
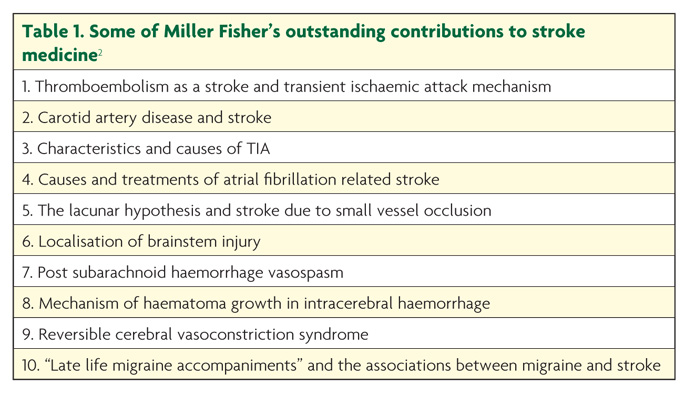
Dr Charles Miller Fisher (December 5, 1913 – April 14, 2012) developed and wrote about the key scientific ideas that underpin almost every aspect of modern stroke medicine. His insatiable curiosity and formidable scientific ability were applied to meticulously describe clinical and pathological features of many types of stroke. A major theme that Dr Fisher developed can be summed up as the idea that: “strokes do not occur at random”, but instead follow characteristic patterns according to their cause and mechanism. He authored more than 200 publications detailing his observations.1 Some of the most significant discoveries are listed in Table 1. Every stroke clinician will immediately recognise the impact these have had on both our conceptual understanding and daily clinical practice.2 A single stroke unit ward round today might include the recognition of lacunar stroke syndromes, the urgent recognition and treatment of symptomatic carotid artery thrombo-embolism, and the diagnosis of a “late life migraine accompaniment” mimicking stroke or transient ischaemic attack (TIA).
Life before becoming a physician held great challenges for Miller Fisher, which may have shaped his extraordinarily determined and productive career in stroke medicine. He was born in 1913 in Ontario, into a large family of eight siblings, and then studied medicine in Toronto, where he was awarded his degree in 1938. He joined the British Royal Navy at the outbreak of war and spent three and a half years interred in a German Prisoner of War Camp, after his boat, HMS Voltaire, was sunk off the coast of Cape Verde. He spent nine hours in the sea, waiting to be rescued, on the very day his wife was due to give birth to their first child, and – in typically uncomplaining manner – reportedly said: “I thought perhaps she was in more trouble than I was”. He trained as a neuropathologist in Boston, and then returned to Montreal, where he began to define what he called “transient ischaemic attacks”. In perhaps his most famous observation, he repeatedly noted “premonitory fleeting symptoms” (including limb sensory symptoms, and monocular visual loss) experienced by patients prior to a hemispheric ischaemic stroke, and made the crucial link to carotid artery atheromatous disease. This led to wide acceptance of the thrombo-embolic theory of ischaemic stroke and TIA. He then moved to Massachusetts General Hospital in the 1950s where he had a long and highly productive career, in the process creating the first stroke service. He died at the age of 98, in 2012, leaving two sons and a daughter.1,3
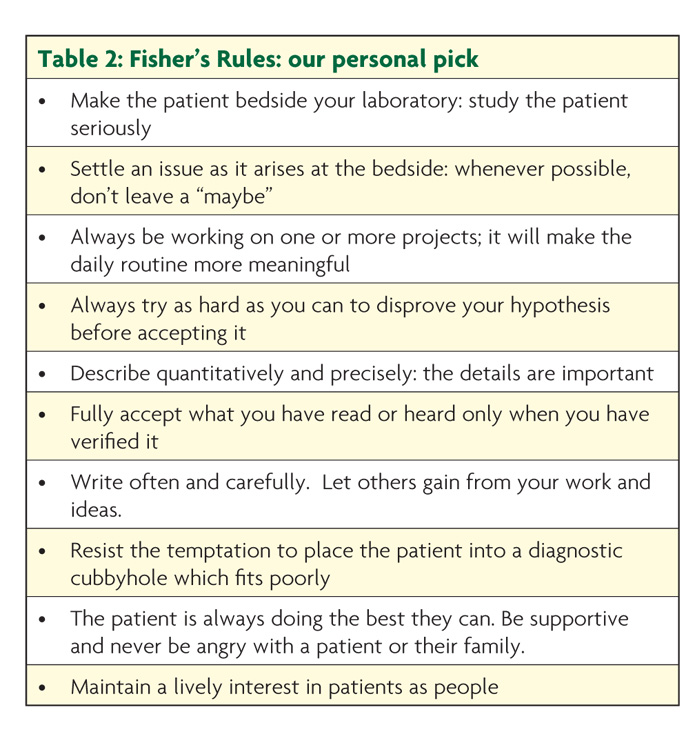
Miller Fisher thrived on the intellectual challenge of clinical practice and became legendary for his dedicated care and teaching, which inspired generations of physicians who trained with him. Louis Caplan, one of his clinical fellows, captured this approach in “Fisher’s Rules”, which remain a blueprint for becoming a great stroke clinician and scientist. We have listed our personal pick, but urge you to read the full publication in order to better understand the attitudes and values he promoted (Table 2).4
Miller Fisher’s ideal of lifelong learning through detailed observation was uniquely coupled with tremendous communication skills and empathy for the plight of patients affected by stroke. Descriptions abound of Miller Fisher in his office poring through his copious notes to correlate clinical observations with pathological findings. After his death his colleagues carefully collected these notes: one trainee doctor reportedly even checked through the bins to retrieve some that were accidentally disposed of!
One of the greatest lessons we can take from Miller Fisher’s life is that he made every day’s work an opportunity to make an observation or original contribution. “If you could describe that,” he would tell the attendees of his weekly case conference, “if you could really describe that patient’s findings and disease mechanism carefully and accurately, you would be the first to do so.” While evidence based medicine in large populations is key to modern neurological practice (and especially to stroke medicine), Miller Fisher reminds us of the power of detailed narrative observations on the symptoms of disease and its impact in the individual patient. This is the way in which new patterns and mechanisms of disease are recognised, and by which the correct treatment for each patient can be determined through logical principles. Dr Miller Fisher (or CMF, to those who knew him) continued ward rounds until he was almost 90 years old, always asking the question “what can the patient teach us?” – a lesson which we would all do well to remember, even in this era of ever more sophisticated investigative techniques.
Read the ACNR article written by Dr Miller Fisher in 2005, where he talks about the discovery of the syndrome which bears his name.
References
- Mohr JP, Caplan LR, Kistler JP. In Memoriam: C Miller Fisher. Stroke 2012;43:1739-40.
- Greenberg SM. C Miller Fisher: An Appreciation. Stroke 2013;44:171-2.
- Caplan LR, Mohr JP, Ackerman RH. In Memoriam: Charles Miller Fisher (1913-2012). Arch Neurol. 2012;69(9):1208-9. doi:10.1001/archneurol.2012.1743.
- Caplan LR. Fishers Rules. Archives of Neurology. 1982;39:389-90.


