Cervical spine injury (CSI) in children is rare but can result in mortality and significant morbidity. The biomechanics of a child’s cervical spine are very different from those of an adult. This has implications in the management of paediatric CSI [1].
Epidemiology
CSI is present in 1-3% of paediatric trauma patients [2-4]. Approximately 72% of spinal injuries in children <8 years old occur in the cervical spine [5]. The cause of injury is influenced by age. Falls are the commonest cause of CSI in the younger population. This is followed by pedestrian and passenger seat accidents in the slightly older group. Sports related accidents are seen most commonly among adolescents. Overall, 26-61% of CSI result from motor vehicle accidents, 34-48% from falls, and sports injuries represent 3- 20% [6,7]. Studies have shown that young males have a higher incidence of CSI, suggesting higher risk behaviour in this group. Patients who have had cervical spine surgery or have a history of CSI are at an increased risk of CSI. Genetic conditions such as osteogenesis imperfecta may result in an increased incidence of spinal fractures. Diseases affecting the ligamentous structures, including Down’s syndrome, Marfan’s syndrome and Ehlers Danlos syndrome, are associated with an increased susceptibility to CSI [8].
Biomechanics – anatomical factors

intubated child.
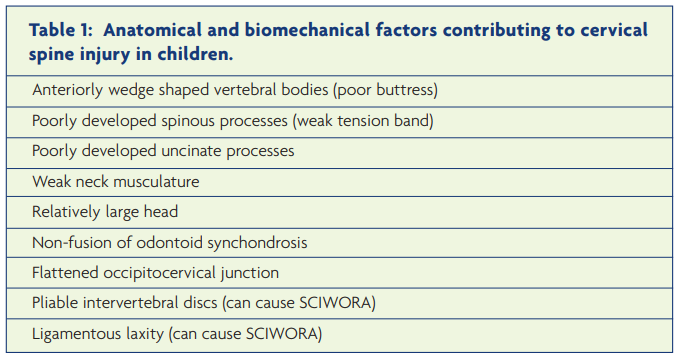
The paediatric cervical spine is intrinsically susceptible to spinal cord injury. A number of anatomical factors account for this (Table 1). In essence, the relatively large child’s head, supported by relatively weak neck musculature, upon a developing spinal column with lax ligaments and pliable discs, is vulnerable to injury [9-11]. In young children the fulcrum for movement is located in the upper cervical spine, leading to a relatively high incidence of injury in the upper cervical spine in this age group. In children over eight years the fulcrum migrates caudally to C5/6 – this is mirrored by an increase in the number of injuries in this region of the spine. Figure 1 shows a typical site of paediatric spinal column injury involving C2.
Initial management considerations
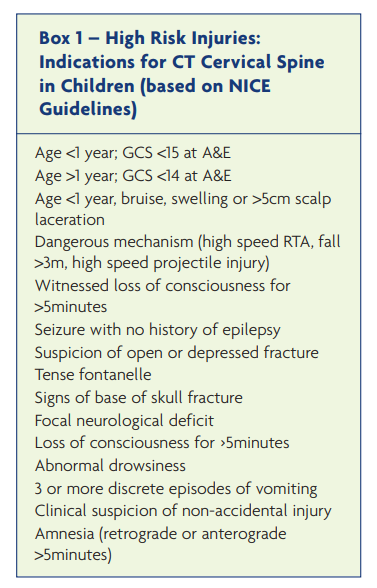
The management of a child with a cervical spine injury is governed by advanced trauma life support principles. Pertinent issues and differences from adult management will be discussed here. The relatively large head puts the spine into kyphosis when supine. Thus the body should be raised by 2.5cm, or a spinal board with an appropriate head indentation should be used. The National Institute for Health and Clinical Excellence (NICE) guideline recommends that high risk patients should have a CT scan of the neck before clinical assessment (Box 1). Patients with a significant head injury are considered ‘at risk’ of a concurrent cervical spine injury as are other high risk patients (eg Down’s syndrome) [12-15].
