Abstract
Before the invention of the ophthalmoscope in 1851, doctors were neither able to recognise papilloedema nor to diagnose accurately intracranial hypertension, malignant hypertension and inflammatory and systemic disorders affecting the optic fundus. This paper seeks to uncover early descriptions and experiments that tried to unravel the causes of the swollen optic disc, its mechanism and its clinical significance. Papilloedema is a purely descriptive name that requires the underlying cause to be specified.
Papilloedema is perhaps the most important physical sign that the aspiring neurologist has to recognise (Figure 1). The advent of non-invasive imaging techniques is no substitute for its clinical recognition. Before Helmholtz’s (1821-1894) invention of the ophthalmoscope in 1851 [1], doctors were unable clearly to distinguish optic neuritis from uveitis, glaucoma, orbital tumours, and other ocular and systemic disorders [2].
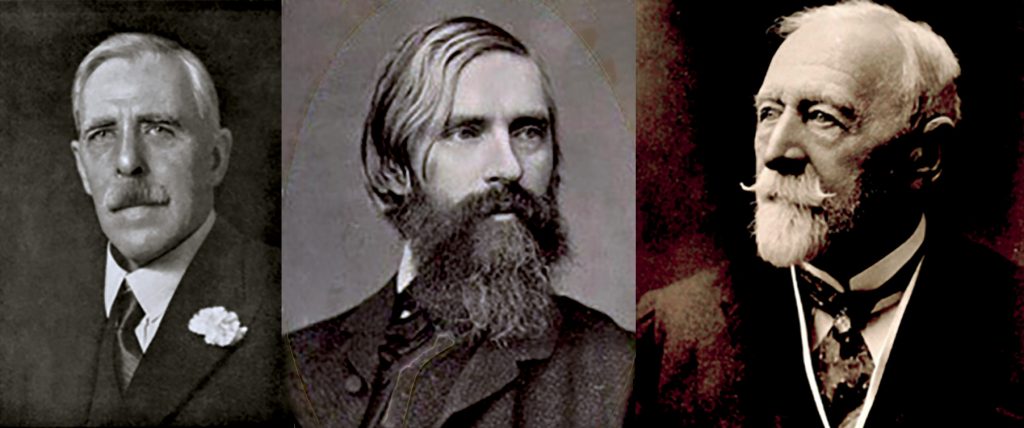
At the end of the nineteenth century British ophthalmology enjoyed an array of internationally esteemed exponents, who included: Jonathan Hutchinson, Nettleship, Doyne, Marcus Gunn, Treacher Collins, Paton and Parsons [3]. The word ‘papilloedema’ was first used in 1908 by Sir John Herbert Parsons (1868-1957) (Figure 2) to replace von Gräfe’s term, ‘choked disc’ (Stauungspapille), caused by raised intracranial pressure. Papillitis, a word used in 1879 by Gowers, is derived from the Latin papilla a nipple. Parsons tried to distinguish the terms then in use, such as ‘optic neuritis’, ‘choked disc’ and ‘papillitis’ [4], although it is clear he was simply renaming the appearance of the optic disc already recognised for over 50 years.
The German term Stauungspapille or strangled papilla had been employed by the ophthalmologist, Albrecht von Gräfe [Graefe] [*] (1828–1870) (Figure 3). He reported in 1860:
a state due to increased pressure within the cranium from the extension of a proliferating process at the base of the brain along the connective elements of the optic nerve eye (‘descending neuritis’) [5].
He gave a lucid description:
…the papilla very considerably and irregularly swollen; it rose abruptly on the one side, to return on the opposite to its proper level. The otherwise transparent substance appeared turbid with an unusually strong admixture of red, as did the adjacent retina, whereby the choroidal boundary of the optic nerve was completely effaced. The retinal veins were dilated, unusually tortuous, very dark in streaks, stood out irregularly in the opaque substance, the arteries were proportionally slight. (cited by Koster) [6]
In this paper, I have no new light to shed upon the controversial mechanisms of the swollen optic disc but refer to selected historical descriptions, views and experiments (reviewed by Hayreh) [7], which tried to unravel them and their causes.
