There has been a great increase in interest in the clinical assessment of dementia and in particular in the early diagnosis of dementia in the last few years. We present a method for assessment of patients with cognitive problems based on our experience in the Cambridge memory clinic and teaching on the Cambridge Dementia Course. There have been great advances in the use of neuroimaging and other biomarkers in the diagnosis of dementia but the diagnosis of dementia remains a clinical one based on the clinical assessment of the patient. Assessing cognitive function requires 4 stages:
- History from the patient
- History from a reliable informant (usually taken separately)
- Physical examination of the patient
- Cognitive examination of the patient
In reality, there is always some mixing up of these stages. The detail and responses to questions in the patient’s history provides an informal assessment of their memory. Language problems often become apparent as the patient speaks.
- History from the patient
Because many patients with dementia have reduced insight, it is often difficult to establish the usual features of a neurological history such as the onset of problems and progression, and the informant interview is often more informative.
Important parts of the history include:
- A brief autobiographical sketch, including maximum educational achievement and work history, provides an estimate of their premorbid cognitive abilities. This knowledge is helpful in tailoring subsequent autobiographical interview for assessing their episodic memory.
- Past medical and psychiatric history may provide useful information. For instance, if the patient has atherosclerosis or major psychiatric disease this influences the differential diagnosis.
- Many medications prescribed for the elderly including beta blockers, sodium valproate, and amitriptyline can cause cognitive problems which are often reversible.
- Alcohol consumption is sometimes minimalised or hidden.
- A family history of dementia will be common in any individual coming from a long-lived pedigree but a history of onset of Alzheimer’s disease (AD) at an age younger than 60 years or behavioural variant Frontotemporal dementia (FTD) in a first degree relative is likely to be significant.
- History from an informant
The importance of the informant’s account cannot be over emphasised, not only due to the effect of possible cognitive impairment on the patient’s recollection of the relevant parts of the history but also on their insight into their current problems. Often organic cognitive problems are suspected when the patient’s relative is more concerned, whereas a worried patient and a less concerned informant would normally be associated with “worried well” patients. Self-repetition and repeated questioning are the hallmarks of the episodic memory impairment seen in AD. Tactless remarks, loss of empathy, and sweet tooth are features commonly volunteered by the relatives of behavioural FTD sufferers. Features of REM sleep behavior disorders are frequently noticed by partners of patients with dementia with Lewy body (DLB).
- Physical Examination
Routine physical examination is normal in most patients presenting with dementia. There are sometimes important signs. Some such as papilloedema or a visual field defect will change the differential diagnosis dramatically making a cerebral tumour much more likely. More often in a memory clinic, parkinsonian features will support a diagnosis of dementia with Lewy Body, an apraxic gait would suggest a vascular or mixed dementia, supranuclear gaze palsy would suggest progressive supranuclear palsy or a related condition or a cortical sensory loss would suggest corticobasal syndrome.
Some unconventional signs can be helpful: the “Head turn sign” is a useful feature seen in organic amnesia and denotes the patient’s reliance on their partner during consultation. Patients with visuospatial problems or “truncal” apraxia may have difficulty navigating to their seat and sit on it askew.
- Cognitive Examination
4.1. Short Cognitive Tests (SCTs)
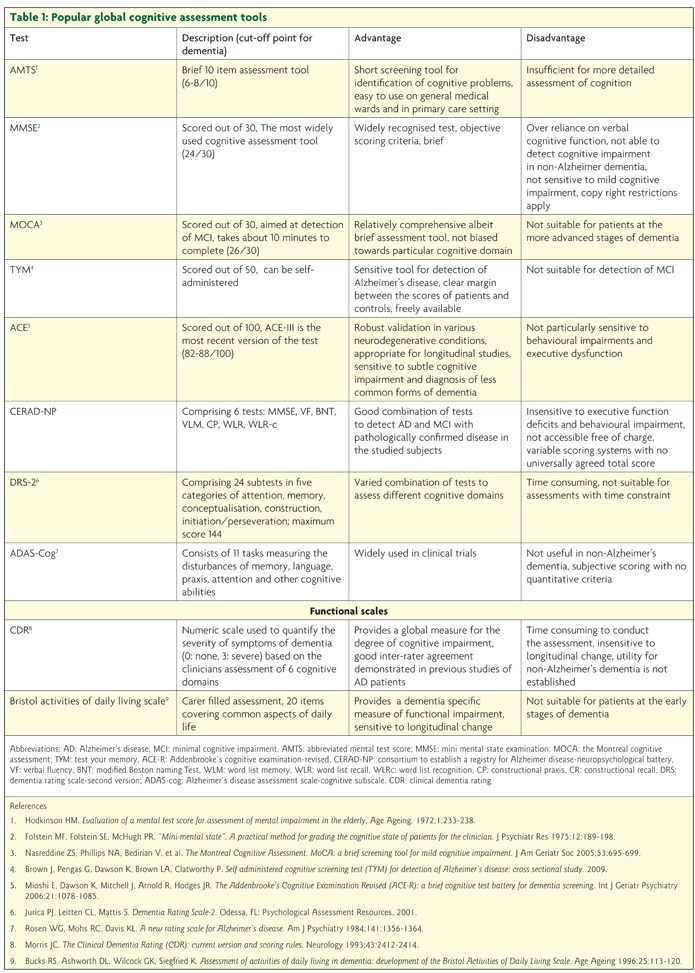