Resuscitation
Paediatric patients in spinal shock are susceptible to hypotension and poor cord perfusion. They require vigilant fluid management, oxygenation and often ventilation. Early introduction of vasopressors for adequate cord perfusion are indicated if blood pressure is suboptimal despite normal volume status. Most fatalities seen in spinal cord injury (SCI) patients result from other injuries including head injuries. A high index of suspicion must be exercised to ensure that concealed causes of haemorrhage are not overlooked. Cases of missed second non-continuous spinal cord injuries among children have also been reported [16]. Lesions above the T6 level may cause autonomic disturbances including impaired temperature regulation, compounded by the high surface area to volume ratio of younger children.
Radiology
Plain cervical radiographs vs CT
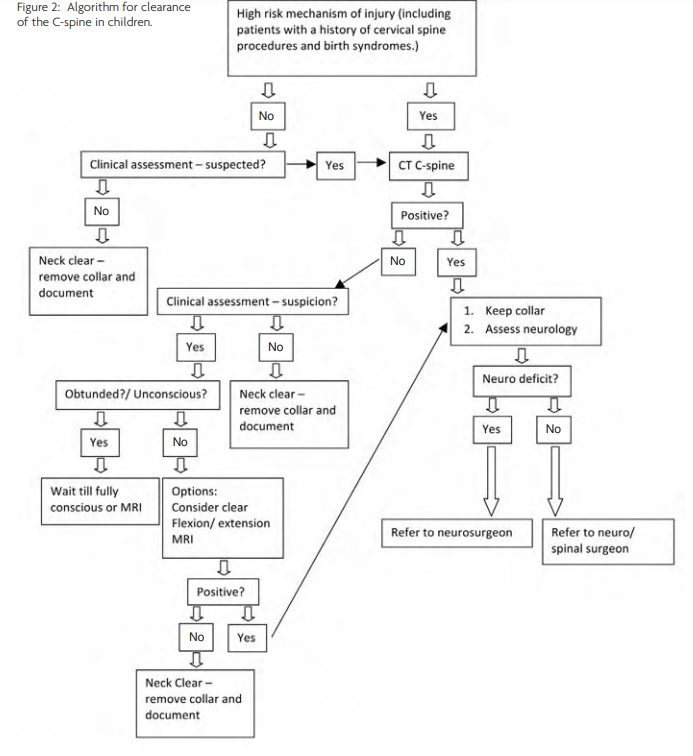
Although a plain cervical spine radiograph exposes the immature vertebrae and growing thyroid to less radiation than a CT of the neck, its use as a screening tool for cervical spine injury is suboptimal. In adults, plain cervical spine radiographs have a sensitivity for fracture detection of 46 to 60%.[17-20] Normal variations in children such as pseudosubluxation, absence of lordosis, epiphysial variations, unfused synchondroses, and incomplete ossification render the plain radiograph difficult to interpret. NICE recommends a CT neck in all patients in whom a CT of the head is indicated because of the high association with head injury (Box 1). [21] CT provides the best resolution and detail for bone injury and is a first line investigation. Reconstructions are helpful in diagnosing fractures and misalignments, and in planning management. An algorithm for radiological clearance of the cervical spine is shown in Figure 2.
The paediatric C-spine radiograph
Although plain radiographs are not as sensitive as CT or MRI in the detection of cervical spine injury an understanding of interpretation is important. A lateral and anteroposterior (AP) view are commonly performed. In younger patients it is difficult to obtain an open-mouth view because of poor compliance.
Vertebral alignment should be studied on the lateral view. The posterior portion vertebral body height is slight taller than the anterior body height, giving the vertebrae a wedge/ rhomboid shape. On the AP view the dens should be equidistant from the lateral masses of C1 and facets of C1/C2 should align. The spinous processes should align and the disc spaces should be symmetrical and similar. In children <8 years the predental space should be less than 5mm (3mm if older), the prevertebral space should be less than 7mm (5mm if older) or less than 1/3 the width of the vertebral body at C3. At C6 it should be less than 14mm (22mm if older). Lack of lordosis is often due to muscle spasm which may be due to a fracture. However, this can be present in some children as a normal variant or as a consequence of positioning on a spinal board. The subdental synchondrosis is the most common normal radiological abnormality mistaken for an odontoid fracture. This shows as a linear lucency at the base of the dens; fusion with the body of C2 occurs between age three and six years. The os terminale is a separate ossification centre that may be present at the tip of the peg i.e. a fragment at the superior-most tip of the odontoid could be a fracture or a normal finding. Pseudosubluxation is found in up to 40% of the paediatric population on lateral C spine x-rays at C2/C3. This shows as 4mm or 40% anterior displacement especially when the child is not placed on a paediatric spinal board. To distinguish from true subluxation (which could imply a Hangman’s fracture) the clinical picture must be considered. The position of the anterior aspect of the C2 spinous process should lie within 2mm of Swischuk’s line (a line drawn from the anterior aspect of C1 to C3 spinous processes) [22-24].
