Abstract
The Clinical Frailty Scale (CFS) has been suggested as a tool to aid treatment escalation decisions for frontline clinicians during the COVID-19 pandemic. We discuss the concept of frailty and the role of the CFS. We explore the limitations of the CFS in people with stable long-term health conditions and suggest organisations implement the new guidance with caution. Training and guidance are available to help avoid poor decisions where the CFS is not appropriate.
The COVID-19 pandemic that emerged from China in December 2019 has now exceeded two million cases and caused over 140,000 deaths worldwide [1]. A severe complication of the SARS-CoV-2 infection is viral pneumonia, with 2.4% of patients requiring respiratory support in an intensive care unit (ICU) [2]. Early data from the UK suggests there is a 66% mortality associated with mechanical ventilation [3]. There is an increasing focus on early decision-making regarding the most appropriate level of care for individuals. This is driven by the need to achieve the best outcome for individual patients, but also may be informed by concerns over limited critical care resources.
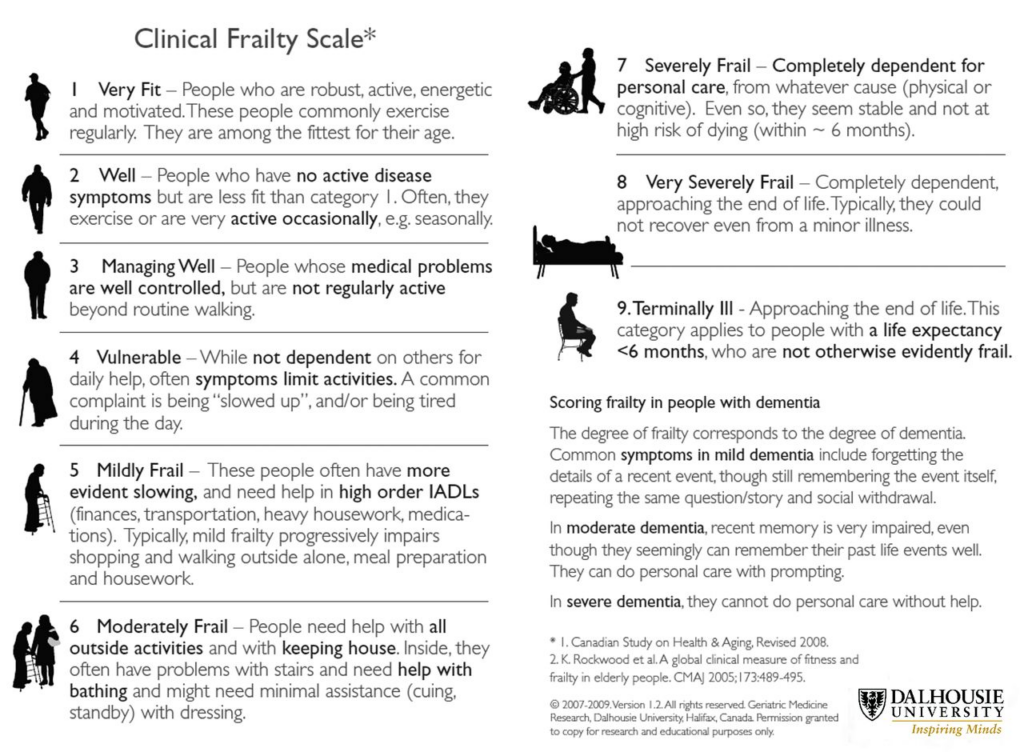
Clinicians are used to making decisions around admission to ICU and cardiopulmonary resuscitation (CPR) based on the likelihood of patient recovery or survival, to an outcome that is acceptable to them. On the 20th March 2020, National Institute for Health and Care Excellence (NICE) released guidance advising clinicians to use the clinical frailty scale (CFS) to guide these decisions (Figure 1 below) [4].
