Abstract
COVID-19 and its aftermath highlight the importance of patient self-care and involvement in monitoring and improving their health. Resources to guide this are essential.
Our objective was to create a web-based patient education tool, to facilitate patient education and empowerment for people with epilepsy, multiple sclerosis and Parkinson’s disease, available without cost to patients, carers and clinicians.
This project was conducted within community and secondary neurology services. Patients and their carers were involved in designing, reviewing and revising the tool, as equal partners with clinicians and digital engineers.
A web-based design template was developed with graphics and links to enable patients to create personalised plans. Participants are patients, carers, clinicians (neurology consultants and specialist nurses), neurological charities, the London Neuroscience Clinical Network, NHS England and Shift.ms (a service design team with experience in creating digital services for individuals living with neurological conditions). Shift.ms conducted in-depth interviews. Clinicians used evidence from personal and PubMed databases. Shift.ms analysed and co-ordinated the responses, and designed the pilot tool.
Confidence College provides a delivery model for patient education relating to multiple sclerosis, epilepsy and Parkinson’s disease. It requires follow-up evaluation regarding uptake.
This web-based accessible patient empowerment tool has no limit on recurrent use, low maintenance costs and no additional costs in up-scaling the number of users. It is ideally suited for use during and after the COVID-19 pandemic.
Neurological disorders are amongst the most common chronic medical conditions, affecting an estimated 1 billion people worldwide. Of the 10 million in the UK, approximately 300,000 have active epilepsy, 137,000 have Parkinson’s disease, and 85,000 have multiple sclerosis (MS) [1]. Their burden outweighs their point prevalence, as reflected in measures such as disability-adjusted life years (DALY); for example, MS is the leading cause of non-traumatic neurological disability in young adults [2]. There is a significant treatment gap, widened since the pandemic [1]. A World Health Organization (WHO) survey of 155 countries found that almost half of the patients with chronic diseases missed their regular medical care and medications since COVID-19 pandemic began [3].
Patient empowerment enables people to gain control over decisions and actions affecting their health. It emphasises self-efficacy, self-awareness, confidence, coping skills and health literacy [4]. It aims to maximise quality of life and treatment effectiveness and is an important aim for both ethical and economic reasons: treatment non-adherence costs the Healthcare system in the United Kingdom alone an estimated £500 million per year [4], and these figures are echoed throughout the world.
Patient empowerment is primarily achieved through education and communication. Coaching and facilitated support groups improve outcomes and are part of development aims of government healthcare schemes. Increasing patient empowerment in a cost-effective and sustainable way is challenging, as it is difficult and costly to test and upscale potential methodologies. In neurology, barriers to face-to-face educational programmes include disabilities, mobility problems, employment, transport and mood, and currently the restrictions associated with the pandemic [3]. Telemedicine is now used in more than 60% of the world, and use of online resources during the COVID-19 pandemic potentially helps vulnerable individuals to receive care and education without compromising safety.
This project developed online modules to increase accuracy and depth of patient knowledge, designed to enable them to tailor individual health plans with clear goals. Developing evidence-based and user-friendly online patient-focused modules is time-consuming, and depends on collaboration between users and providers. This article outlines the process involved in producing these for three long-term neurological illnesses: multiple sclerosis, epilepsy and Parkinson’s disease.
Multiple sclerosis
Surveys of MS services by University College London partners (an academic health science network) highlight regional variations in standards of care and treatment gaps [5]. Individuals with MS, carers and families expressed a desire to improve their confidence in self-management but lacked the necessary tools. Confidence College evolved from this need, in collaboration with the London Neurology Network. Face-to-face courses are expensive in time and resources and are not accessible to all, especially during the COVID-19 pandemic. Online education offers universal access, and flexibility around employment, transport, and family commitments in this generally young population. The project was extended in a second phase to epilepsy and Parkinson’s disease.
Epilepsy
Roughly 19-44% of patients with epilepsy are non-adherent to treatment. This increases mortality risk threefold, and increases health costs. Past attempts to improve adherence targeted Applications and e-pill boxes, but forgetfulness is the problem in only 24% of patients. Other factors include perceived unaffordability, underestimating the need for medication, and side effects. An in-depth survey in patients with epilepsy highlighted knowledge gaps, with only 50% aware of sudden unexpected death in epilepsy, and 38% aware of status epilepticus. A greater awareness of the importance of medication adherence (98%) and seizure triggers (84%) suggests a major cognitive dissonance. Solutions to address this education imbalance require an interactive process. The Modular Service Package Epilepsy (MOSES) is an innovative comprehensive group educational module for epilepsy. A randomised trial in Germany showed it reduced seizures in participants [6]. In the UK, qualitative benefit was demonstrated but there were difficulties with attendance, memory and concentration [7]. Online interactive educational resources aim to reduce these barriers.
