord injury, several case reports describe improved hand activity where functional splints were customised to both individual impairments and the specific task [11-13]. In spinal cord injury, case reports focus on the use of wrist driven orthoses to support a tendinosis grip to improve pinch grip in tasks. Success appears to be dependent on a specific level of injury and muscle power in the wrist and thumb [14,15].
Lycra has become a material of interest in splinting the paediatric population to achieve increased participation in daily activities [16]. The areas of high pressure provided by the tight fit of the lycra garment are intended to increase sensory and proprioceptive awareness, and produce a mechanical compressive effect [17]. The benefits depend on ensuring that the targeted area of the body is positioned to promote effective movement and function, which requires customised fitting [18]. For children with cerebral palsy and adults with stroke [14] improvements in efficient movement and task performance have been reported when using Lycra arm garments in combination with goal directed training [19].
While splinting can improve upper limb activity, one potential side effect is increased movement of other joints. In one study of 20 healthy participants, immobilising the wrist led to increased compensatory movements of the shoulder during a feeding activity [20]. In patients with compromised muscle control, compensatory movement of other muscle groups would have already occured due to impairments, thus the clinician needs to consider balancing a compromised movement pattern with facilitating functional use of the arm [1].
Clinical reasoning and assessment
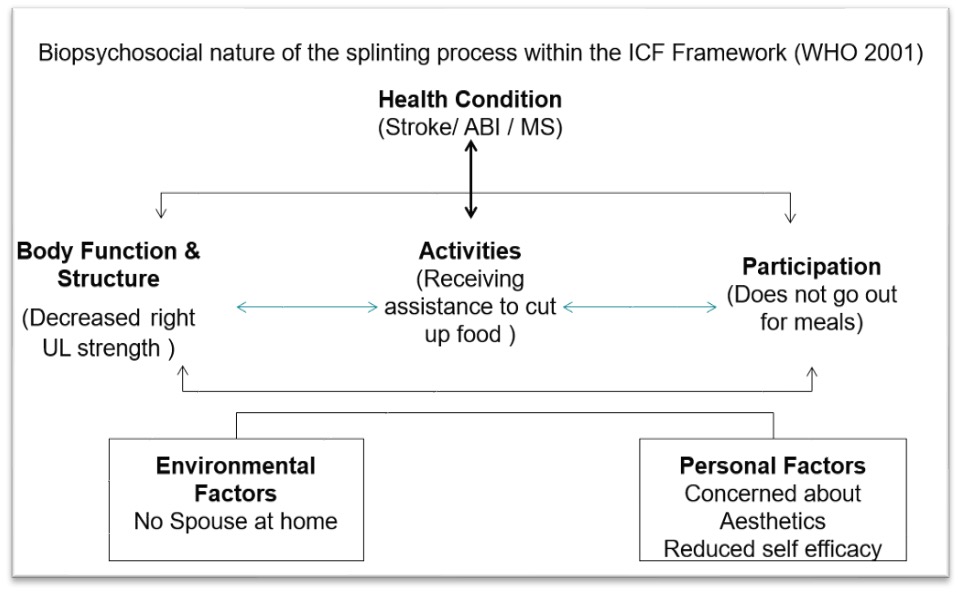
As therapists, we are constantly thinking about how we can help our patients ‘keep their hand in the game’. In the absence of relevant published research concerning functional splinting, we must use our clinical reasoning to decide whether it will help within a comprehensive goal-directed rehabilitation programme. A biopsychosocial framework, such as the International Classification of Functioning, Disability and Health [5] (Figure 1), supports clinical reasoning to:
- Establish the meaningful activities that the person wants, needs, or must participate in. This provides a focus for goal setting and intervention, e.g., a patient needs to be able to cut food in order to feed themselves.
- Analyse all the impairments (body function and structure) that are influencing movement patterns and preventing both activities and participation e.g., patterns of weakness, spasticity, loss of joint range, shoulder restriction and pain, sensory loss, apraxia [1].
- Analyse task performance and establish the movement errors providing a focus for the intervention. It is essential to know how the hand would routinely perform functional tasks along with the required grasp and pinch grip, e.g., unable to hold a knife in a way that allows cutting of food. In Acquired Brain injury, a formal tool that provides a structured manner for this process is Upper Limb Performance Analysis [6].
- Understand the environmental and personal factors that influence a person’s performance of activities, e.g., someone who lives alone so has no one to help cut their food.
- Clinically reason how a splint may be used to promote the appropriate movement pattern required to achieve the task, e.g., design a splint to allow the hand to correctly grip a knife to cut food and compensate for reduced hand strength.
