Summary
- Individuals with Down syndrome are at high risk of developing Alzheimer’s disease (AD)
- Multiple levels of evidence (genetic, histopathological, imaging and clinical) suggest that the study of AD in Down syndrome will inform our understanding of sporadic AD.
- Key areas for research of AD in Down syndrome include (i) better identification and study of pre-symptomatic AD and (ii) improving predictive validity in models of AD
- New initiatives to research AD in Down syndrome offer exciting opportunities for the benefits of detailed clinical studies and robust trials, performed almost exclusively on AD in the general population to date, to be brought to the DS population.
Abbreviations: Aβ: amyloid-beta protein; AD: Alzheimer’s disease; APP: amyloid precursor protein; DS: Down syndrome
Introduction
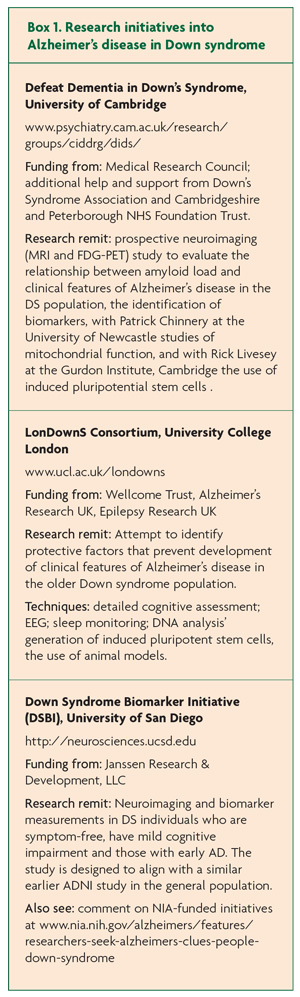
Individuals with Down syndrome (DS) have a high risk of developing Alzheimer neuropathology which, in later life, gives rise to the symptoms of Alzheimer’s disease (AD).1,2,3 In the context of the improving life expectancy of people with DS, new research initiatives have been launched with the specific remit of investigating this relationship (Box 1). However, the research investment into DS also reflects the aspiration that the study of AD in DS will bring benefit to patients with AD whether or not they have DS. In this article we discuss the rationale for this and whether such research can inform about AD more widely.
Comparison of AD in people with and without Down syndrome
There is convincing evidence at multiple levels that the study of AD in people with DS could inform our understanding of sporadic AD.
i. Histopathology
Historical studies of Alzheimer pathology in people with DS were complicated by selection bias, often limited clinical information and without karyotypic confirmation of DS. Since these early studies, detailed neuropathological accounts have described and quantified neuropathology in DS and conclusively demonstrated the same pathological hallmarks of amyloid plaques and neurofibrillary tangles as in sporadic AD.1 Alzheimer pathology is virtually ubiquitous in the DS population ≥30 years, but time to onset of clinical features is highly variable.7 The disparity between AD neuropathology and clinical symptoms is also seen in the general population, but is particularly striking in the DS population, and this is the subject of planned research in the LonDownS project (see Box 1).
ii. Genetics
The observation that individuals with complete trisomy 21 (accounting for the vast majority of people with DS) developed early-onset Alzheimer pathology led to studies that localised the amyloid precursor protein (APP) on chromosome 21.4 In addition, in later studies disomic individuals with AD were found with three copies of the APP gene due to a de novo interstitial chromosomal duplication and, in other cases, mutations were observed in the APP gene in kindreds with early-onset autosomal dominant AD.5 Such inherited mutations affect the processing of amyloid beta in vitro and, it is hypothesised, this abnormal processing leads to accumulation of pathogenic oligomers. Together these various observations both in DS and in the general population led to the amyloid cascade hypothesis of AD.6 Experimental models of trisomy 21, overproduction of APP and accumulation of Aβ species each convincingly recapitulate patterns of in vitro protein pathophysiology seen with autosomal-dominant forms of AD.2 However, these autosomal dominant causes only represent a small minority (<1%) of all cases of AD and it is considered unlikely that they represent the extent of the heterogeneity of disease mechanisms in the full spectrum of sporadic AD. In contrast, support for common pathophysiological mechanisms comes from recent genome-wide association studies. These have demonstrated shared genetic risk factors for sporadic AD and early disease progression of AD in DS.5
iii. Imaging
A recent cross-sectional MRI study demonstrated smaller whole brain, temporal lobe and hippocampal volumes in DS individuals with AD compared with DS controls.8 These findings are equivalent to those seen in studies of AD in the general population, in which early and significant volume reductions in medial temporal lobe structures are often seen, a finding supplemented by additional longitudinal data.9,10 Following the completion of a proof of principle study11 a neuroimaging study of people with DS over 30 years using PET imaging to detect cerebral amyloid binding combined with its cerebral localisation using structural MRI is being undertaken by the Cambridge DS group to investigate the relationship between cerebral amyloid deposition, cerebral atrophy and clinical symptoms.
