Abstract
Functional neurological disorders remain common presentations to both outpatient and inpatient NHS services, but little consensus exists with respect to how such services and clinical pathways for patients should be structured and should function. This article sets out a model for an integrated multidisciplinary approach that takes full account of the number of specialties involved, constraint on resources and time involved, and that has functioned well in the NHS despite a pandemic.
Functional neurological disorders (FND) are amongst the most common presentations in outpatient neurology clinics [1] leading to approximately 8000 new diagnoses per year in the UK alone [2,3]. Functional neurological disorders can be similar in appearance to disorders of the brain and nervous system but occur in the absence of organic pathology [4]. They can be identified through careful neurology assessment not just through exclusion of organic conditions but through inclusion of positive signs for diagnosis [5].
Despite its ubiquity, FND is both under-recognised and under-resourced in the NHS. This has changed in recent years with increasing research into the aetiology, assessment, and treatment of FND as well as the establishment of the FND Society for the development of understanding of these conditions [3]. However, prognosis often remains variable with one study finding quality of life ratings to be poorer in some FND presentations than with comparable organic conditions [6] and another identifying that 58% of a tracked cohort of FND patients were still reporting symptoms 12 years later [7].
One of the major issues in the treatment of FND has been lack of understanding of the condition amongst healthcare professionals. A synthesis of 11 qualitative studies into the experience of healthcare professionals (HCPs) in working with FND found common uncertainty in the management of FND which frequently led to moving the patient care onto another discipline [8]. The authors observed that this typically leads to a vicious cycle whereby patients are “passed from one professional to another but without receiving clear, honest information, or effective treatment”. They propose that clear clinical pathways are part of the solution to alleviate uncertainty in HCPs and improve treatment for patients with FND.
Development of the Exeter model as an integrated FND pathway
The NHS Five Year Forward View [9] sought to break down barriers in how care is provided between community and acute services, physical and mental health teams, and between health and social care. Devon Partnership NHS Trust responded to this with the development of the Integrated Psychological Medicine Approach which focused on establishing integrated pathways for long-term health conditions which might otherwise fall in the gap between physical and mental health services [10]. Existing Community Neuropsychology Services dedicated a small resource to working with functional neurological symptoms which evolved into an FND assessment and treatment service [11].
Over time this service worked in collaboration with Neurology and Rehabilitation specialities within the Royal Devon University Healthcare NHS Foundation Trust, developing shared expertise and trialling new initiatives [12]. This led to the emergence of a core group of interdisciplinary colleagues across both Trusts with an interest in improving care for people with FND. Following a regional conference in 2020 this group decided to form a virtual FND Multidisciplinary Team (MDT) to establish an integrated FND pathway across community and acute settings in physical and mental health services (See Figure 1).
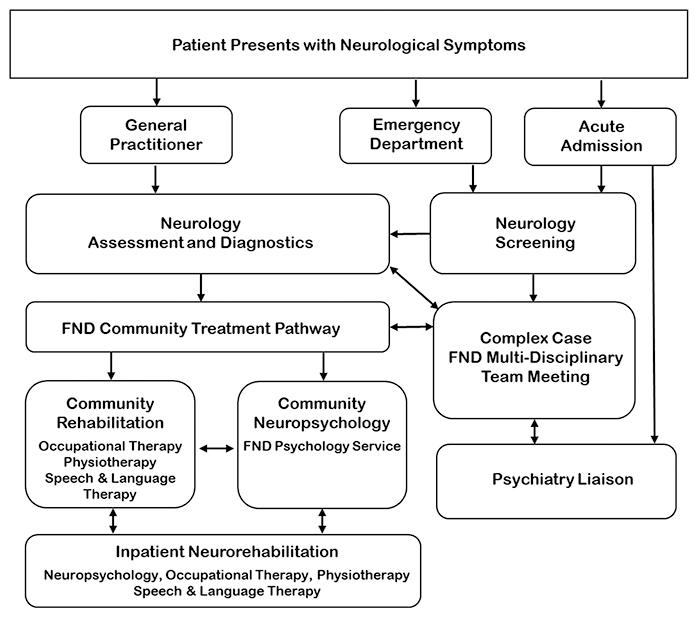
The underlying principle of the Exeter model is that the assessment and treatment of FND is part of the core business of acute and community services and therefore should be integrated with coherent pathways and clear roles. The clinical input can either be delivered in parallel across professions or as profession-specific episodes depending on patient need. The multidisciplinary nature of the team overseeing this pathway has been essential in order to capture patients presenting at different parts of the system, to develop coherent care-plans that reach across stepped-care, and to disseminate the full range of expertise required to support patients and families with FND. The pathway includes a twice monthly MDT meeting to; discuss the management of complex case presentations, reflect on the functioning of the pathway, establish new practices and protocols, and to develop new initiatives for raising awareness of FND within local healthcare settings.