Ludwig Türck (1810-68) in 1853 first described retinal haemorrhages, due to stasis in the cavernous sinus caused by the raised intracranial pressure in intracranial tumours [8]. But it was von Gräfe, who in four cases of ‘sarcoma cerebri’ observed a:
high–grade swelling of the optic nerve head was determined by ophthalmoscopy, … which was pathologically–anatomically examined.’ He said that pressure of the tumours on the cavernous sinus led to a congestion of the blood in the retinal veins, and to the tumefaction of the papilla, which gradually led to hypertrophy of the connective tissue [5].
Hughlings Jackson (1835–1911) in 1871 recognised optic neuritis in brain tumours — and even described four stages, but wisely cautioned that the appearances were not specific and demanded a search for other causes [9].
The nomenclature was bewilderingly varied [10]. Harvey Cushing (1869–1939), preferring the term choked disc coined by von Gräfe, wrote:
…papilledema, …actually conveys nothing more of the process than does choked disc, and its adoption would only add confusion.
This view was supported in the minutely argued text of Thomas Clifford Allbutt (Figure 4) (1836-1925), physician to the General Infirmary at Leeds. The ophthalmoscope [11] was at first underused, causing Allbutt to warn:
No observer of nervous diseases can now dispense with the use of the ophthalmoscope; and the reports of cases in which the instrument was not frequently used must henceforth be regarded as defective in an important particular [12].
Allbutt preferred the term ‘choked disc’ [12], though both Hughlings Jackson and William Gowers (1845-1915) in 1879 called it ‘optic neuritis’. Supporting von Gräfe, Allbutt described:
The disc is prominent, its outlines are dimmed, and the retinal veins are distended, dark and tortuous. This state we call choked, swollen, or congested disc. [with von Graefe, this he attributed to increased pressure within the cranium]
At other times we see rather a proliferative than a dropsical process… vessels are now less distended…concealed by new elements, which also extend over and conceal a wide belt of surrounding retina. To this state the term optic neuritis, neuroretinitis or descending neuritis is applied.
However, confusion persisted [13] in both nomenclature and cause, since not all papilloedema was due to raised intracranial pressure.
Edward Nettleship, (1845-1913) who removed a cataract from William Gladstone, and attended Queen Victoria for the same condition, was according to Sir John Parsons: the most scientific teacher of his time. In 1884 Nettleship gave a comprehensive account of ‘retro-ocular [syn. retrobulbar] neuritis’, almost certainly demyelinating, emphasising pain on eye movement, abnormal disc appearances and impaired colour vision [14]. Eleven of his 16 patients had a central scotoma. He accurately characterised its features:
Failure of sight limited to one eye, often accompanied by neuralgic pain about the temple and orbit and by pain in moving the eye; many recover but permanent damage and even total blindness may ensue; there is at first little, sometimes no, ophthalmoscopic change, but the disc often becomes more or less atrophic in a few weeks… The defect in vision is often described at first as a ‘‘gauze’’ or a ‘‘yellow mist’’ or a ‘‘dark patch’’ or a ‘‘spot’’ which covers the object looked at and gives an unnatural colour, the hand looking, for example, as if covered by a brown glove [15].
Thomas Buzzard (1831-1919), close friend both of Hughlings Jackson and Sir David Ferrier, in 1893 reported the association of optic neuritis with disseminated (multiple) sclerosis [16].
Leslie Paton and Gordon Holmes reported 60 brain tumour patients and by histological examinations explored theories of its pathogenesis [17]. They established that papilloedema was a result of intracranial hypertension [13] and not, as then commonly thought, an inflammatory process. They also observed: ‘as the disc swells lateralward, it displaces the retina … throwing it into series of folds which run concentric with the edge of the disc.’ (Paton’s folds: now well shown on spectral-domain optical coherence tomography).
Pathogenesis
Cushing with Bordley experimentally investigated mechanisms and found that when fluid was forced under pressure into the subdural space, there was engorgement of the retinal veins and the development of papilloedema (Figure 1). They showed that when the fluid pressure was greater than venous pressure there was engorgement of the retinal veins, and when it approached the arterial pressure a high grade choked disc resulted [18].
