“The hospital should ask its doctors which meetings they want funding to attend. And then they should let the doctors know they can have the full amount of money requested. But . ?”
This is a personal account of new ideas and facts that I acquired in five hours at an exciting and excellent meeting where I also met many friends and colleagues who added, greatly, both to enjoyment and to learning.
The most striking outcome for me was a realisation that, although I read all articles submitted to Clinical Rehabilitation, I search regularly in relation to a book on rehabilitation, and I have been interested in most aspects of rehabilitation for 37 years, nonetheless I learned about major and important ideas and developments that I had absolutely not heard about. How can this happen?
Generally I, like most people, go to meetings which focus on areas that I am particularly interested in, and may even be expert in. I obviously meet others with similar interests, many are also friends. We may learn a few small facts, but generally we all know what each of us is doing, and we all read much the same material. It is a very comfortable experience, reassuring me that what I know or think is correct, and maybe introducing a further new fact or idea entirely within an existing model or framework.
Further, employers have a narrow view on continuing professional development. They ignore the third and most important word, DEVELOPMENT. Instead they focus on increasing targeted knowledge and skills. Employers are then surprised, when trying to alter or improve services, that staff do not come up with any particularly new ideas. They then spend a fortune on external advisors who know nothing, except how to charge large sums to suggest either obvious or inappropriate and/or impossible ideas.
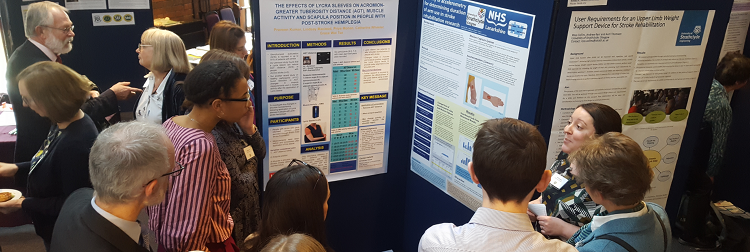
The reason this meeting was so full of new and different ideas for me, and I think it was for most people, was precisely because most of us were outside our comfort zone for most of the time. Of course there was an underlying general interest in rehabilitation but the range of different professions and the range of different healthcare and non-healthcare specialities represented was large. There was always someone to ask the awkward but insightful question, and someone else to give an alternative valid answer.
The next part of the initial quotation was:
“But you are not allowed to use any of it on any of the meetings you requested!”
Though the quotation is not verbatim, it was the message given by David Sacket speaking at the Radcliffe Infirmary about 20 years ago. He emphasised the great importance of and benefits that arise from going to meeting well outside your own small area of interest.
Content of five main presentations
A personal view
Nicola Walsh started her talk considering evidence for effective therapies for people with knee osteo-arthritis, which concluded that exercise and changing behaviour were both important. Most importantly, she then broadened her view to encompass (a) other similar disorders and (b) practical considerations, especially affordability. She concluded that the role of a rehabilitation team was to diagnose correctly (understand what was wrong, and what could be done), and then to refer to non-health, ‘normal’ community resources where exercise professionals with training in behavioural change strategies would help the person learn to exercise as part of normal life.
Candy McCabe illustrated the principle of (a) gaining a proper understanding and (b) using this to design an approach for the patient to use with (c) education of the patient; her chosen population was people with complex regional pain syndrome. She showed how normal pain mechanisms, essential to protect us from harm, can become distorted (why is unknown), becoming excessively vigilant and responsive to at least some aspects of the threat. This distorts perception of bodily parts and bodily function. A treatment approach based on this analysis, using virtual reality and many other techniques works; analgesia is spectacularly unsuccessful.
Garth Johnson spoke about bioengineering in rehabilitation. Completely unexpectedly (to me), he highlighted the role that bioengineers and a bioengineering approach have in analysing and understanding any disorder of movement, from joint arthritis to disordered motor control after stroke. The outcome of understanding joint function has been demonstrated in the development of increasingly complex, and successful joint replacement. However the emphasis was on neurologically disordered motor control, and he showed how bioengineering data could answer questions that neurophysiological investigation could not.
Roshan dasNair took a different approach – his interest was in rehabilitation for cognitive deficits, specifically memory problems in people with multiple sclerosis. He started by disabusing us of the belief that systematic reviews were necessarily a sound evidence base, revealing that a widely quoted systematic review that concluded that there is good evidence that cognitive rehabilitation helps people with memory deficits. A critical review (by another group) showed that there was in fact no evidence to support the conclusion. He then told us about his (to be published soon) large trial, which had not found evidence of benefit across a range of outcomes.
Carolyn Young, the last speaker, also talked about multiple sclerosis. She started with a question – how many of us had heard of or knew about the TONiC study? Very few, if any. Yet it has recruited 25% of all patients with motor neurone disease (MND) in England, and over 7,000 people with multiple sclerosis (MS) from England. It is the ‘Trajectories of Outcomes in Neurological Conditions (TONiC) study’ and has permission to study not only MS and MND but also traumatic brain injury and neuro-muscular condition. She also told us about the Wilson and Cleary ‘conceptual model of patient outcomes’, based on the biopsychosocial model. Watch the TONiC study; it will potentially help rehabilitation greatly. tonic.thewaltoncentre.nhs.uk