The complex case FND MDT acts as the focal point in establishing, maintaining and developing the pathway. The major strength of the MDT is the value of what can emerge from the dialogue between professions as well as in the specialist role that each discipline contributes to the pathway:
Neurology
Neurologists are first and foremost involved in the diagnosis of FND. However, their role extends beyond this to treatment and in particular using clinical signs to explain to patients how well their nervous systems can work with the appropriate education and support. Patients with FND frequently develop new symptoms that may concern HCPs and the neurologist can offer clear advice as to whether this is or is not consistent with FND. Following MDT discussions neurologists are in a favourable position to offer effective second opinions for colleagues and arrange clinical review (usually face to face, but also via online consultations especially during the COVID pandemic). This is both intradepartmental where diagnosis remains challenging and also across specialties, in particular working alongside gastroenterologists and pain specialists. Finally, the neurologist has the opportunity to learn from others within the team about aspects they may not be familiar with, e.g. personality disorders thus enlisting expertise from psychiatry colleagues or complex psychosocial backgrounds from general practitioners.
Occupational therapy
Occupational therapists work with people with FND to enable meaningful participation in activities of daily living, including work-like and leisure occupations. This can take the form of interventions such as graded task practice, fatigue/symptom management, and vocational rehabilitation. Additional interventions also utilised, if necessary, can include compensatory aids, adaptations, and splinting. These interventions are individually assessed and managed to prevent the introduction of secondary problems that may prevent the restoration of normal movement and function. An advantage of the Exeter Model is that clinicians develop the skills and experience to support colleagues to use such compensatory techniques in a way that minimises the risk to the person’s recovery and avoids iatrogenic harm.
Physiotherapy
The role of the physiotherapist is pivotal at a number of levels and employs a specific skillset. Education is perhaps foremost: this involves reinforcing information from the neurologist and psychologist as well as lifestyle advice. Secondly, a more physiotherapy discrete approach should explore the effects different movement has on symptoms, encouraging normal physical activity, discouraging disadvantageous habitual postures, supporting graded activity and pragmatically yet sparingly and safely prescribing equipment. Thirdly, physiotherapists will often pick up positive signs of FND where the diagnosis is yet to be confirmed requiring effective communication with the whole team. The subtype of FND and individual circumstances of the patient will inform timing, type and intensity of intervention that a community physiotherapist offers as part of the MDT. The importance of physiotherapy expertise within the MDT has been examined in a number of studies [13,14,15,16,17].
Psychiatry liaison
Liaison psychiatrists and allied teams can usefully undertake a number of roles in the FND pathway. They are familiar with the hinterland between so called ‘physical’ and ‘mental’ healthcare delivery. Liaison psychiatrists and those other MDT colleagues working in liaison psychiatry teams can usefully undertake a number of roles in such a pathway. Firstly, they can help the wider team identify the presence of co-morbid mental disorders, or usefully exclude them. However, liaison psychiatrists do not see this as the be all and end all of their role. More subtle difficulties can be identified and a comprehensive ‘bio-psycho-social’ assessment can lead to a useful formulation which can be shared with the patient and the wider treating team. Liaison psychiatrists can act as ‘translators’ helping mental health professionals and those who work in medical environments to understand each other’s language and also the realities of what services are able to achieve. Patients with functional disorders may sometimes have a background of significant psychological trauma and this can be explored sensitively and made sense of, both for the patient and the other treating professionals. Behaviours that can be experienced as challenging or anxiety provoking for non-mental health professionals can be made sense of and useful risk assessment work can be undertaken.
Psychology
The role of clinical psychology and neuropsychology in FND can include: neuropsychological testing, bio-psycho-social assessment and formulation, and a range of interventions targeting potential psychological contributors to these conditions. The potential benefits of psychological interventions for FND are supported by an emerging evidence base [18,19,20,21]. These promising outcomes have been replicated locally in a pilot evaluation of Intensive Short-term Dynamic Psychotherapy (ISTDP) offered as part of our FND pathway [22] where we also offer Eye Movement Desensitisation and Reprocessing therapy (EMDR), Acceptance and Commitment Therapy (ACT), Cognitive Analytic Therapy (CAT) and Compassion Focused Therapy (CFT). FND psychoeducation and elements of these models are also incorporated into an online format for patients where a full course of psychological therapy is not indicated or appropriate. Overall, this set of psychotherapy models provides a range of potential mechanisms for ameliorating symptoms or improving quality of life through both implicit unconscious and explicit conscious processes [23].