A swollen disc caused by raised intracranial pressure affects visual acuity late in its course, whereas inflammatory, demyelinating, ischaemic, and proliferative optic neuritis results in early loss of acuity, an enlarged blind spot, central or paracentral scotoma, and impaired colour vision. When papilloedema is caused by raised cerebrospinal fluid pressure, the pressure in the optic nerve sheath slows axoplasmic flow causing swelling of optic nerve fibres and the optic disc. This oedema induces secondary venous stasis and the accumulation of extracellular fluid in the lamina cribrosa [7].
Conclusion
Many arguments based on nomenclature can be resolved by the view that papilloedema can variously result from raised intracranial pressure, malignant hypertension, and from ischaemic optic neuropathy, demyelination, inflammatory and infiltrative diseases of the optic nerve. Papilloedema is, therefore, best understood as a purely descriptive name that requires the underlying cause to be specified.
References
- Helmholtz H. Beschreibung eines Augenspiegels. Berlin, Germany: A Förstner’sche Verlagsbuchhandlung; 1851. https://doi.org/10.1007/978-3-662-41295-4
- Pearce JMS. The Ophthalmoscope: Helmholtz’s Augenspiegel. Eur Neurol 2009;61:244-258. https://doi.org/10.1159/000198418
- Duke-Elder S. John Herbert Parsons, 1868-1957. Biogr. Mems Fell. R. Soc. 1958;4,:204-214. https://doi.org/10.1098/rsbm.1958.0018
- Parsons JH. Pathology of the Eye. London, Hodder & Stoughton.1908;4:1249 et seq.
- von Gräfe A. Über Komplikation von Sehnervenentzündung mit Gehirnkrankheiten. Arch. f. Ophth. VII, 2. 1860. See: https://archive.org/stream/b21287429/b21287429_djvu.txt
- Koster W. Two cases of tumour of the brain, with remarks on the connexion between cerebral tumours and affections of the retina and of the optic nerve. Translated from the Nederlandsch Archief voor Genesen Natuurkunde, le Deel, 4e Aflevering, Utrecht, 1865. (Continued from page 68C.) Medical Press and Circular. https://archive.org/stream/…/medicalpresscirc02londuoft_djvu.txt
- Hayreh SS. Pathogenesis of optic disc edema in raised intracranial pressure. Prog Retin Eye Res. 2016 Jan;50:108-44. https://doi.org/10.1016/j.preteyeres.2015.10.001
- Türck L. Ein Fall von Hämorrhagie der Netzhaut beider Augen. Zeit. Ges. Wien. Ärzte. 1853;9:214-218. Cited by Garrison and Morton’s Medical Bibliography [5870]: 2nd edn. Andre Deutsch, 1954.
- Jackson H. Med Times and Gazette 1871;1: 241,341, 581. cited in: Lecture on optic neuritis from intracranial disease. In: Taylor J, ed. Selected writings of JH Jackson, 2 volumes. 1931. Reprinted: London: Staples Press 1958;2:251-64.
- Lenore FE. Toward a definition of papilledema: a historical review, 1851-1911. Surgical Neurology 1982;17(3):178 – 180. https://doi.org/10.1016/0090-3019(82)90270-1
- Allbutt TC. On the Use of the Ophthalmoscope in Diseases of the Nervous System, Kidneys, etc. Macmillan: I871.
- Allbutt TC. On The Causation And Significance Of The Choked Disc In Intracranial Diseases. Brit med J 1872;1:443-5. https://doi.org/10.1136/bmj.1.591.443
- Horsley V. Optic Neuritis,’ ‘Choked Disc,’ Or ‘Papilloedema. Br Med J. 1910;1:553-558. https://doi.org/10.1136/bmj.1.2566.553
- Pearce JMS. Edward Nettleship and Optic neuritis. Advances in Clinical Neuroscience and Rehabilitation. 2017;17(1);15-16.
- Nettleship E. On cases of retro-ocular neuritis. Trans Ophthal Soc UK 1884;4:186-226.
- Buzzard T. Atrophy of the optic nerve as a symptom of chronic disease of the central nervous system. Br Med J 1893;2:779-784.
[*] Perhaps better known for von Graefe’s sign in hyperthyroidism: a failure of the upper lid to follow a downward movement of the eyeball when the patient looks downward.