Clinical assessment
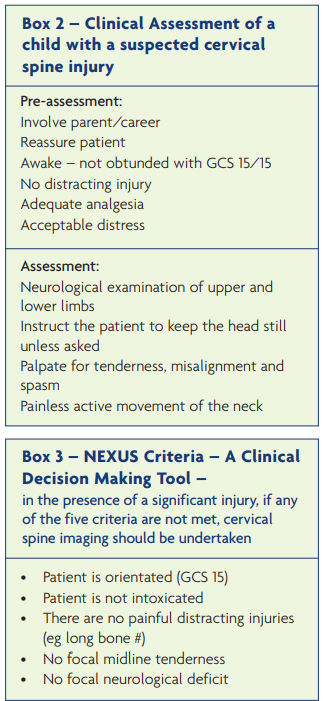
The key steps in the management of a child with a possible spinal column injury are (i) determining if there is a neurological deficit and (ii) whether there is evidence of a radiological abnormality (Box 2). The history should focus on the mechanism and mode of injury. The most common symptom is neck pain and focal midline tenderness is the commonest sign. If the child is orientated, does not have any other painful distracting injury and is not under the influence of drugs, the neck can be assessed before imaging. A child in distress can be examined after analgesia. A neurological examination should be performed followed by checking for focal midline tenderness and then examining the active range of movement of the neck as suggested by the National Emergency X-Radiography Utilisation Study (NEXUS) criteria (Box 3) [25,26].
The Canadian C-spine rule is a checklist evaluated in individuals over 16 years old that identifies low risk patients in which clinical clearance can safely be conducted. Although both the Cervical C-spine rule and the NEXUS guidelines have not been validated for children, they are being applied to fully conscious, compliant children in order to avoid excessive radiation exposure at a young age [27-29].
MRI
MRI is the most sensitive tool for the detection of spinal cord injury, nerve damage and ligamentous injuries [30]. Transient or persistent neurological symptoms and signs or suspicion of a vascular injury, warrant an MRI. A normal MRI is associated with a good prognosis. Spinal cord injury, including haematomyelia, suggests a poor prognosis. Surgically amenable lesions such as a traumatic prolapsed disc and extradural or subdural haemorrhage are best detected using MRI. In one study 31% of patients with neurological symptoms and signs with normal plain films or CT scans were shown to have abnormal MRI findings [31].
Management
Role of steroids
To date there are no studies that have evaluated the use of high dose steroids in the management of acute spinal cord injury in a paediatric population. The National Acute Spinal Injury Study excluded paediatric patients [32]. Although the study concluded in favour of early use of methylprednisolone (30mg/kg in the first hour followed by 5.4 mg/kg/h for 23 hours), there have been robust discussions about the clinical significance of the marginal advantages seen. The use of steroids is highly controversial and remains at the discretion of the treating physician.
Thromboembolism
DVT is quite uncommon in this age group. It occurs more commonly in patients with central venous lines and those who suffer from severe sepsis. Studies have not found paralysis or immobilisation alone to be a significant risk factor for thrombosis in children; DVT prophylaxis is therefore not necessarily indicated in every child with a spinal cord injury [33-35].
Specific cervical spine injuries seen in paediatric patients
Atlanto-occipital dissociation
Atlanto-occipital dissociation is usually a fatal injury seen in children who are involved in high velocity/rapid deceleration motor vehicle accidents. The relatively large head has greater inertial moment than the spine leading to distraction and dissociation. Survivors usually harbour significant neurological deficits. The injury may be difficult to detect with initial imaging; widening of the O-C1 distance (>5mm) is a characteristic sign. MR scanning confirms the presence of injury. Internal fixation and fusion is the mainstay of treatment. Traction can lead to further distraction causing further neurological deficit.