Parkinson’s disease
Parkinson’s disease is highly variable, so information is required on the many features and management strategies. While a holistic, multidisciplinary approach is desirable, a minority of patients have access to such care. Qualitative research suggests that many healthcare professionals consider self-management in Parkinson’s disease as important but identify barriers such as lack of resources [8], and research in this field is currently limited [9]. Face-to-face self-management courses are available through charities and peer-support. However, these have limited reach, depending on local availability, are not suitable for all, and are time limited.
Methods
Confidence College is a collaboration between NHS England, Shift.ms (a technological company developing patient-centred educational tools) and NeuroResponse® (a digital health community interest company) for the original MS work.
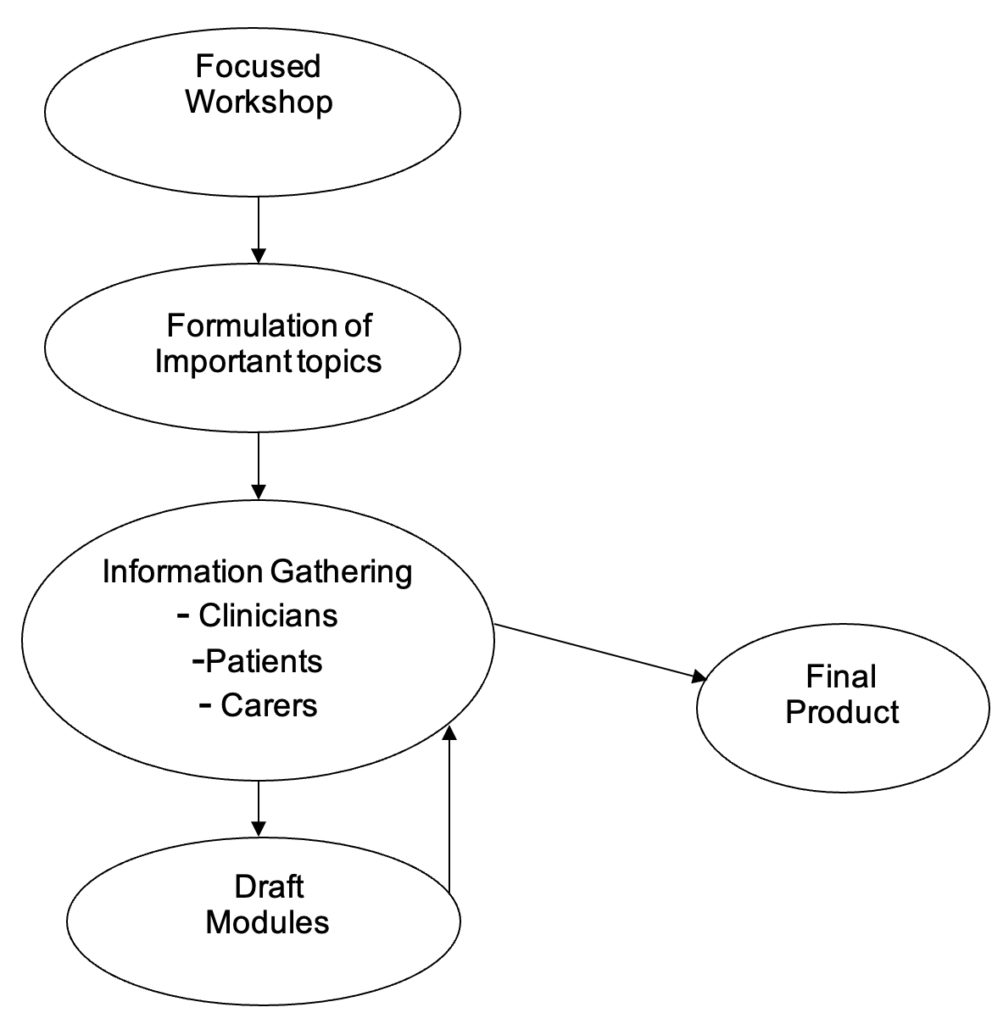
The development process was iterative, led by clinicians in each specialty, and involved reviewing the clinical information, individual interviews with patients regarding their chief concerns and information needs, and multi-disciplinary focus groups (Figure 1). Three topics for each condition were chosen for this pilot and developed into modules.
Results
Confidence College is accessible through http://www.confidencecollege.org.