Speech and language therapy
Speech and language therapists work with people with functional disorders of communication (including altered fluency, voice, articulation, prosody, accent and language), swallowing and cough. They can have a role to play in diagnosis; positively identifying functional symptoms through detailed assessment and liaising with the MDT regarding next steps where required. Patients are supported to understand the specific mechanisms underlying their symptoms and due attention is given to predisposing, precipitating and perpetuating factors in collaboration with MDT colleagues as appropriate. Although there is much work to be done to develop evidence-based treatments, detailed consensus recommendations have been published [24]. Therapy can vary significantly depending on the needs of the patient but may include; bringing the focus of attention to conditions under which pathways already function well, distraction, symptom and behaviour modification, specific exercises to release muscular tension and work to promote a greater sense of calm within the body and mind. Speech and language therapists working with FND within our service also draw on principles from a range of psychological approaches including ACT, Cognitive Behavioural Therapy (CBT) and Solution-Focused Brief Therapy.
Inpatient neurorehabilitation
There is an emerging literature on inpatient treatments and rehabilitation for FND. However, Consensus treatment guidelines have yet to be established. In this literature multidisciplinary team based interventions that include the role of physical therapy in addition to psychotherapy has increasingly been recognised [25,26,27,28]. There is preliminary evidence for the benefits of a multidisciplinary approach that utilises physiotherapy and psychological therapies such as; CBT, hypnosis and motor-retraining [27,29,30].
In relation to the specific NHS pathway described in this paper, Yates et al [31; unpublished poster presentation] carried out two retrospective studies comparing the differences in functional outcome measures of patients with FND and those with organic neurological disorders who were referred for inpatient multidisciplinary neurological rehabilitation. Both studies provided preliminary evidence that the inpatient rehabilitation pathway significantly improved the overall functioning of patients with FND over a four week period on measures of mobility; and that inpatient rehabilitation significantly reduced the complexity of need and intervention of patients. The clinical experience of the authors is that as the community FND pathway infrastructure has evolved the requirement for inpatient rehabilitation has substantially reduced.
Discussion
Operating in an emerging clinical field, we have also found it immensely helpful to extend our joint working to a wider range of colleagues and stakeholders. This has included the opportunity to work in collaboration with a local patient-led FND charity (FND FrieNDs) and with multidisciplinary colleagues across the South West in neighbouring NHS Trusts. This enables us to share and reflect on our service delivery as well as to learn from examples of good practice in the whole region.
A crucial aspect of the complex case MDT has been the ability to involve the wider network and especially general practitioners who are so often the core of effective FND care. These discussions are aimed at ensuring the right team of professionals are involved, which can lead to more productive and responsive discussions with the patient to ensure that they are getting the right care at the right time.
One area we are hoping to expand is the integration with Social Care Services. This will likely involve representation at the complex case MDT and joint work to ensure that our colleagues in Social Care are FND aware. Similar projects for raising awareness of FND have already been instigated in our local inpatient settings and are planned for our emergency department.
Conclusions
In order to address historic disparities in care for FND we found it was essential to work across professional disciplines and establish an integrated pathway of care across acute and community services. This has involved developing and sharing FND expertise, raising awareness of the condition in all settings, partnership working with our third sector colleagues, and finding time to meet regularly as a multidisciplinary group seeking better care for FND.
The Exeter model evolved from the premise that FND input should not be seen as the province of only specifically commissioned services or regional providers. People with FND and their carers deserve well-designed services that can locally meet the needs of the majority of patients through providing continuity of care and effective multidisciplinary input. We fully support the need for FND to be better resourced nationally through specific commissioning but would also encourage colleagues not to wait until funding has been secured before working together to develop pathways. Whilst we still have much to learn about effective support for people with FND, we have found the opportunity to work together on the pathway as a multidisciplinary group to be hugely enjoyable and professionally highly rewarding.