Figure 1: Clinical Frailty Scale
Frailty is a term commonly used in geriatric medicine to describe the accumulation of deficits across several physiological systems that lead to a state of increased vulnerability to adverse health outcomes and poor recovery after a stressor event, such as infection [5]. There are a number of models of frailty and tools to measure frailty. The CFS was devised as a simple clinical measure able to predict death and institutionalisation in older people [6]. Its use has been validated in people over 65 years and helps identify those who would most benefit from a comprehensive geriatric assessment. With time it has been adopted by other specialties to help guide decision-making about complex interventions such as renal replacement therapy, transcatheter aortic valve implantation, and emergency laparotomy. In the ICU setting, large observational studies have shown associations between high CFS scores and increased risk of extubation failure, early mortality, and discharge to long-term care [7-9].
The widespread application of CFS at the front door for the assessment of patients with COVID-19 led to concerns from patients and an outcry from disability advocacy groups [10,11]. These concerns primarily centred around the risk that clinicians may be influenced by the value that society places on disabled individuals’ lives. A misapplication of the CFS in patients with stable disabilities may lead to snap judgments based on high social care or support needs an individual may have.
NICE amended the guideline on 25th March 2020 to include the statement:
The CFS should not be used in younger people, people with stable long-term disabilities (for example, cerebral palsy), learning disability or autism. An individualised assessment is recommended in all cases where the CFS is not appropriate.
We believe there may still be a dilemma for doctors, and a risk of harm to patients. Does this brief caveat give new users of the CFS enough information to judge when its use is not appropriate? It is amply clear that the CFS is inappropriate for people with learning disabilities and autism. However, clinicians may be falsely reassured that outside of these stated examples, the CFS can be applied with confidence, even in those as young as 65 years.
Interpretation of the NICE amendment is hampered by the lack of a consistent concept of disability. Cerebral palsy is a health condition. Those who score highly on the CFS are almost certain to have disabilities. The CFS descriptors draw heavily on activities of daily living, and activity limitation is a key aspect of what constitutes a disability, according to the International Classification of Functioning, Disability, and Health (ICF) model [12]. Indeed there has been found to be a very high degree of overlap between frailty and disability (when defined as a dependency in at least one basic ADL) [13].
Perhaps the emphasis should be on the word stable. However, the CFS captures only a single point in time, suggested to be two weeks prior to the acute presentation. The presence or absence of an underlying trend to increased dependency consistent with frailty will not be apparent. In short, despite the appearance of this disclaimer, invalid use of the CFS may continue. If this happens it would not only be discriminatory, it would be ineffective and would result in making the wrong decisions about the best use of limited healthcare resources.
The CFS is not a direct measure of frailty, which is a physiological state. It is a series of roughly ordinal descriptions based mostly on the ‘activity’ domain. Its use is intuitive for clinicians as the descriptions are neatly described and are of recognisable phenotypes. Although the CFS functions well in older people as a surrogate for the likelihood of frailty, the score and the frailty are two different things. The assumption being made when a CFS score is used to predict a health outcome is that the interaction is mediated by frailty. When applied to younger people, or those for whom measuring activity would be confounded, the assumption is not valid. Many health conditions cause limitations in activity, such as arthritis, COPD, or anxiety, not necessarily via frailty. This is especially true in younger people and when the disease process is largely confined to a single body system. In someone with a previous traumatic brain injury, the link between needing assistance with finances, and chance of surviving an ICU admission may not be present at all, or may be present via another causal mechanism.
This highlights the risk of over-medicalising our decision-making. Learning from the social model of disability, and recognising the significance of social determinants of health, we should accept that ‘physiological vulnerability’ is not the only plausible causal link between activity limitation and health outcomes. This is important because if younger disabled people experience worse outcomes from hospitalisation, this may be for reasons other than physiological frailty. These reasons need to be exposed and challenged, not made into a self-fulfilling prophecy.
We also risk losing the trust of disabled people and those with long-term conditions, especially in the climate of an unprecedented pandemic. A policy for blanket administration of the CFS on admission may lead to an anchoring bias in subsequent decision making, even by clinicians aware of its limitations. This must be consciously resisted. Some people with activity limitations associated with a longstanding stable health condition may indeed be less likely to benefit from ICU admission. Ideally, this requires an individualised assessment by a clinician experienced in that particular patient group, in partnership with the individual. Availability of ideally experienced clinicians may be difficult to achieve during this pandemic. The use of a patient passport can ensure relevant information is available to all hospital clinicians to aid decision making. Effective advanced care planning reduces the need for decisions to be made in an emergency and enables the values and priorities of the individual to be incorporated fully into decision making.