Multiple slerosis
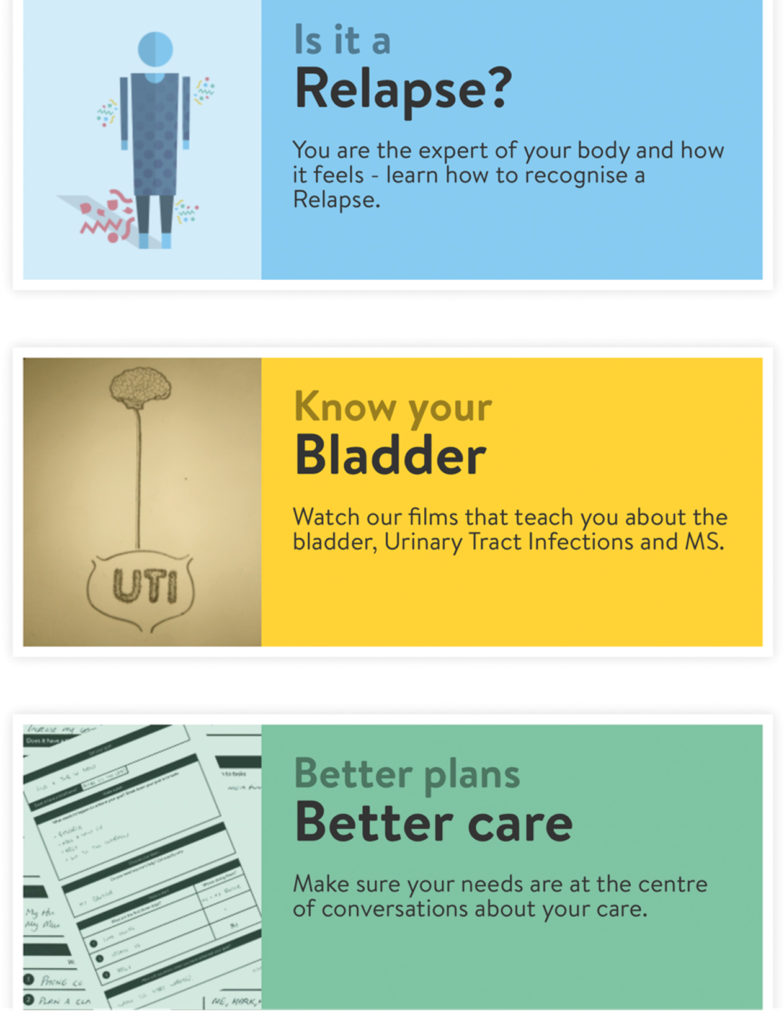
Is it a relapse?
Approximately 85% of individuals with MS present with relapses. Symptoms vary in presentation, severity and impact. They include weakness, visual disturbance, fatigue, cognitive problems, and any other symptom associated with MS. Relapses may have a major impact on family and colleagues. 67% of employed individuals require sickness leave, and 66% need additional support for routine daily tasks [10]. Relapses may occur with no precipitating factor and the speed and extent of recovery is often unpredictable, causing uncertainty.
It can be difficult for both individuals with MS and clinicians to identify a relapse. In this module, individuals and their families learn the definition of a relapse, how to self-monitor and how to differentiate between transient changes in background symptoms and an acute event. This section empowers patients to recognise features of a relapse and feel confident to report them to clinicians.
Know your bladder
Urinary tract infections are recorded in 13%-80% of patients with MS. They are amongst the top three reasons for hospitalisations in MS, accounting for 30%-50% of all in-patient admissions [11].
Recognising UTI symptoms in a person with MS can be difficult since typical symptoms may be absent and the presentation may be non-specific malaise. Symptoms suggestive of UTI in the general population (urinary frequency and incontinence) may reflect chronic lower urinary tract dysfunction and not signify infection.
The aim of this module is to promote adequate fluid intake, increase early detection of UTIs, use of a urine dipstick, and improve confidence in reporting symptoms to clinicians.
Better plans, better care
This section is shared across all three conditions and aims to empower patients by equipping them with confidence to express their needs to clinicians. It emphasises the need for individuals to identify personal goals that are unique and reflect their values. This potentially allows patients and carers to use their community and hospital consultations to maximum advantage.
Epilepsy
Living Well
This module gives illustrative information about what an epileptic seizure is, what happens to an individual with epilepsy, and what they can do to improve their epilepsy and care, in terms of lifestyle and medication.
It enables patients to develop their understanding of why and how seizures develop. This potentially reduces patients’ anxiety, particularly about the unpredictability of seizures. Better understanding seizures can have a positive impact on managing epilepsy, such as enhancing treatment adherence and reducing emergency department visits.
Mind Matters
The second module discusses links between epileptic seizures, mood and behavioural changes, and offers ways to cope with unpleasant thoughts.
Better plans, better care
Here, the care planning documents are discussed, allowing people to individualise them, ask the most useful questions at their neurological reviews, and establish epilepsy goals.