Over the years, many SCTs have been developed. It is crucial to remember that they are aids to the examination of the patient, not diagnostic tests. If time is no object then the Addenbrooke’s Cognitive Examination version 3 (ACE-III) allows a relatively full assessment of the patient and is the test of choice in most memory clinics. The Mini mental state examination (MMSE), despite its many limitations, remains popular but is now restricted by copyright. The Montreal Cognitive Assessment (MoCA) and Test Your Memory (TYM) are more recent innovations which have clear advantages over the MMSE and are quicker to administer than the ACE-III. These are all multi-domain tests which assess several cognitive skills. Other tests such as abbreviated mental test score (AMTS) and GP assessment of cognition (GPcog) are much more limited in scope and whilst widely recommended, are too brief to allow a proper assessment of a patient’s cognition. There is no one test that is universally appropriate for all settings and even for each given situation, different tools have their own weaknesses and benefits. Table 1 provides a summary of the most popular assessment tools and their main pros and cons.
The combination of an experienced clinician’s assessment and a poor score on a short cognitive test is usually sufficient to diagnose dementia. Some patients, however, need a more thorough assessment.
4.2. Problem oriented cognitive assessment
The symptoms mentioned by the patients or their informants during history taking provide diagnostic clues. It is worth remembering that symptomatology in this context has anatomical but not pathological importance as symptoms reflect the involved areas of the brain as opposed to the presumed pathology affecting those areas.
4.2.1. Attention and orientation: Preserved attention and orientation is a prerequisite for normal cognitive function and impaired orientation is a hallmark of delirium.
– 4.2.1.1. Orientation: Time and place orientation are useful clinically; in AD orientation for time is lost before orientation to place. Time orientation should be assessed by asking questions about date, time of the day, day of the week, month of the year, season, and year. Orientation to place can be tested by asking the names of the hospital, ward, town, or home address.
– 4.2.1.2. Attention can be tested by spelling a 5 letter word such as “world” backwards, forward and backward digit span, serial 7s, and recitation of the months of the year or the days of the week in reverse order. In aphasic patients one should opt for less language specific tests such as digit span. Normal forward digit span is considered 6 +/-1 and backward digit span is normally one less than forward.
4.2.2. Declarative memory: This is divided into episodic and semantic memory.
– 4.2.2.1. Episodic memory: Loss of episodic memory is a cardinal feature of AD. The history provides a valuable test of episodic memory; patients are often unable to provide the details of their past medical problems such as dates of operations, etc. Informal autobiographical interview in context of history taking is another effective way of exposing memory lapses. By asking patients questions about life events in both recent and remote past, one can expose memory deficits that may surprise relatives. Patients are often unable to recall recent important news, destination of holidays, or comment on their favourite soap operas. Other complaints such as forgetting appointments or needing shopping lists may reflect poor attention rather than poor memory and are less discriminatory.
– 4.2.2.2 Semantic memory: This is the part of memory that comprises our knowledge about the surrounding world that is not necessarily linked to life events. Conditions such as semantic dementia and some forms of limbic encephalitis involve the anterior temporal lobes and selectively involve semantic memory. Patients who suffer from semantic memory deficits speak fluently and an initial impression can be of normal speech. Semantic paraphasias may provide a diagnostic clue. Asking the patient to repeat a word and then to define it is one way to expose semantic impairments. Patients with semantic dementia have no problems in repeating but are unable to define words like caterpillar, barrister or xylophone. Semantic dementia should be suspected when the patient scores very poorly on naming line drawings or mispronounces irregular words such as pint and dough (surface dyslexia).