iv. Clinical
Age-specific prevalence rates of AD in people with DS increase from a few percent in the 30’s, to 40% or higher in the 50’s and 60’s.3 However, the characteristic impairments in early stages of AD are important differences in DS. ‘Forgetfulness’ and episodic memory impairments occur early in AD in the general population, whereas changes in personality and behaviour, and objective impairments in executive function are often the earliest signs in DS.3,6 Just as for the diagnosis of AD in the general population, the most valuable data often comes from informant or carer interviews, and in the absence of easily-applied bedside cognitive tests, such information contributes to a greater extent towards making diagnosis of AD in DS. One difficulty comparing across studies is that neuropsychological assessments used in the study of non-DS individuals cannot readily be applied to the DS population without significant adjustments. These differences in the clinical features of AD in DS and non-DS individuals are interesting topics for further investigation. For example, why does frontal dysfunction occur preferentially and early in DS individuals? Does this reflect different AD pathophysiology or, alternatively, an interaction with the developmentally-determined small reserve capacity of the frontal lobes in DS?
Why study AD in Down syndrome?
Clinical trials in AD have been uniformly disappointing and no disease-modifying therapies for AD are yet available. A series of monoclonal antibodies demonstrated to specifically and potently interfere with deposition of the pathological substrate amyloid-beta in vitro and in rodent models have failed to significantly alter disease progression or severity. These disappointing results demonstrate a critical need for novel experimental approaches to the study of AD with the aim of developing effective preventative therapeutic agents. For this to be possible two specific problems must be overcome. DS provides a means to address these and by doing so, effective treatments could be developed that would bring benefit to people with DS and inform our understanding of sporadic AD. We identify these problems as:
i. The identification and study of pre-symptomatic AD
Accurate identification of pre-symptomatic individuals, either with AD pathology or before, is relevant to understanding the natural course of disease progression, for the identification of risk factors for progression to clinical symptoms, and for the early application of potential disease-modifying agents. Although AD is common, it is by no means ubiquitous and there is good evidence for healthy ageing without AD. Some studies have addressed this issue of early identification by using individuals with mild cognitive impairment, in which there is objective evidence of limited cognitive (usually memory) impairment but without meeting criteria for the diagnosis of AD. However, not all individuals with MCI go on to develop AD, and better understanding of predictors of MCI-AD disease progression will be important.12 Clinical manifestations of AD correlate to a disease process as evidenced initially by pre-symptomatic regional cerebral hypometabolism and later when structural imaging and neuropathology demonstrate significant and widespread atrophy. The pre-symptomatic hypometabolism is considered to be an indication of synaptic abnormalities and attributed to toxic effects of abnormal proteins or oligomers. In the absence of established atrophy, the hope is that neuronal physiology may be restored if the offending ‘toxic material’ can be removed or rendered inactive.
We propose that prospective studies of AD in DS are more feasible due to the higher incidence of Alzheimer pathology and AD in this population and the likely homogeneity of causation, arguably linked to APP on chromosome 21. Such an approach provides the opportunity to prospectively study the biomarkers of disease, including neuroimaging or CSF biomarkers, alongside clinical measures. This would then enable proof-of-principle studies of whether earlier administration of disease-modifying treatments, including those already developed, such as anti-amyloid monoclonal antibodies, are efficacious.
ii. The need to improve predictive validity in models of AD
Research using DS-derived clinical, radiological or biological substrates may have advantages over existing animal and cellular disease models. Animal models critically require, for the most part, overexpression or alteration of a hypothesised ‘culprit gene’ and behavioural measures of the effect. This is a problematic approach as it requires a priori identification of a gene of interest and limits this approach to genetic abnormalities that are either monogenic or have high penetrance. A second problem with this approach is the quality of the outcome measures: developing specific and sensitive tests that capture ‘Alzheimer’ qualities in non-human subjects is a significant challenge. Nevertheless, these animal models have been heavily used in the development and testing of potential disease-modifying therapies.
