The third annual Parkinson’s Review Meeting (PRM) was held at the Academy of Medical Sciences in Portland Place, London and was supported by an unrestricted grant from Genus Pharmaceuticals Ltd. Discussions were chaired by Professor Kailash Bhatia, Professor of Clinical Neurology at UCL and Honorary Consultant Neurologist at London’s National Hospital for Neurology & Neurosurgery. The opinions expressed in this article are not necessarily those of the publisher or Genus Pharmaceuticals
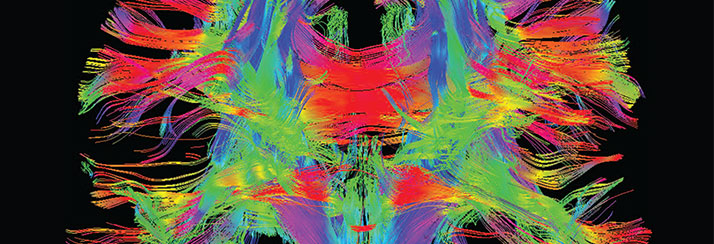
The meeting was opened by Dr Thomas Foltynie, Consultant Neurologist and Senior Lecturer at the National Hospital for Neurology & Neurosurgery. To deliver optimal care, quality standards should ensure that each Parkinson’s patient has access to a PD specialist and specialist nurse alongside a multidisciplinary team (MDT) and non-drug treatments. There are a number of options available when patients’ Parkinson’s cannot be controlled on oral therapies alone. APO-go is indicated in patients whose disease is not sufficiently controlled by oral anti-Parkinson medication. Other advanced treatments are available: apomorphine infusion via pump, Deep Brain Stimulation (DBS) and levodopa intestinal gel. Mode of administration is also a factor as apomorphine can be given as intermittent injections or as a continuous subcutaneous pump infusion and DBS can target different areas of the brain.
Dr Jon Stamford (Scientific & Advocate Communication Coordinator for the Cure Parkinson’s Trust) and Brian Corbin gave frank and rather moving accounts of their patient experience as sufferers of PD. Jon explained how NMS had affected his quality of life, but agreed that no two patients were symptomatically alike making a ‘one size fits all’ treatment algorithm unfeasible. Brian explained how personalised treatment has allowed him to return to work, in particular the huge support provided by his PD nurse specialist. “All PD patients have the right to a specialist nurse”, he added.
Professor K Ray Chaudhuri, Consultant Neurologist and Professor in Neurology/Movement Disorders at King’s College Hospital NHS Foundation Trust, then spoke about how motor and non-motor symptoms (NMS) of PD cause poor quality of life for patients and their caregivers, yet NMS tend to be under-recognised and under-treated. Khoo et al.1 studied the frequency of NMS in a newly diagnosed PD patient cohort and found that symptoms such as impairment of olfaction, REM loss of atonia, REM sleep behaviour disorder (RBD), constipation, depression, colour vision effects, pain and excessive daytime sleepiness (EDS), were common, reflecting the multi-system nature of the disorder.
Newly released results from the AM IMPAKT2 study described the effect of apomorphine s.c. injection in PD patients with (the often under-recognised) morning akinesia resulting from delayed or unreliable onset of effect of their first morning dose of levodopa. By circumventing the oral route, apomorphine s.c. injection provided rapid and reliable turning-ON for patients with morning akinesia, reducing time-to-on by an average of 40 minutes. Professor Chaudhuri’s presentation closed with an emphasis on how as well as motor-related symptoms, NMS and multi-morbid conditions can be a significant burden for Parkinson’s patients.
Seema Buckley, Chief Pharmacist at NHS Kingston Clinical Commissioning Group (CCG) discussed the payer perspective and how any commissioned PD services need to innovate to improve quality whilst reducing cost. This comes in the wake of July’s NHS call to action requesting CCGs make further savings of £30billion on top of Sir David Nicholson’s QIPP efficiency savings challenge. NHS England will implement consistent national policies, but the CCGs may allow for variability based on local health needs.
The next speaker, presenting the business manager’s perspective for coding the PD pathway using the best practice tariff was Alexa Coombes, Neurology Business Manager for UCL Hospitals NHS Trust. Historically, the system was made based on Healthcare Resource Group (HRG) codes, which does not always reflect pathways or specialist centres and leaves little scope for innovation. Alexa explained that system revisions had assigned a cost per patient episode based on bed-days, consumables, medical/nursing or scientific staff time, radiology and diagnostics and consequently, adjusted HRG codes for many specialist areas have been introduced. The new integrated commissioning framework splits care into a multi-tiered generic service model (involving local community and primary care, MDT specialist outreach clinics and specialist care hubs to undertake a full range of neurology-related procedures).
Charles Rendell, London Regional Commissioning Advisor at Neurological Commissioning Support (NCS) outlined some of the new organisations within the NHS including 12 Strategic Clinical Networks (SCNs) and Clinical Senates. The new networks are: cancer; cardiovascular including renal, diabetes and stroke; maternity, children and young people; and, mental health, dementia and neurological conditions (as lobbied for by NCS). SCNs could be key for improving neurology services and Charles urged participants to build their awareness of local activities within their SCN and take an active lead in commissioning decisions.
Professor Chaudhuri spoke about setting up a complex Parkinson’s referral service. In Professor Chaudhuri’s Trust they have used the 2011 Parkinson’s Audit from Parkinson’s UK as a benchmark when designing their referral service. Professor Chaudhuri thought that despite a genuine need to iron out national quality differences, ideally there should be nominated centres of excellence for PD and devolved areas which refer to these centres. To facilitate this type of hub-and.spoke model would require the involvement of GPSIs in neurology and Parkinson’s Specialist Nurses and collaboration between Parkinson’s services and geriatric care would benefit referral services.
Allan Karr, Pharmacy Business Manager of UCLH and Chairman of the National Homecare Medicines Committee outlined how homecare can support PD patient outcomes. For patients homecare can mean increased choice, reduced waiting times, travel and hence increased convenience. Homecare currently covers a multitude of therapeutic areas including PD where apomorphine is regularly supplied by homecare.
The PRM included frequent audience and panel questions and keypad voting and it was very encouraging to hear such passionate opinions and valuable knowledge and experience being shared. For further information on the day’s talks and outcomes or if you would like to know more about other PRM events taking place throughout the UK, please contact prm@genuspharma.com.
References
- Khoo TK Yarnall AJ, Duncan GW, et al. The spectrum of nonmotor symptoms in early Parkinson disease. Neurology 2013; 80: 276-281
- For study information see: http://www.acnr.co.uk/2013/05/news.review-6/ (last accessed;:23 October 2013) APO-1013-1934 Date of preparation: October 2013
ACNR2013;13:6:34. Online 3/1/14