4.2.3. Language
Assessment of language starts from the first moments of the consultation. By listening to the patient whilst they provide the history, a trained ear can detect a number of impairments including phonological errors, grammatical mistakes, anomia, and speech abnormalities such as dysarthria and apraxia of speech. Some patients will have an abnormal rhythm of speech (dysprody). Many of these impairments are best appreciated by listening to the patients’ connected speech during an informal interview. A more formal approach complements the informal listening. Language assessment should include testing reading and writing.
– 4.2.3.1. Anomia is a hallmark of aphasia. Anomia or “word finding difficulty” can easily be assessed objectively by asking the patients to name common objects in the consultation room or at their bedside. A watch is a useful aid as it contains components of varied word frequency, therefore difficulty, such as hands, winder, strap, buckle, etc. to expose more subtle anomia. Anomia is non-specific and needs further assessment.
– 4.2.3.2. Comprehension difficulty can be due to a number of factors. Single word comprehension difficulty is a relatively uncommon cause and can be assessed by asking patients to point to objects by either their names or description. Syntactic problems can be identified by asking patients questions put in a syntactically complex structure eg “touch your left ear when I hold up 3 fingers”.
– 4.2.3.3. Impaired repetition can be either at single word level or a problem with sentence repetition. Isolated sentence repetition problems would normally suggest an impairment of the phonological loop component of the working memory. Single word repetition difficulty is usually due to problems with articulation in context of either dysarthria or apraxia of speech. Differentiating speech apraxia from aphasia can be difficult and often debatable.
4.2.4. Visuospatial impairment
Visuospatial impairment can be suspected by seeing the patient missing the chair whilst trying to sit or struggling to find their way out of the consultation room. Features in the history such as minor road accidents or parking problems may imply problems with spatial judgement.
– 4.2.4.1. Visual neglect can be noticed in patients who do not comb one half of their hair or do not shave half of their face. Neglect can be tested by asking the patients to bisect a line or copy a double-headed daisy. Hemi-neglect implies damage to the contra-lateral parietal lobe. Simultagnosia is another feature of non-dominant parietal lobe damage that can be detected in tasks such as letter or shape cancellation in which patients are asked to cancel particular letters that are written in different sizes and shapes.
– 4.2.4.2. Construction apraxia, despite the terminology, is widely accepted as a useful marker of visuospatial impairment. The most widely utilised way of assessing this is by asking the patients to copy relatively complex shapes such as inter-locking pentagons or wired cubes. Alternatively, by seeing the patients drawing a clock face with hands pointing at a particular time, one obtains valuable information about their executive and visuospatial function.
– 4.2.4.3. Prosopagnosia can be tested by asking the patient to identify famous faces either in a formal test or from a celebrity magazine. It is an unusual feature that suggests posterior, non-dominant or bilateral hemisphere disease.
4.2.5. Apraxia
Apraxia is the inability to execute motor responses despite intact basic motor functions. A number of different types of apraxias have been described but it suffices to mention that presence of apraxia would indicate damage to the supplementary motor area and should be tested by the following:
– 4.2.5.1. Orobuccal apraxia: ask the patients to do a number of well learnt actions such as blowing, kissing, and yawning. Impairment in these actions is commonly seen in various types of aphasia.
– 4.2.5.2. Limb apraxia: ask the patients to demonstrate how they would stir sugar in a cup of coffee or ask them to mime to various gestures (both meaningful and meaningless)
4.2.6. Executive function
Executive function which traditionally localises to the frontal lobes can be tested in many different ways for example: asking the patient to estimate answers (How far is it from Cambridge to London?) or interpret proverbs. The value of such tests in localising problems is debatable, careful observation of the patient’s behaviour is usually more valuable.
Conclusion
The clinical assessment of a patient with dementia can be divided into 4 stages. The assessment requires time and some expertise and is aided by the use of short cognitive tests. A system to allow thorough assessment of patients is presented. Investigations such as neuroimaging, neuropsychological testing and cerebrospinal fluid testing should be determined by the initial clinical assessment of the patient.
- Brown J. The use and misuse of short cognitive tests in the diagnosis of dementia. J Neurol Neurosurg Psychiatry. 2015;86:680-5.
- Kipps CM, Hodges JR. Cognitive assessment for clinicians. J Neurol Neurosurg Psychiatry 2005;76 Suppl1:i22-30.
- Mion M et al. What the left and right anterior fusiform gyri tell us about semantic memory. Brain 2010;133(11):3256-68.
- Nestor PJ et al. Declarative memory impairments in Alzheimer’s disease and semantic dementia. Neuroimage 2006;30(3):1010-20.