Functional Splinting Intervention
The purpose of the functional splint and the individual’s level of impairment will guide the design and choice of materials. Splints can be made from several different materials that provide a range of support to single or multiple joints. Static splints immobilise joints and are typically made from thermoplastic material, while dynamic splints provide a supportive force but allow movement, for example, lycra, neoprene and taping. We use the information from movement analysis together with client centred goals to design individual functional splints, keeping in mind these five principles:
- Promoting and supporting functional patterns of grip (Figure 2).
- Stabilising where there is weakness (Figure 3).
- Improving patterns of movement to increase efficiency (Figures 4 & 5).
- Enabling independent practice (Figures 6 & 7)
- Increasing intensity of self-directed practice (Figures 8 & 9)
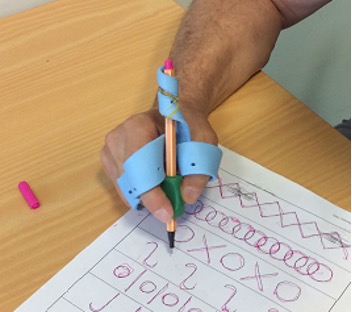







Figure 4 demonstrates how splinting can be used to improve efficiency of movement. The individual’s goal was to use a fork: a functional splint supports extension of the index finger with a dynamic strap around finger and fork, enabling him to hold it. He struggles to maintain adequate pronation, compensating through trunk lateral flexion and shoulder abduction and elevation. In Figure 5, a neoprene pronation strap has been introduced, anchored to a thumb spica which stabilises the wrist. This re-directs the pull of the supinators, altering the pattern of movement and allowing the hand to engage in the functional task. Independent repetitive task practice is therefore of a higher quality movement, with less trunk compensations.
Figure 6: The cutlery splint is custom made from thermoplastic and plastazote tubing to hold the hand in the correct position to cut food and independently feed. This was combined with a prefabricated wrist support to stabilise the wrist during task. Figure 7: The hand splint allows extension of MCP, PIP and DIP joints to allow flat hand placement during daily prayer.
Challenges and future priorities
The literature reports that upper limb splints may be abandoned by patients however individualised splinting has been demonstrated to lead to continued use of splints over a 4 week period [21]. Factors contributing to this are discomfort, pain, usefulness, ease of use and splint selection that has a clear link to the patient’s goals. It cannot be overemphasised how important clinical reasoning and education are in improving patient adherence and determining the success of a functional splint. The provision of the splint should not be a one off event and follow up is equally important. In restorative treatment, monitoring progress and removing levels of support are essential. In compensatory treatment, ongoing review is paramount for monitoring progression as motor skills worsen, requiring increased support over time.
Published research demonstrating a lack of evidence for static splinting overnight in early stroke to avoid contracture [22] has sometimes been mis-interpreted leading to the belief that all splinting in clinical practice should be discouraged. Therapists themselves have identified a lack of training in undergraduate programmes and limited access to training in the workplace [10] which may account for reduced application of splinting clinically. Consequently, many therapists have lost confidence and competence in this area, and service provision of splinting for neurological conditions has, in our experience, been dramatically eroded.
There is an urgent need for improved training and education for clinicians. Whilst it is important that there is research into the effectiveness of functional splinting in different clinical situations, it is equally important that the design of future studies and clinical trials asks appropriate questions and use appropriate outcome measures. In the meantime, clinicians should consider splinting for function as an intervention that successfully engages the hand in occupation within a goal orientated recovery programme.
References
- Copley, J, Kuipers K. (2014) Neurorehabilitation of the Upper Limb across the Lifespan. West Sussex John Wiley & Sons Ltd.
- Rose G (1986) Orthotics, principles and practice. London: Heinemann.
- Wong Y, Ada L, Månum G, et al. Upper limb practice with a dynamic hand orthosis to improve arm and hand function in people after stroke: a feasibility study. Pilot Feasibility Stud 9, 132 (2023). https://doi. org/10.1186/s40814-023-01353-8
- Lannin NA, Cusick A, Hills C, Kinnear B, Vogel K, Matthews K, Bowring G. Upper limb motor training using a Saebo™ orthosis is feasible for increasing taskspecific practice in hospital after stroke. Aust Occup Ther J. 2016;63(6):364-372. Epub 2016 Sep 19. PMID: 27646624.
- World Health Organization. (2001). International classification of functioning, disability and health: ICF. World Health Organization
- Holman Barden HL, Baguley IJ, Nott MT, Heard R, Chapparo C. Measuring task performance after acquired brain injury: Construct and concurrent validity of ‘Upper Limb Performance Analysis’, Brain Injury 2015;29(10):1223-1231.
