Introduction
Coma accompanying fever, which now would be termed encephalitis, was described by Sydenham as early as the 17th century, although associations between fever and brain dysfunction were recognised even earlier.1 Since then, much progress has been made in understanding the causes, biological mechanisms, epidemiology and treatment of encephalitis; however, numerous gaps still exist in our knowledge: there is still a long way to go.
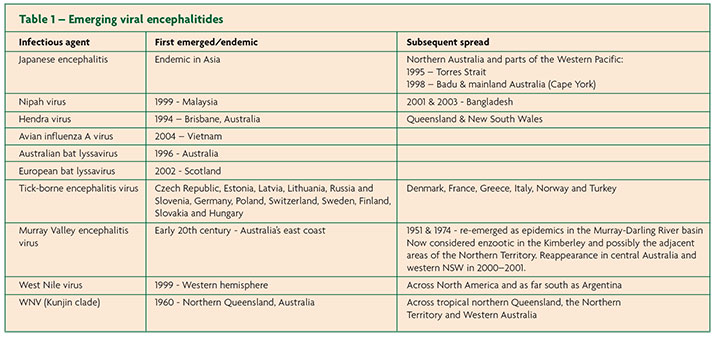
One reason for the increased interest in encephalitis is the recognition that it is a sentinel condition for new and emerging infections (Table 1). Consequently, numerous national studies have been implemented in different continents to investigate its aetiology and epidemiology.2-5 The recent discovery of antibody-associated forms of encephalitis has given added impetus to this effort. Other reviews have described what is already known about encephalitis.6,7 This paper will focus on the challenges faced in studying encephalitis and recent advances of direct clinical relevance that have occurred in the field.
Importance
Although considered a rare syndrome in resource-rich settings, the incidence of encephalitis is likely to be higher than previously estimated. It was estimated that only 700 cases of encephalitis occur per year in England;8 however, new data suggest that this is an underestimate and that the occurrence of encephalitis is substantially higher (Granerod et al., submitted). Outcomes remain poor: over one-third of encephalitis patients recruited to a multicentre prospective study of encephalitis in England either died or were left with severe disabilities.2 The median age of patients in this study was only 30 years; 34% of cases occurred in children <18 years of age. Other studies have shown similarly poor outcomes. In a contemporary French study 10% of patients died in the acute phase of the illness.3 After three years follow-up of 167 surviving patients, a further nine patients had died of encephalitis-related causes and 15% were severely impaired or in a vegetative state.9 It is estimated that ~70,000 cases of Japanese encephalitis (JE), considered the most important of the viral encephalitides in Asia, occur annually in the 24 JE-endemic countries.10 This is predominantly a disease of children; approximately 20–30% of cases are fatal and 30–50% of survivors have significant neurological sequelae.10 Survivors who make a seemingly good recovery are often left with milder impairments that impact upon quality of life. Encephalitis has significant implications not only for patients directly but also wider economic and public health implications.
Current problems
Encephalitis is challenging to diagnose, manage and study. It is a syndrome of multiple aetiologies and pathogeneses. Pathogenetic mechanisms for the parenchymal inflammation of encephalitis range from direct infectious to immune-mediated; however, specific mechanisms within each of these groups are diverse and often incompletely understood. For example, Mycoplasma pneumoniae is increasingly implicated in encephalitis; however, its exact role (i.e. whether through direct infection or as a trigger for immune-mediated disease) remains controversial due to incomplete understanding of the biology of the organism and host immune response to it, and inherent limitations of its specific microbiological diagnostic test in the context of central nervous system (CNS) disease.11-13
Despite greater than 100 known causes, in most cases of encephalitis neither a pathogenetic mechanism nor aetiology is identified. Accurate and complete case ascertainment of encephalitis cases is made difficult by the complexity of the syndrome, difficulties in distinguishing it from non-encephalitis mimics, and the lack of standard clinical case definitions. There is no standard laboratory diagnostic algorithm for encephalitis in the United Kingdom (UK); although most laboratories test for herpes simplex virus (HSV), varicella zoster virus (VZV) and enteroviruses nucleic acid sequences in the cerebrospinal fluid (CSF) of immunocompetent patients. This practice is supported in the recently published National Guidelines for the Management of Suspected Viral Encephalitis in the UK.14 Testing beyond this varies greatly between centres. To complicate matters further, the test specificity following detection of some viruses, such as lymphotropic herpes viruses (EBV; CMV; HHV-6), in CSF is much lower than for the neurotropic herpesviruses (HSV; VZV). For certain viruses, such as EBV, calculation of the CSF EBV viral load can be helpful: higher values are more likely indicative of aetiological significance.15 However, one pitfall for the diagnostician and researcher is HHV-6. A minority of patients have chromosomal integration of HHV-6 DNA; such patients have consistently high levels of HHV-6 DNA in CSF, blood and plasma.16,17 For other agents, such as West Nile Virus (WNV), detection of an acute serological response in CSF or serum provides strong evidence for causality. Although written primarily for epidemiological studies proposed diagnostic criteria for infectious aetiologies of encephalitis may aid the clinician in interpreting these laboratory results.18
Emerging infections
There is growing evidence that an increasing number of viruses can cause encephalitis in human hosts (Table 1). Many recently emerged zoonotic viruses, including Hendra virus and Australian bat lyssavirus, have presented with an encephalitic syndrome in humans.19 European bat lyssavirus resulted in the death of a man from rabies in Scotland in 2002.20 Two outbreaks that occurred in Bangladesh in 2001 and 2003 marked the re-emergence of Nipah virus encephalitis.21 A Vietnamese child, whose death in 2004 was reported to be from encephalitis of unknown cause, was later found to be infected with avian influenza H5N1, suggesting a wider clinical spectrum than previously recognised for this microbe.22 The 1999 outbreak in New York marked the detection of WNV in the Western hemisphere for the first time; it has since spread across America and as far south as Argentina.23 Although some aetiological agents are at present geographically restricted, global warming, ecological change, and an increase in international travel may help infectious agents to cross boundaries. The experience of WNV in North America illustrates the potential for diseases to be introduced to new areas if the vectors are present and the environment supportive.24 Hypothetically, new infectious causes could be found amongst the many encephalitis cases of unknown aetiology. Clinicians are encouraged to notify cases of acute encephalitis, as the prime purpose of the statutory notification system is to allow for rapid detection of potential outbreaks and epidemics.
