Abstract
Insomnia is thought to affect 5-10% of the general population and is associated with daytime impairment and distress. Insomniacs were found to have a higher risk of poor cardiometabolic health. However, this association is only significant if they have both insomnia and objective short sleep duration.
Key points
- Self-reported sleep duration does not always correlate with objective sleep loss.
- The mis-match between subjective and objective sleep duration is due in part to sleep state misperception.
- Only a relatively small percentage of insomniacs with objective short sleep duration have high risk of cardiometabolic disease.
Introduction
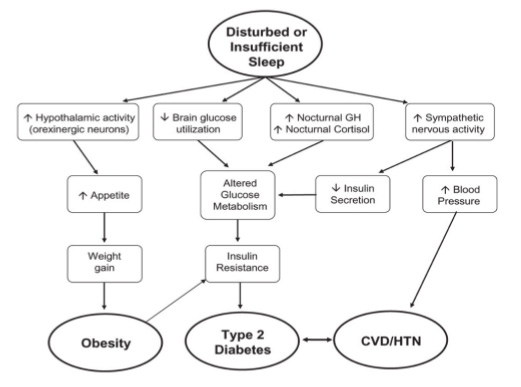
Cardiometabolic health (CMH) is an umbrella term encompassing the cardiovascular and metabolic systems. Risk factors for worse CMH include insulin resistance, hypertension, abdominal obesity and dyslipidaemia. There are substantial economic and individual burdens associated with poor CMH. It is well established that poor diet and physical inactivity have causative roles, but emerging evidence suggests that poor sleep quality and sleep deprivation also increase the risk of cardiometabolic disease (Figure 1). Sleep disturbance could be due to societal pressure such as shift work or due to specific sleep disorders such as obstructive sleep apnoea, restless leg syndrome or insomnia disorder.1
Insomnia remains the commonest sleep disorder affecting approximately 5-10% of the general population. Whilst commonly presenting alongside other medical and psychiatric disorders, insomnia is now recognised as a separate disorder in its own right. Insomnia disorder is defined as difficulty falling and staying asleep despite adequate circumstances for sleep with subsequent daytime distress and impairment. Most patients complain of prolonged, frustrating awakenings during the sleep period.2
Sleep duration can be measured subjectively using sleep diaries or objectively using the gold standard of video polysomnography (psg). Accelerometry can also be used as an objective measure, albeit less sensitive than video psg. The diagnosis of insomnia is based on poor subjective sleep quality with daytime distress rather than objectively measured sleep fragmentation. In fact, there is often a mismatch between subjective and objective sleep duration and patients may significantly underestimate total sleep time – known as “sleep state misperception”.3
Sleep misperception is considered common within chronic insomnia. Various factors have been suggested to play a role in it, including altered perceptual time processing, pre-sleep worry and subtle EEG changes that might not be well measured with PSG. This has led to increasing interest in Insomniacs with objective normal sleep duration compared to those with objectively short sleep. Whether the underestimation of sleep duration in insomniacs deserves a separate diagnostic category remains under debate. Sleep misperception in itself is associated with depression, anxiety and worse coping resources. In addition, people with different insomnia phenotypes may respond to different treatment approaches.3 Here we will describe the relationship between metabolic syndromes and insomnia with both subjective and objective short sleep durations.
Insomnia and diabetes
Sleep disturbance is significantly associated with abnormal glucose regulation and higher incidence of type 2 diabetes (T2D).4 However, this association could well be confounded by other factors, such as socioeconomic status, alcohol, smoking and psychiatric distress which will all increase the risk of both insomnia symptoms and T2D. A prospective cohort study investigated possible confounders and the cumulative effect of insomnia over 20 years. The results suggested that the association between sleep and diabetes were largely confounded, especially by psychiatric distress which needs further investigation.5
In many research studies looking at insomnia and diabetes, sleep disturbance was measured by questionnaires and obstructive sleep apnoea was not controlled for. However, an important, population-based study carried out by Vgontzas et al.6 measured sleep objectively with PSG alongside self-report sleep diaries. They found that compared to those who slept >6 hours per night, those who had insomnia and objectively slept for ≤5 hours per night had an approximately 300% increased risk of diabetes (OR 2.95, 95% CI 1.24-7.03). While those who have no insomnia and sleep <5 hours per night only had a 10% increased risk of diabetes (OR 1.10, 95% CI 0.68-1.79). There was also a positive correlation between the severity of insomnia and the likelihood of developing diabetes. These findings suggest that objective sleep measurement in insomnia could be a useful marker for its severity and impact upon glucose regulation. The cross sectional nature of the study means a causal relationship cannot be determined.