Parkinson’s disease
Living Well
This module has three sub-sections. The first, “What happens to the brain?” provides an illustrated overview of Parkinson’s disease, explains the motor and non-motor symptoms, and the unique disease impact experienced by individuals. The second, “Parkinson’s profile”, provides a template for individuals to create a structured record of their own illness, starting with how Parkinson’s affects them, and factors that worsen and alleviate their symptoms. The third, “What can I do?”, highlights evidence-based variables that patients can influence: medication, lifestyle and exercise. The aim is that patients become expert in understanding their condition, including differentiating between Parkinson’s symptoms and treatment side-effects.
Mind Matters
Mood is affected in at least 30% of patients [12]. This section, based on cognitive behavioural principles, focuses on understanding mood and unpleasant thoughts. Links to free online resources are provided to help patients and their carers formulate improvements.
Better plans, better care
This contains templates for a personal description of the patient’s life, and their goals, with the aim of personalising treatments and consultations.
Discussion
Confidence College is a collaboration between patients, carers and neurology clinicians, government and charities. It has developed online tools to support self-management in three neurological conditions: multiple sclerosis, epilepsy and Parkinson’s disease.
As part of the next stage of development, links to Confidence College will be offered to charity and NHS organisations, with the aim of embedding it into patient resources.
Conclusion
These tools facilitate patient empowerment by enabling individuals to gain a greater understanding of their condition, and through creating personalised health plans.
The use of Confidence College allows patients to prepare for consultations, or carry out in their own time and will not add to the length of consultations. Gathering data on usage is part of the next stage of the research.
Practice implications
This approach has the major advantage of having potential for wide scale use without additional costs: the structure and contents are enduring as it is hosted by NHS England but is available to all. It focuses on self-management of the most significant issues among people with chronic neurological conditions, rather than on new treatment development. These modules are however pilot tools and require long-term testing with a wide representative population to establish utility and impact on care and can be developed further. Future developments may involve adding other topics identified as valuable by the user community. If proven to add value, Confidence College could provide a template for such tools in other disease areas.
References
- Neurological Alliance. https://www.neural.org.uk/ (accessed March 2021). (n.d.).
- Jick SS, Li L, Falcone GJ, Vassilev ZP, Wallander MA. Epidemiology of multiple sclerosis: results from a large observational study in the UK. Journal of Neurology 2015;262:2033-41. https://doi.org/10.1007/s00415-015-7796-2
- World Health Organisation. Rapid assessment of service delivery for NCDs during the COVID-19 pandemic. https://www.who.int/publications/m/intem/rapid-assessment-of-service-delivery-for-ncds-during-the-covid-19-pandemic, (accessed March 2021). (n.d.).
- European Patients Forum. Patient empowerment. https://www.eu-patient.eu/news/New-Archive/patients-prescribe-the-epf-campaign-on-patient-empowerment/ (accessed November 2021). (n.d.).
- Porter B. National survey has important implications for MS nurse specialists. British Journal of Neuroscience Nursing 2006;2:272-3. https://doi.org/10.12968/bjnn.2006.2.6.21708
- May TW, Pfäfflin M. The efficacy of an educational treatment program for patients with epilepsy (MOSES): Results of a controlled, randomized study. Epilepsia 2002;43:539-49. https://doi.org/10.1046/j.1528-1157.2002.23801.x
- Ridsdale L, Philpott SJ, Krooupa AM, Morgan M. People with epilepsy obtain added value from education in groups: results of a qualitative study. European Journal of Neurology 2017;24:609-16. https://doi.org/10.1111/ene.13253
- Armstrong M, Tuijt R, Read J, Pigott J, Davies N, Manthorpe J, Frost R, Schrag A, Walters K. Health care professionals’ perspectives on self-management for people with Parkinson’s: qualitative findings from a UK study. BMC Geriatrics 2021;21:1. https://doi.org/10.1186/s12877-021-02678-w
- Pigott J, Kane E, Ambler, G, Walters, K, Schrag A. Systematic review and meta-analysis of clinical effectiveness of self-management interventions in Parkinson’s disease. BMC Geriatrics 2022;22:1-29. https://doi.org/10.1186/s12877-021-02656-2
- Nickerson M, Marrie RA. The multiple sclerosis relapse experience: Patient-reported outcomes from the North American Research Committee on Multiple Sclerosis (NARCOMS) Registry. BMC Neurology 2013;13:1-0. https://doi.org/10.1186/1471-2377-13-119
- Marrie RA, Elliott L, Marriott J, Cossoy M, Blanchard J, Tennakoon A., Yu N. Dramatically changing rates and reasons for hospitalization in multiple sclerosis. Neurology 2014;83:929-37. https://doi.org/10.1212/WNL.0000000000000753
- Gallagher DA, Lees AJ, Schrag A. What are the most important nonmotor symptoms in patients with Parkinson’s disease and are we missing them? Movement Disorders 2010;25:2493-500. https://doi.org/10.1002/mds.23394