- Kleim JA, Jones TA. Principles of Experience Dependent Neural Plasticity: Implications for Rehabilitation After Brain Damage. Journal of Speech, Language, and Hearing Research. 2008;51: 225-239
- Ramdharry, G., Bull, K., Jeffcott,R., and Frame, A. An expert opinion: Rehabilitation options for people with polyneuropathy ACNR May 2020 https://doi. org/10.47795/EUNI7797
- Li S, Francisco GE, Rymer WZ. A New Definition of Poststroke Spasticity and the Interference of Spasticity With Motor Recovery From Acute to Chronic Stages. Neurorehabil Neural Repair. 2021 Jul;35(7):601-610. doi: 10.1177/15459683211011214. Epub 2021 May 12. PMID: 33978513.
- Kilbride, C. Hoffman K., Tuckey J., Baird, T. Marston, L. & Souza,L. Contemporary splinting practice in the UK for adults with neurological dysfunction: A cross-sectional survey International journal of therapy and rehabilitation. 2013;20:559-566 https://doi.org/10.12968/ ijtr.2013.20.11.559
- Videler A, Eijffnger E, Nollet F, Beelen A. (2012). A Thumb Opposition Splint to Improve Manual Dexterity and Upper-Limb Functioning in Charcot-Marie-Tooth Disease. Journal of Rehabilitation Medicine: Official Journal of the UEMS European Board of Physical and Rehabilitation Medicine. 44(3):249-253. https://doi. org/10.2340/16501977-0932
- Tanaka K, Horaiya, Akagi J and Kihoin N. (2014). Timely manner application of handorthosis to patients with amyotrophic lateral sclerosis: a case report. Prosthetics and orthotics international. 38(3):239-242 https://doi. org/10.1177/0309364613489334
- Ivy C, Smith S & Materi. Upper extremity orthoses use in Amyotrophic Lateral Sclerosis/ Motor Neuron Disease: Three Case Reports. American Association for Hand Surgery. 2014;9:543-550. https://doi.org/10.1007/ s11552-014-9626-x
- King M, Verkaaik J, Nicholls A, Collins F. A wrist extension operated lateral key grip orthosis for people with tetraplegia. Technology & disability. 2009;21:19-23. https://doi.org/10.3233/TAD-2009-0267
- Portnova A, Mukherjee G, Peters K, Yamane A, Steele K. (2018) Design of a 3D-printed, open-source wrist driven orthosis for individuals with spinal cord injury. PLoS ONE 13 (2): e0193106. https://doi.org/10.1371/ journal.pone.0193106
- Attard J. Rithalia S. A review of the use of lycra pressure orthoses for children with cerebral palsy. International Journal of Therapy and Rehabilitation. 2004;11:120-126. https://doi.org/10.12968/ ijtr.2004.11.3.13384
- Buchanan, K, Hourihan S. (2016) Physical and Postural management of Spasticity, in Stevenson, VL. and Jarrett, L., (eds) Spasticity management; A Practical Multidisciplinary Guide (2nd ed), Boca Raton, CRC Press. https://doi.org/10.1201/b21452-4
- Morris J, John A, Wedderburn L. Rauchhaus P & Donnan P. Dynamic Lycra® orthoses as an adjunct to arm rehabilitation after stroke: a single-blind, two- arm parallel group, randomized controlled feasibility trial. Clinical Rehabilitation. 2019;33(8):1331-1343 https:// doi.org/10.1177/0269215519840403
- Elliott CM, Reid SL, Alderson JA, Elliott BC. 2011. Lycra® arms splints in conjunction with goal-directed training can improve movement in children with cerebral palsy. Neurorehabilitation. 2011;28(1):47-54. https://doi.org/10.3233/NRE-2011-0631
- May-Lisowski TL, King PM. Effect of wearing a static wrist orthosis on shoulder movement during feeding. American Journal of Occupational Therapy. 2008;62:438-445. https://doi.org/10.5014/ajot.62.4.438
- Kuipers K et al. (2009) Do clients with acquired brain injury use the splints prescribed by occupational therapists? A descriptive study. NeuroRehabilitation. 2009;24:365-375. https://doi.org/10.3233/NRE-2009-0491
- Lannin NA, Cusick A, Mucluskey A, Robert D, Herbert. Effects of Splinting on wrist contracture after stroke. A randomised control trial. Stroke 2007;38:111-116 https://doi.org/10.1161/01.STR.0000251722.77088.12