Insomnia and cardiorespiratory fitness
A large number of studies have focused on the relationship between insomnia and mental disorders, but few have investigated the effect of insomnia on respiratory function. A large cross sectional population study examined the association between insomnia and peak oxygen uptake (VO2peak) measurement of cardiorespiratory fitness. Participants were asked to walk/run at an increasing speed on a treadmill until exhaustion and VO2peak levels were determined. As poor cardiorespiratory fitness is also closely associated with poor cardiometabolic heath, even in the absence of insomnia. Strand et al. controlled for various potentially confounding factors including BMI, blood pressure, resting heart rate, total serum cholesterol and physical activity index. They observed reduced VO2peak in people with insomnia compared to those without. The association between repeated awakenings throughout the night and VO2peak was found to be the strongest when compared to early awakening and daytime sleepiness. They also identified an inverse association between the severity of insomnia and VO2peak. As cardiorespiratory fitness is a strong risk predictor of CVD, we can anticipate a negative correlation between the severity of insomnia and cardiometabolic health.7
In contrast, Bonnet and Arand8 measured overall oxygen use in insomniacs and reported an increased VO2 in people with primary insomnia compared to the controls across 24 hours. They also gave 12 adults without insomnia 400mg of caffeine three times daily for one week and participants developed insomnia symptoms including poor sleep, increased sleep latency, fatigue and anxiety. Their metabolic rates were significantly elevated as indicated by the increased VO2 level.
These two studies suggests that people with insomnia have a higher level of oxygen consumption throughout the day compared to those without insomnia. However, their peak oxygen consumption is reduced under intensive exercise, suggesting their cardiometabolic function is only reduced under physical stress.
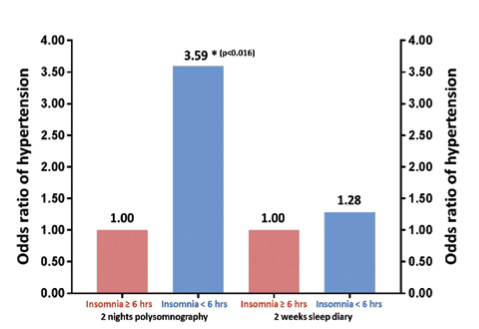
Insomnia and cardiovascular disease CVD is the worldwide leading cause of mortality.9 Hypertension is a common risk factor for CVD. The negative impact of sleep disturbance on blood pressure has already been described in many epidemiological studies. Most of these only examined insomnia or short sleep based on self-report diaries.9 However Vgontzas et al.10 carried out a population based cross sectional study which examined the joint effects of insomnia and objective sleep duration on hypertension. The combination of chronic insomnia (insomnia complaint ≥1 year) and a sleep duration of ≤5 hours per night was found to be associated with a 500% increased risk of hypertension compared to those without insomnia and sleep for >6 hours per night. The risk of hypertension was only increased by 13% in those who had no insomnia and slept <5 hours per night. However, objective short sleep duration or insomnia alone were not found to be significantly associated with a higher risk of hypertension. Bertisch et al.9 did a similar study which investigated the association between insomnia with objective short sleep duration and risk of CVD. They have found that participants have a 29% higher risk of incident CVD when they have insomnia with an objective sleep duration of <6 hours per night, while the association between incident CVD and subjective short sleep duration is not significant. These studies provide evidence that insomniacs with objective short sleep duration are more vulnerable to CVD but not those with only a subjective short sleep time. Therefore, both objective sleep duration and insomnia symptoms seem important for risk assessments.9
An American study reported higher CVD events in those with insomnia complaints every day compared to those without any complaints, and a Swedish study reported that those who had difficulty initiating sleep had a higher risk of coronary artery disease mortality.1 Poor subjective sleep quality was associated with higher risk of hypertension. However, a cross sectional observation study by Bathgate et al.11 reported that only objective short sleep duration was associated with a higher risk of hypertension, while the relationship was not significant with subjective sleep duration. Another study reported that lower objective sleep efficiency was strongly associated with higher prevalence of prehypertension.1
Based on the above studies, insomnia with objective, but not subjective, short sleep duration is associated with higher risk of CVD and hypertension.