References
- Stone J, Carson A, Duncan R, Roberts R, Warlow C, Hibberd C, Coleman R, Cull R, Murray G, Pelosi A, Cavanagh J. Who is referred to neurology clinics?-the diagnoses made in 3781 new patients. Clinical neurology and neurosurgery. 2010 Nov 1;112(9):747-51. https://doi.org/10.1016/j.clineuro.2010.05.011
- Carson A, Lehn A. Epidemiology. In: Hallett M, Stone J, Carson A. (eds). Handbook of clinical neurology: Vol 139: Functional neurologic disorders. Elsevier, 2016:47-60. https://doi.org/10.1016/B978-0-12-801772-2.00005-9
- Bennett K, Diamond C, Hoeritzauer I, Gardiner P, McWhirter L, Carson A, Stone J. A practical review of functional neurological disorder (FND) for the general physician. Clinical Medicine. 2021 Jan;21(1):28. https://doi.org/10.7861/clinmed.2020-0987
- Reuber M, Howlett S, Khan A, Grünewald RA. Non-epileptic seizures and other functional neurological symptoms: predisposing, precipitating, and perpetuating factors. Psychosomatics. 2007 May 1;48(3):230-85. https://doi.org/10.1176/appi.psy.48.3.230
- Finkelstein SA, Cortel‐LeBlanc MA, Cortel‐LeBlanc A, Stone J. Functional neurological disorder in the emergency department. Academic Emergency Medicine. 2021 Apr 18. https://doi.org/10.1111/acem.14263
- Testa SM, Schefft BK, Szaflarski JP, Yeh HS, Privitera MD. Mood, personality, and health‐related quality of life in epileptic and psychogenic seizure disorders. Epilepsia. 2007 May;48(5):973-82. https://doi.org/10.1111/j.1528-1167.2006.00965.x
- Stone J, Sharpe M, Rothwell PM, Warlow CP. The 12 year prognosis of unilateral functional weakness and sensory disturbance. Journal of Neurology, Neurosurgery & Psychiatry. 2003 May 1;74(5):591-6. https://doi.org/10.1136/jnnp.74.5.591
- Barnett C, Davis R, Mitchell C, Tyson S. The vicious cycle of functional neurological disorders: a synthesis of healthcare professionals’ views on working with patients with functional neurological disorder. Disability and rehabilitation. 2020 Sep 22:1-0. https://doi.org/10.1080/09638288.2020.1822935
- England NHS. The NHS five year forward view. 2014. London: NHS England.
- Devon Partnership NHS Trust. An Integrated Psychological Medicine Service for Devon: Symptom Management. 2016. Exeter: Devon Partnership NHS Trust.
- Russell L, Carrick R, Turner A, Yates, P. The Development of a Functional Neurological Symptoms Service within a National Health Service Setting. The Neuropsychologist. 2019 April 7.
- Butler L, Russell L, Yates P. Outcome of Physiotherapy Pilot within the Functional Neurological Symptoms Service for Reduction of Hospital Admission. 2019. Exeter: Devon Partnership NHS Trust.
- Czarnecki K, Thompson JM, Seime R, Geda YE, Duffy JR, Ahlskog JE. Functional movement disorders: successful treatment with a physical therapy rehabilitation protocol. Parkinsonism & related disorders. 2012 Mar 1;18(3):247-51. https://doi.org/10.1016/j.parkreldis.2011.10.011
- Jordbru AA, Smedstad LM, Klungsøyr O, Martinsen EW. Psychogenic gait disorder: a randomized controlled trial of physical rehabilitation with one-year follow-up. Journal of rehabilitation medicine. 2014 Feb 5;46(2):181-7. https://doi.org/10.2340/16501977-1246
- Nielsen G, Ricciardi L, Demartini B, Hunter R, Joyce E, Edwards MJ. Outcomes of a 5-day physiotherapy programme for functional (psychogenic) motor disorders. Journal of neurology. 2015 Mar;262(3):674-81. https://doi.org/10.1007/s00415-014-7631-1
- Nielsen G, Buszewicz M, Stevenson F, Hunter R, Holt K, Dudziec M, Ricciardi L, Marsden J, Joyce E, Edwards MJ. Randomised feasibility study of physiotherapy for patients with functional motor symptoms. Journal of Neurology, Neurosurgery & Psychiatry. 2017 Jun 1;88(6):484-90. https://doi.org/10.1136/jnnp-2016-314408
- Petrochilos P, Elmalem MS, Patel D, Louissaint H, Hayward K, Ranu J, Selai C. Outcomes of a 5-week individualised MDT outpatient (day-patient) treatment programme for functional neurological symptom disorder (FNSD). Journal of neurology. 2020 Sep;267(9):2655-66. https://doi.org/10.1007/s00415-020-09874-5
- Gutkin M, McLean L, Brown R, Kanaan RA. Systematic review of psychotherapy for adults with functional neurological disorder. Journal of Neurology, Neurosurgery & Psychiatry. 2021 Jan 1;92(1):36-44. https://doi.org/10.1136/jnnp-2019-321926
- LaFrance WC, Baird GL, Barry JJ, Blum AS, Webb AF, Keitner GI, Machan JT, Miller I, Szaflarski JP. Multicenter pilot treatment trial for psychogenic nonepileptic seizures: a randomized clinical trial. JAMA psychiatry. 2014 Sep 1;71(9):997-1005. https://doi.org/10.1001/jamapsychiatry.2014.817
- Goldstein LH, Robinson EJ, Mellers JD, Stone J, Carson A, Reuber M, Medford N, McCrone P, Murray J, Richardson MP, Pilecka I. Cognitive behavioural therapy for adults with dissociative seizures (CODES): a pragmatic, multicentre, randomised controlled trial. The Lancet Psychiatry. 2020 Jun 1;7(6):491-505.
