After attending the MasterClass and being tasked with producing a project encompassing aspects of Parkinons patient care, we endeavoured to create a project relevant to our particular patient cohort. As a newly appointed Consultant Geriatrician, and SpR with a specialist interest in orthogeriatrics and movement disorders, we found a lot of scope for quality improvement in management of bone health.
Parkinson’s disease (PD) is being increasingly recognised as an independent risk factor for osteoporosis and fragility fractures. There is a two-fold risk of hip fracture for men with PD and three-fold for women. Those with Parkinson’s present earlier in morbidity trajectory, with hip fracture than non-PD counterparts. The median time to hip fracture calculated as four years from diagnosis. Vitamin D deficiency is common in these patients1. Osteoporosis pathophysiology is proposed to be multifactorial in nature, contributory factors being reduced activity, sarcopenia, malnutrition, vitamin D deficiency and factors related to L-Dopa metabolism2.
There is a universal lack of clear guidelines in management of bone health in patients with Parkinson’s disease, and no reference to PD-specific peri-operative guidance in standardised fracture neck of femur pathways. On that basis and from anecdotal evidence of poor management and outcomes of Parkinson’s patients who suffer a hip fracture, lack of consistent review of bone health in the outpatient setting, we embarked on a quality improvement project. We divided the project into an inpatient and an outpatient arm.
Aims/Objectives
To review inpatient care and outcomes for patients with Parkinon’s disease who experience a fractured neck of femur.
Method
A retrospective review of 18 months of data from our trust’s national hip fracture database was reviewed. This covered the period January 2015 to June 2016. This data includes information on: length of stay (LOS), discharge destination, time to surgery, performance status (ASA) and cognition (pre- and post-operative AMT [abbreviated mental test]). A sample of case notes of patients with Parkinson’s was also reviewed in more depth.
Following review of this data, a review of available Parkinson’s medications was also undertaken.
Results
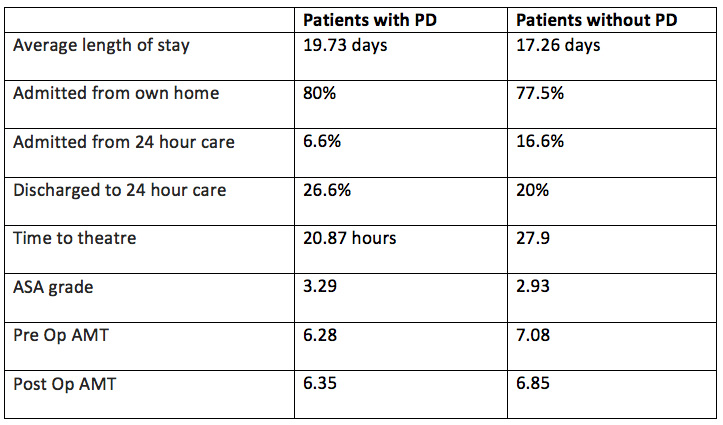
659 patients were admitted with a fractured neck of femur over the 18 months. Fifteen patients (2.25%) had a working diagnosis of idiopathic PD. The patients with PD had a total of 296 bed days with a 2.46 days longer average LOS; 19.73 (10–46) days, compared to the patients without PD average of 17.27 (1–120) days.
The patients with Parkinson’s were more likely to be residing in their own home pre-op, however had a higher rate of discharge to 24 hour care.
Patients with PD did have a shorter time to theatre.
The table below summarises the results:
The review of case notes showed high rates of delirium, constipation, urinary catheter insertion and delay in physio review. One patient was inappropriately prescribed a rotigotine patch. Another patient was given intravenous haloperidol in theatre recovery, when they were in urinary retention and settled following a catheter.
Parkinson’s disease medications were not routinely stocked on the orthopaedic wards. They are currently only available in the emergency medication cupboard or on the geriatric medicine wards.
Discussion and future plans
Results reflect the ethos that patients with Parkinson’s are pre-morbidly higher functioning at time of hip fracture; however, have increased peri-operative morbidity and poorer outcomes, including admission to 24 hour care. Having reviewed outcomes and patient journeys following hip fracture, and outpatient bone health management, we are implementing practice change at trust level. During our current transition to a paperless system, we are opportunistically augmenting our Fracture Neck of Femur Pathway, to include a PD subsection. This peri-operative guidance will include medication management, NBM status, common complications, a directive section on rehab and prominently placed contact details for our PD Nurse specialist. We also have an IV Bisphosphonate pathway as a once-off therapeutic opportunity for selected patients. In terms of in-building systematic bone health review to out-patient assessments, we have proposed 2-yearly review. We are also engaging nursing staff in out-patients to ask the question of “any falls or fractures” since last review, as well as planning the addition of an e-prompt on our proforma.
References
- Lyell, V et al (2015) Assessment and management of fracture risk in patients with Parkinson’s disease Age Ageing 44 (1): 34-41
- Van den bos, F et al (2013) Parkinson’s disease and osteoporosis Age Ageing 42: 156–162.