An area of great interest at the moment is that of inducible pluripotent stem cells, and the potential for patient-derived cells to be ‘reprogrammed’ into neurons. In the context of DS, for example, skin cells taken by a simple skin biopsy have been used to generate neurons with the same genetic propensity for Alzheimer type pathology.13 This is a potentially powerful tool for the identification of pathways of cell dysfunction preceding cell death and molecules that may interfere with these pathways.
Critics would appropriately question the assumption that AD in DS resembles sporadic disease, and indeed, the differences discussed above demonstrate that there are limitations to this approach. Similar criticisms are applicable to the in-depth study of rare monogenic causes of AD. AD is a heterogeneous disease entity, as reflected by the multitude of genetic and non-genetic factors implicated in its pathogenesis, variation in clinical manifestations of pathological burden, and differing rates of disease progression. Therefore, a well-defined and more homogenously affected population, such as DS individuals with AD, may offer a useful initial study cohort, even though subsequent validation of treatment approaches in a broader population is necessary.
Discussion
Novel methods for investigating AD and developing therapeutic strategies are clearly necessary. It is exciting to see the enthusiasm of funding agencies for studies in DS as a way to better understand AD in DS and non-DS populations alike. It is equally good to see the many opportunities for detailed clinical studies, and robust trials that have been performed almost exclusively on AD in the general population to date, now being also made available to the DS population.
References
- Wisniewski KE, Dalton AJ, Mclachlan, DRC et al. Alzheimer’s disease in Down’s syndrome: Clinicopathologic studies. Neurology 1985:35:957-61. PMID: 3159974
- Oliver C and Holland AJ. Down’s Syndrome and Alzheimer’s disease: a review. Psychological Medicine 1986:16:307-22. PMID: 2941815
- Holland, AJ, Hon, J, Huppert, FA, Stevens, F and Watson, P. A population-based study of the prevalence and presentation of dementia in adults with Down Syndrome. British Journal of Psychiatry, 1998;172:493-8.
- Tanzi RE, Gusella JF, Watkins PC et al. Amyloid beta Protein Gene: cDNA, mRNA Distribution, and Genetic Linkage near the Alzheimer Locus. Science 1987:235:880-4. PMID: 2949367
- Jones EL, Mok K, Hanney M et al. Evidence that PICALM affects age at onset of Alzheimer’s dementia in Down syndrome. Neurobiol. Aging 2013:34:2441.e1-5. PMID: 23601808
- Selkoe DJ. Amyloid β-Protein and the Genetics of Alzheimer’s Disease. J Biol Chem 1996:271:18295-8. PMID: 8756120
- Ball SL, Holland AJ, Treppner P et al. Executive dysfunction and its association with personality and behaviour changes in the development of Alzheimer’s disease in adults with Down syndrome and mild to moderate learning disabilities. Br J Clin Psychol 2008:47:1-29. PMID: 17681112
- Mullins D, Daly E, Simmons A et al. Dementia in Down’s syndrome: an MRI comparison with Alzheimer’s disease in the general population. J Neurodev Disord 2013:5:19. PMID: 23962297
- Jack CR, Petersen RC, Xu YC et al. Prediction of AD with MRI-Based Hippocampal Volume in Mild Cognitive Impairment. Neurology 1999:52:1397-403. PMID: 10227624
- Jack CR, Petersen RC, O’Brien PC et al. MR-based hippocampal volumetry in the diagnosis of Alzheimer’s disease. Neurology 1992:42:183-8. PMID: 1734300
- Landt J, Carlos D’Abrera J, Holland AJ, Aigbirhio FI, Fryer TD, Canales R, Hong YT, Menon DK, Baron J-C and Zaman SH. Using positron emission tomography and [11C] Pittsburgh Compound-B to image brain fibrillar β-amyloid in adults with Down’s syndrome: its safety, acceptability, and feasibility. Archives of Neurology, 2011:68:890-6. PMID: 21403005
- Mitchell J, Arnold R, Dawson K et al. Outcome in subgroups of mild cognitive impairment (MCI) is highly predictable using a simple algorithm. J Neurol 2009:256:1500-9. PMID: 19434441
- Shi Y, Kirwan P, Smith J et al. A human stem cell model of early Alzheimer’s disease pathology in Down syndrome. Sci Transl Med 2012:4:124-9.