Atlanto-axial rotatory injuries
Rotatory injuries to the atlanto-axial complex are more common in children than in adults. The initiating trauma may be minor and is accompanied by painful torticollis. Imaging investigations may be difficult to interpret in the presence of torticollis. Plain x-rays show anterior displacement of the lateral mass of C1 in relation to the dens, and rotation of the C2 spinous process. CT scans can be helpful, demonstrating the anatomical relationships of C1/2.
Rotation of the neck normally occurs in three phases (Figure 3). Armed with this knowledge Pang and Li have defined three grades of rotatory injury [36-38]. The severity of injury probably represents a continuum from the limits of normality to true subluxation. A grade I injury is at the severe end of the spectrum and represents a ‘sticky’ association between C1 and C2 in a locked position. A Grade III injury shows mild resistance to rotation. Treatment is usually conservative with minor cases recovering spontaneously. Other cases require manual or halter traction reduction with immobilisation in a hard collar. The duration of collar placement is generally recommended to equal the length of time the torticollis was present before treatment. Fusion is rarely required [11].

Disruption of the odontoid synchondrosis
The synchondrosis between the dens and the body of C2 is vulnerable to injury before ossification at the age of seven. Such injury is usually treated with prolonged (>10 weeks) external immobilisation, although internal fixation and fusion may be required if a nonoperative approach fails to achieve union.
Subaxial spine injuries
In children, subaxial fractures are less common than in adults. Other injuries include unilateral and bilateral facet dislocations. Investigation should actively look for ligamentous instability. An angulation of >11 degrees and/or >3.5mm subluxation should warn of ligamentous injury and instability [39]. Evidence on the management is largely based on retrospective observational studies and case reports. The principles of treatment are similar to those deployed in adults; manual reduction, traction and surgery with internal fixation and fusion.
SCIWORA (spinal cord injury without radiological abnormality (Figure 4)

note the cord contusion at C6 and C7 and the presence of
a subtle disc bulge.
SCIWORA is a condition seen in children that is characterised by a traumatic neurological deficit in the absence of fracture or ligamentous injury on plain radiograph, flexion/ extension views or CT [40,41]. Pathology may be evident on MR scanning. About 50-60% of children with traumatic spinal cord injuries do not show any abnormality on X-ray or CT [16]. SCIWORA is more common in children <9 years, but can be caused by sporting injuries in the older child. Signs of myelopathy can develop several days after the injury. SCIWORA can be caused by flexion compression of the cord (which may cause a reversible disc herniation), or hyperextension with inward buckling of the interlaminar ligaments. A distraction injury can also cause cord damage: although the paediatric spinal column can be distracted to up to 5cm, the cord itself is much less extensile.
Patients with congenital spinal canal stenosis, (e.g. trisomy 21) and hyperelasticity conditions (e.g. Ehlers Dahlos syndrome and pseudoxanthoma elasticum) are particularly at risk of SCIWORA. The prognosis of SCIWORA is governed by the MRI findings. Haematomyelia predicts a poor prognosis, whilst an excellent recovery may occur in the absence of a visible parenchymal injury [42]. There have been no reported cases of children with SCIWORA who have later developed spinal instability. Therefore, early immobilisation directed at the avoidance of aggravating the cord injury is appropriate. Although the mainstay of treatment has been prolonged immobilisation others question this view. Once spinal stability has been confirmed with flexion/ extension views, consideration can be given to the early cessation of immobilisation.
External immobilisation
The unstable cervical spine can be immobilised externally. Options include collar, halo and traction or a Minerva jacket [43]. A collar gives limited protection and can result in pressure sores. A Halo ring is commonly used to enable traction and subsequent external immobilisation in children. Traction is crucial in restoring spinal alignment. For children less than four years of age, one pound per level is used. This can be increased to two pounds per level for older children. Careful serial radiographs are required to check for reduction and to avoid over-distraction. The patient is usually supine in bed, thus exposed to atelectasis, pressure ulcers, and other problems associated with prolonged mobility [44]. In children less than two years of age, multiple pins, up to six or eight, are used to finger tightness. Halo use can be complicated by pin track infections, dural penetration, and supraorbital nerve injuries. In older children fewer pins with greater torque are used. The Minerva jacket has been reported to be superior to a halo in preventing flexion and extension at every vertebral level [43].