- Russell L, Abbass A, Allder S. A review of the treatment of functional neurological disorder with intensive short-term dynamic psychotherapy. Epilepsy & Behavior. 2022 May 1;130:108657. https://doi.org/10.1016/j.yebeh.2022.108657
- Russell L, Turner A, Yates P. A Preliminary Evaluation of the Application of Intensive Short-Term Dynamic Psychotherapy within a Functional Neurological Symptoms Service. The Neuropsychologist. 2017 Oct 4:25-32.
- Russell L, Carrick R. Psychological Therapy for Functional Neurological Symptoms. Conference Presentation: Developing Service Pathways for Functional Neurological Disorder, January 24, 2020, Exeter, England.
- Baker J, Barnett C, Cavalli L, Dietrich M, Dixon L, Duffy JR, Elias A, Fraser DE, Freeburn JL, Gregory C, McKenzie K. Management of functional communication, swallowing, cough and related disorders: consensus recommendations for speech and language therapy. Journal of Neurology, Neurosurgery & Psychiatry. 2021 Oct 1;92(10):1112-25. https://doi.org/10.1136/jnnp-2021-326767
- Saifee TA, Kassavetis P, Pareés I, Kojovic M, Fisher L, Morton L, Foong J, Price G, Joyce EM, Edwards MJ. Inpatient treatment of functional motor symptoms: a long-term follow-up study. Journal of neurology. 2012 Sep;259(9):1958-63. https://doi.org/10.1007/s00415-012-6530-6
- McCormack R, Moriarty J, Mellers JD, Shotbolt P, Pastena R, Landes N, Goldstein L, Fleminger S, David AS. Specialist inpatient treatment for severe motor conversion disorder: a retrospective comparative study. Journal of Neurology, Neurosurgery & Psychiatry. 2014 Aug 1;85(8):895-900. https://doi.org/10.1136/jnnp-2013-305716
- Jacob AE, Kaelin DL, Roach AR, Ziegler CH, LaFaver K. Motor retraining (MoRe) for functional movement disorders: outcomes from a 1-week multidisciplinary rehabilitation program. PM&R. 2018 Nov 1;10(11):1164-72. https://doi.org/10.1016/j.pmrj.2018.05.011
- McKee K, Glass S, Adams C, Stephen CD, King F, Parlman K, Perez DL, Kontos N. The inpatient assessment and management of motor functional neurological disorders: an interdisciplinary perspective. Psychosomatics. 2018 Jul 1;59(4):358-68. https://doi.org/10.1016/j.psym.2017.12.006
- Humblestone S, Roelofs J, Selai C, Moutoussis M. Queen Square Guided Self Help for Functional Neurological Symptom Disorder. Downloaded 2021, February. https://doi.org/10.31234/osf.io/yd598
- Moene FC, Spinhoven P, Hoogduin KA, van Dyck R. A randomised controlled clinical trial on the additional effect of hypnosis in a comprehensive treatment programme for in-patients with conversion disorder of the motor type. Psychotherapy and psychosomatics. 2002;71(2):66-76. https://doi.org/10.1159/000049348
- Yates P, Harrower T, Parry E, Dendle J. Two studies of inpatient rehabilitation outcomes for patients with functional neurological disorders (FND). Treatment Abstracts: Poster presented at: 3rd International Conference on Functional (Psychogenic) Neurological Disorders, September 6-8, 2017 Edinburgh, Scotland.