As a way forward we suggest that applying the CFS appropriately requires an understanding of its underlying premise. Geriatricians are already familiar with this, but this new guidance may see staff groups who are not well versed in frailty concepts using the CFS under pressure. The team behind the CFS has recently published a helpful one-page ‘top tips’ guide which should be available in all clinical areas where the CFS is being used [14]. The NHS Clinical Frailty Network provides training in the use of the CFS [15]. Where Trusts have incorporated CFS into their local guidelines or documentation, the caveats to its use must be clearly indicated.
In conclusion, we suggest that in addition to the recent amendments to NICE guidance on the use of the CFS in making treatment escalation decisions, where there is doubt as to the applicability of the frailty concept, the CFS should not be used. There is no substitute for an individualised assessment by an experienced clinician.
References
- Johns Hopkins Coronavirus Resource Center. COVID-19 Map [Internet]. [cited 2020 Apr 17]. Available from: https://coronavirus.jhu.edu/map.html
- European Centre for Disease Prevention and Control. Coronavirus disease 2019 (COVID-19 ) in the EU/EEA and the UK – eighth update. 2020. [cited 2020 Apr 17]. Available from: https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-rapid-risk-assessment-coronavirus-disease-2019-eighth-update-8-april-2020.pdf
- Intensive Care National Audit and Research Centre. ICNARC report on COVID-19 in critical care. 2020. [cited 2020 Apr 17]. Available from: https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports
- National Institute for Health and Care Excellence. COVID-19 rapid guideline: critical care in adults. NICE, 2020.
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet 2013;381:752-62. https://doi.org/10.1016/S0140-6736(12)62167-9
- Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005;173:489-95. https://doi.org/10.1503/cmaj.050051
- Fernando SM, McIsaac DI, Rochwerg B, Bagshaw SM, Muscedere J, Munshi L, et al. Frailty and invasive mechanical ventilation: association with outcomes, extubation failure, and tracheostomy. Intensive Care Med 2019;45:1742-52. https://doi.org/10.1007/s00134-019-05795-8
- Guidet B, de Lange DW, Boumendil A, Leaver S, Watson X, Boulanger C, et al. The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med 2020;46:57-69. https://doi.org/10.1007/s00134-019-05853-1
- Le Maguet P, Roquilly A, Lasocki S, Asehnoune K, Carise E, Saint Martin M, et al. Prevalence and impact of frailty on mortality in elderly ICU patients: A prospective, multicenter, observational study. Intensive Care Med 2014;40:674-82. https://doi.org/10.1007/s00134-014-3253-4
- Baker D. No assumptions should be made about people’s quality of life irrespective of any disability – The BMJ [Internet]. [cited 2020 Apr 17]. Available from: https://blogs.bmj.com/bmj/2020/03/31/daniel-baker-no-assumptions-should-be-made-about-peoples-quality-of-life-irrespective-of-any-disability/
- Disability Rights UK. Covid 19 and the rights of disabled people. [Internet]. [cited 2020 Apr 17]. Available from: https://www.disabilityrightsuk.org/news/2020/april/covid-19-and-rights-disabled-people
- World Health Organisation. International Classification of Functioning, Disability, and Health: ICF. WHO, Geneva. 2001.
- Theou O, Rockwood MRH, Mitnitski A, Rockwood K. Disability and co-morbidity in relation to frailty: How much do they overlap? Arch Gerontol Geriatr. 2012;55:e1-e8. https://doi.org/10.1016/j.archger.2012.03.001
- Rockwood K, Fay S, Theou O, Dykes L. Top tips to help you use the Clinical Frailty Scale [Internet]. 2020 [cited 2020 Apr 17]. Available from: https://d29e30c9-ac68-433c-8256-f6f9c1d4a9ec.filesusr.com/ugd/bbd630_fd268508c43140d492168a59a57d2a75.pdf
- Specialised Clinical Frailty Network CFS Training [Internet]. [cited 2020 Apr 17]. Available from: https://www.scfn.org.uk/clinical-frailty-scale-training