Surgery
Internal fixation and fusion of the cervical spine is normally reserved for the minority of children with occipito-atlanto disruption, unstable subaxial spinal injuries or failed external fixation treatments. The aim of surgery is to stabilise the spine, prevent further neurological deterioration and facilitate early rehabilitation. The challenges seen in paediatric spinal surgery are anatomical and technological. The small vertebral body, epiphysis and endplate may effect abnormal growth and development if insulted. The poorly developed supporting musculature and the limited availability of suitable implants contribute to difficulties. By the age of 10, the cervical spine has almost reached its adult height and the complication rate is lower.
Careful surgical planning is needed to study the anatomical variables. If the patient is placed supine, the head/body position needs to be adjusted by using a head recess or body elevation. In the prone position, careful spinal stabilisation is needed. The Mayfield head clamp can be used in older children using a force of 30-40N. Dissection of the C2 muscles must be minimised to avoid instability. Blood loss should also be minimised. In children <10 years of age, posterior instrumentation and plating is avoided because of instrument bulk [43,44]. In children younger than 10 years of age, posterior vertebral arthrodesis can predispose children to the crankshaft phenomenon where the anterior body continues to grow, causing progressive deformity [45].
Complications of SCI and Treatment
SCI is debilitating and can cause neurological and systemic sequelae. Appropriate spinal care and rehabilitation are mandatory.
- Cardiovascular complications include bradycardia, hypotension and other autonomic disturbances in the early post-traumatic phase.
- Respiratory complications include lung atelactasis, aspiration pneumonia and infection. Tracheostomy may be required in some patients.
- Gastrointestinal complications include reflux oesophagitis, Cushing’s ulcer, prolonged ileus and nutritional imbalance, constipation and a risk of laxative overuse. Percutaneous endoscopic gastrostomy (PEG) may be needed in some children.
- Urological complications include a predisposition to calculus formation and urinary tract infection.
- Neurological and musculoskeletal complications include paralysis, disuse atrophy, contractures, joint deformities, heterotopic ossification, sensory loss and neuropathic ulcers, osteopaenia and rarely post-traumatic syringomyelia.
- Psychosocial complications can be a major burden. The child and family can be affected with all aspects of life being subject to significant change.
Conclusion
Childhood SCI is a devastating phenomenon. Fortunately it is rare and has specific injury patterns due to anatomical and biomechanical factors. SCIWORA remains a diagnostic pitfall if not suspected early. MRI is an important tool and provides prognostic information. Management of a child with a SCI requires a multidisciplinary approach to minimise the risk of secondary problems and to rationalise management in the absence of Class I evidence.
References
- Viccellio P, Simon H, Pressman BD, Shah MN, Mower WR, Hoffman JR. A prospective multicenter study of cervical spine injury in children. Pediatrics 2001;108(2):E20. https://doi.org/10.1542/peds.108.2.e20
- Kokoska ER, Keller MS, Rallo MC, Weber TR. Characteristics of pediatric cervical spine injuries. J Pediatr Surg 2001;36(1):100-5. https://doi.org/10.1053/jpsu.2001.20022
- Baker C, Kadish H, Schunk JE. Evaluation of pediatric cervical spine injuries. Am J Emerg Med 1999;17(3):230-4. https://doi.org/10.1016/S0735-6757(99)90111-0
- Dietrich AM, Ginn-Pease ME, Bartkowski HM, King DR. Pediatric cervical spine fractures: predominantly subtle presentation. J Pediatr Surg 1991;26(8):995-9. https://doi.org/10.1016/0022-3468(91)90850-S
- Kewalramani LS, Kraus JF, Sterling HM. Acute spinal-cord lesions in a pediatric population: epidemiological and clinical features. Paraplegia 1980;18(3):206-19. https://doi.org/10.1038/sc.1980.36
- Patel JC, Tepas JJ, III, Mollitt DL, Pieper P. Pediatric cervical spine injuries: defining the disease. J Pediatr Surg 2001;36(2):373-6. https://doi.org/10.1053/jpsu.2001.20720
- Cirak B, Ziegfeld S, Knight VM, Chang D, Avellino AM, Paidas CN. Spinal injuries in children. J Pediatr Surg. 2004;39(4):607-12. https://doi.org/10.1016/j.jpedsurg.2003.12.011
- Leonard JC, Kuppermann N, Olsen C, Babcock-Cimpello L, Brown K, Mahajan P et al. Factors associated with cervical spine injury in children after blunt trauma. Ann Emerg Med 2011;58(2):145-55. https://doi.org/10.1016/j.annemergmed.2010.08.038
- Cattell HS, Filtzer DL. Pseudosubluxation and other normal variations in the cervical spine in children. A study of one hundred and sixty children. J Bone Joint Surg Am 1965;47(7):1295-309. https://doi.org/10.2106/00004623-196547070-00001
- BAILEY DK. The normal cervical spine in infants and children. Radiology 1952;59(5):712-19. https://doi.org/10.1148/59.5.712
- Gore PA, Chang S, Theodore N. Cervical spine injuries in children: attention to radiographic differences and stability compared to those in the adult patient. Semin Pediatr Neurol 2009;16(1):42-58. https://doi.org/10.1016/j.spen.2009.03.003
- Whitfield P. The National Institute of Clinical Excellence Head Injury Guidelines: A Summary to Assist Implementation. ACNR 8[1]. 2008. https://doi.org/10.47795/ALGP2007
- NICE. CG56. Head injury: triage, assessment, investigation and early management of head injury in infants, children and adults. 2011.