Insomnia and obesity
Obesity is a worldwide problem, mainly caused by excess calorie intake and physical inactivity. It is associated with CVD, stroke, T2D and psychological problems.
Experimental data reported an increased level of appetite- stimulating ghrelin, decreased level of appetite-inhibiting leptin and glucose intolerance in sleep-restricted individuals.12 Many cohort, cross-sectional and longitudinal studies have determined an association between poor sleep and obesity.12 However, the main limitation of these studies is the lack of objective sleep measurements. Studies on sleep and obesity have been summarised in a review by Tatjana Crönlein.12
In contrast to the large number of studies on other sleep disorders and obesity, limited studies have investigated the association between insomnia disorder and obesity. Huang et al.13 measured sleep using PSG in Chinese insomniac patients and healthy controls but found no significant difference in their BMI. Another study by Crönlein et al.14 found that German patients with severe chronic insomnia even had lower BMI than controls.
Conclusion Self-reported sleep duration is sufficient for a diagnosis for insomnia disorder, however it clearly does not always correlate with objective sleep loss due in part to sleep state misperception. There is an increased risk of hypertension and diabetes in those with insomnia but ONLY if they have an objectively short sleep time as well, this is approximately 10% of those who suffer from insomnia.15 There is no clear link between obesity and insomnia.
References
- Knutson KL. Sleep duration and cardiometabolic risk: a review of the epidemiologic evidence. Best practice & research Clinical endocrinology & metabolism. 2010;24:731-743.
- Roth T. Insomnia: Definition, Prevalence, Etiology, and Consequences. Journal of Clinical Sleep Medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2007;3:S7-S10.
- Fernandez-Mendoza J, Calhoun SL, Bixler EO, Karataraki M, Liao D, Vela-Bueno A, Ramos-Platon MJ, Sauder KA, Basta M, Vgontzas AN. Sleep Misperception and Chronic Insomnia in the General Population: The Role of Objective Sleep Duration and Psychological Profiles. Psychosomatic medicine. 2011;73:88-97.
- Knutson KL, Ryden AM, Mander BA, Van Cauter E. Role of sleep duration and quality in the risk and severity of type 2 diabetes mellitus. Archives of Internal Medicine. 2006;166:1768-1774.
- Green MJ, Espie CA, Popham F, Robertson T, Benzeval M. Insomnia symptoms as a cause of type 2 diabetes Incidence: a 20 year cohort study. BMC Psychiatry. 2017;17:94.
- Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Bixler EO. Insomnia With Objective Short Sleep Duration Is Associated With Type 2 Diabetes: A population- based study. Diabetes Care. 2009;32:1980-1985.
- Strand LB, Laugsand LE, Wisløff U, Nes BM, Vatten L, Janszky I. Insomnia Symptoms and Cardiorespiratory Fitness in Healthy Individuals: The Nord-Trøndelag Health Study (HUNT). Sleep. 2013;36:99-108C.
- Bonnet MH, Arand DL. Insomnia, metabolic rate and sleep restoration. Journal of internal medicine. 2003;254:23-31.
- Bertisch SM, Pollock BD, Mittleman MA, Buysse DJ, Bazzano LA, Gottlieb DJ, Redline S. Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: Sleep Heart Health Study. Sleep. 2018;41.
- Vgontzas AN, Liao D, Bixler EO, Chrousos GP, Vela-Bueno A. Insomnia with Objective Short Sleep Duration is Associated with a High Risk for Hypertension. Sleep. 2009;32:491-497.
- Bathgate CJ, Edinger JD, Wyatt JK, Krystal AD. Objective but Not Subjective Short Sleep Duration Associated with Increased Risk for Hypertension in Individuals with Insomnia. Sleep. 2016;39:1037-1045.
- Cronlein T. Insomnia and obesity. Current opinion in psychiatry. 2016;29:409- 412.
- Huang L, Zhou J, Sun Y, Li Z, Lei F, Zhou G, Tang X. Polysomnographically determined sleep and body mass index in patients with insomnia. Psychiatry research. 2013;209:540-544.
- Cronlein T, Langguth B, Busch V, Rupprecht R, Wetter TC. Severe chronic insomnia is not associated with higher body mass index. Journal of sleep research. 2015;24:514-517.
- Vgontzas AN, Fernandez-Mendoza J, Liao D, Bixler EO. Insomnia with Objective Short Sleep Duration: the Most Biologically Severe Phenotype of the Disorder. Sleep medicine reviews. 2013;17:241-254.