- Van D, Gahagan CA. Down syndrome. Cervical spine abnormalities and problems. Clin Pediatr (Phila) 1988;27(9):415-18. https://doi.org/10.1177/000992288802700901
- Hankinson TC, Anderson RC. Craniovertebral junction abnormalities in Down syndrome. Neurosurgery 2010;66(3 Suppl):32-8. https://doi.org/10.1227/01.NEU.0000365803.22786.F0
- Heilman CB, Riesenburger RI. Simultaneous noncontiguous cervical spine injuries in a pediatric patient: case report. Neurosurgery 2001;49(4):1017-20. https://doi.org/10.1227/00006123-200110000-00046
- Brohi K, Healy M, Fotheringham T, Chan O, Aylwin C, Whitley S et al. Helical computed tomographic scanning for the evaluation of the cervical spine in the unconscious, intubated trauma patient. J Trauma 2005;58(5):897-901. https://doi.org/10.1097/01.TA.0000171984.25699.35
- Mathen R, Inaba K, Munera F, Teixeira PG, Rivas L, McKenney M et al. Prospective evaluation of multislice computed tomography versus plain radiographic cervical spine clearance in trauma patients. J Trauma. 2007;62(6):1427-31. https://doi.org/10.1097/01.ta.0000239813.78603.15
- Holmes JF, Akkinepalli R. Computed tomography versus plain radiography to screen for cervical spine injury: a meta-analysis. J Trauma 2005;58(5):902-5. https://doi.org/10.1097/01.TA.0000162138.36519.2A
- Lindsey RW, Diliberti TC, Doherty BJ, Watson AB. Efficacy of radiographic evaluation of the cervical spine in emergency situations. South Med J 1993;86(11):1253-5. https://doi.org/10.1097/00007611-199311000-00013
- CG56 Head injury: review proposal consultation.
- Lustrin ES, Karakas SP, Ortiz AO, Cinnamon J, Castillo M, Vaheesan K et al. Pediatric cervical spine: normal anatomy, variants, and trauma. Radiographics 2003;23(3):539-60. https://doi.org/10.1148/rg.233025121
- Fesmire FM, Luten RC. The pediatric cervical spine: developmental anatomy and clinical aspects. J Emerg Med. 1989;7(2):133-42.
- Khanna G, El-Khoury GY. Imaging of cervical spine injuries of childhood. Skeletal Radiol 2007;36(6):477-94. https://doi.org/10.1007/s00256-006-0223-0
- Hoffman JR, Wolfson AB, Todd K, Mower WR. Selective cervical spine radiography in blunt trauma: methodology of the National Emergency X-Radiography Utilization Study (NEXUS). Ann Emerg Med 1998;32(4):461-9. https://doi.org/10.1016/S0196-0644(98)70176-3
- Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-9. https://doi.org/10.1056/NEJM200007133430203
- Stiell IG, Wells GA, Vandemheen KL, Clement CM, Lesiuk H, De M, V et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA 2001;286(15):1841-8. https://doi.org/10.1001/jama.286.15.1841
- Burns EC, Yanchar NL. Using cervical spine clearance guidelines in a pediatric population: a survey of physician practices and opinions. CJEM 2011;13(1):1-6. https://doi.org/10.2310/8000.2011.100220
- Slack SE, Clancy MJ. Clearing the cervical spine of paediatric trauma patients. Emerg Med J 2004;21(2):189-93. https://doi.org/10.1136/emj.2003.012310
- Radiographic assessment of the cervical spine in symptomatic trauma patients. Neurosurgery 2002;50(3Suppl):S36-S43. https://doi.org/10.1097/00006123-200203001-00009
- Keiper MD, Zimmerman RA, Bilaniuk LT. MRI in the assessment of the supportive soft tissues of the cervical spine in acute trauma in children. Neuroradiology 1998;40(6):359-63. https://doi.org/10.1007/s002340050599
- Shepard MJ, Bracken MB. The effect of methylprednisolone, naloxone, and spinal cord trauma on four liver enzymes: observations from NASCIS 2. National Acute Spinal Cord Injury Study. Paraplegia 1994;32(4):236-45. https://doi.org/10.1038/sc.1994.43
- Sandoval JA, Sheehan MP, Stonerock CE, Shafique S, Rescorla FJ, Dalsing MC. Incidence, risk factors, and treatment patterns for deep venous thrombosis in hospitalized children: an increasing population at risk. J Vasc Surg 2008;47(4):837-43. https://doi.org/10.1016/j.jvs.2007.11.054
- van Ommen CH, Heijboer H, Buller HR, Hirasing RA, Heijmans HS, Peters M. Venous thromboembolism in childhood: a prospective two-year registry in The Netherlands. J Pediatr 2001;139(5):676-81. https://doi.org/10.1067/mpd.2001.118192
- Nowak-Gottl U, Kosch A, Schlegel N, Salem M, MancoJohnson M. Thromboembolism in children. Curr Opin Hematol 2002;9(5):448-53. https://doi.org/10.1097/00062752-200209000-00010
- Fielding JW, Hawkins RJ. Atlanto-axial rotatory fixation. (Fixed rotatory subluxation of the atlanto-axial joint). J Bone Joint Surg Am 1977;59(1):37-44. https://doi.org/10.2106/00004623-197759010-00005
- Pang D, Li V. Atlantoaxial rotatory fixation: part 2-new diagnostic paradigm and a new classification based on motion analysis using computed tomographic imaging. Neurosurgery 2005;57(5):941-53. https://doi.org/10.1227/01.NEU.0000181309.13211.3A
- Pang D, Li V. Atlantoaxial rotatory fixation: Part 1- Biomechanics of normal rotation at the atlantoaxial joint in children. Neurosurgery 2004;55(3):614-25. https://doi.org/10.1227/01.NEU.0000134386.31806.A6
- White AA, III, Panjabi MM. The basic kinematics of the human spine. A review of past and current knowledge. Spine (Phila Pa 1976) 1978;3(1):12-20. https://doi.org/10.1097/00007632-197803000-00003
- Pang D, Wilberger JE, Jr. Spinal cord injury without radiographic abnormalities in children. J Neurosurg. 982;57(1):114-29. https://doi.org/10.3171/jns.1982.57.1.0114
- Pollack IF, Pang D, Sclabassi R. Recurrent spinal cord injury without radiographic abnormalities in children. J Neurosurg 1988;69(2):177-82. https://doi.org/10.3171/jns.1988.69.2.0177
- Gray R Fleicher SLFMH. Textbook of Pediatric emergency medicine Ch 106. [5th Edition], 1409-1431. Lippincott Williams and Wilkins.
- McCall T, Fassett D, Brockmeyer D. Cervical spine trauma in children: a review. Neurosurg Focus 2006;20(2):E5. https://doi.org/10.3171/foc.2006.20.2.6
- Laurel C Blakemore LC EMRCMKERKE. American academy of Orthopaedics surgeon. 2011 Annual Meeting Instructional Course Lecture Handout.
- Dubousset J, Herring JA, Shufflebarger H. The crankshaft phenomenon. J Pediatr Orthop 1989;9(5):541-5 https://doi.org/10.1097/01241398-198909010-00008