Aetiological developments
Determining aetiology is a key first step to improve patient outcome. Several recent advances in the field of encephalitis are pertinent to the large proportion of cases of unknown cause.
A recent study by the Health Protection Agency (HPA) showed that systematic and extensive testing in a prospective cohort significantly reduced the proportion of cases of unknown aetiology from 60% previously described to 37%.2,8 It highlighted the importance of rigorous investigation for known causes of encephalitis – achieved in this study by involvement of a wide multidisciplinary team with expertise ranging from the clinical to laboratory.
The HPA study represents the largest prospective cohort of encephalitis patients to date in the British Isles. HSV was confirmed as the most common known aetiological agent, consistent with the findings of other international studies.3 It reinforces maintaining a low threshold for initiating acyclovir treatment in patients with suspected encephalitis. Interestingly of 38 HSV cases, three were diagnosed through detection of intrathecal production of HSV-specific antibody; these samples were PCR negative and would have been missed using only the latter diagnostic technique.25 Sampling CSF early (<3 days after the onset of neurological symptoms) or late (>14 days) in the disease course reduces the probability of a positive viral PCR.26 Thus, if CSF HSV PCR is not performed acutely, a later CSF and serum, taken 10-14 days after symptom onset, should be tested for intrathecal production of HSV antibodies to confirm the diagnosis.14
Arguably the most important recent aetiological development in the field of encephalitis is the recognition of antibody-associated forms of encephalitis, in particular N-methyl-D-aspartate receptor (NMDAR)-antibodies and voltage-gated potassium channel (VGKC)-complex antibodies. In the HPA study almost 10% of all encephalitis cases were associated with these antibodies. This was the first study to highlight their significance within a cohort of encephalitis patients, suggesting that they are more common than initially thought and emphasising the importance of considering this diagnosis, especially in patients with prominent seizures, normal cranial imaging, absence of fever, and only mild CSF pleocytosis. These syndromes are amenable to treatment if it is initiated promptly. Almost 60% of patients with antibody-associated encephalitis in the HPA study either died or were left severely disabled; their antibody status was only recognised retrospectively at the end of the study.2
The California Encephalitis Project (CEP), initiated in 1998 to study the epidemiology and aetiology of encephalitis in California, has reported similar findings.4 Since 2007, when NMDAR-antibodies were first reported, cases of encephalitis of uncertain aetiology in individuals ≤30 years of age referred to CEP have been tested for these antibodies. The frequency of NMDAR-antibody encephalitis was found to surpass that of individual viral aetiologies, including HSV.27
Antibody-associated encephalitis
There has been enormous interest over the last few years from researchers worldwide with regard to encephalitis associated with antibodies that target synaptic proteins. As mentioned above, the most common type is NMDAR-antibody encephalitis, followed by encephalitis associated with leucine-rich glioma inactivated 1 (LGI1) antibodies.28 Encephalitis has also been associated with antibodies to another VGKC-complex protein, namely contactin-associated protein-like 2 (CASPR-2). Still further antibodies have been described in limbic encephalitis, including those to alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) and gamma-aminobutyric acid-B (GABAB) receptors. More recently, antibodies to metabotropic glutamate receptor 5 (mGluR5) have been described in limbic encephalitis, as have antibodies to white matter glial or myelin antigens in acute disseminated encephalomyelitis.29 The field of antibody-mediated CNS disease is only in gestation; more antibody-associated syndromes may yet be identified amongst the many encephalitis cases of unknown cause. Rapidity of testing for antibody-associated encephalitis will be considerably assisted with the development of commercial assays. It is hoped that these will soon be available.29
Other developments
The recent HPA study led to the development of published clinical and aetiological case definitions, which informed how cases were classified.18 These present the UK perspective on aetiological case definitions for acute encephalitis; they include immune-mediated causes. Wide usage of these definitions is encouraged to facilitate better comparison between studies. They are the basis for an International Working Group that aims to determine by consensus an optimal set of criteria/case definitions to recommend for use in clinical practice, public health, and research internationally.
Within the UK a major practice development is the recent publication of National Guidelines for the Management of Suspected Viral Encephalitis in Adults and Children, briefly referred to above.14,30 The guidance covers initial investigation of all patients with suspected acute encephalitis; it includes specific management advice for the viral encephalitides, particularly HSV, VZV and enteroviral encephalitis; as well as advice for assessment of encephalitis in the immunosuppressed and returning traveller. A management algorithm is included modelled on the successful guidance for management of suspected bacterial meningitis. It can be downloaded from: http://www.braininfectionsuk.org/resources/documents/YJINF2823.pdf.
Whilst high dose intravenous acyclovir is well established as treatment for HSV encephalitis the role of other treatments, such as steroids, are not.31,32 There is circumstantial and animal model evidence to suggest that corticosteroids with acyclovir might improve clinical outcome in HSV encephalitis.33 The German trial of Acyclovir and Corticosteroids in Herpes-simplex-virus-Encephalitis (GACHE) is a multicentre, multinational, randomised, double-blind, placebo-controlled trial that aims to assess the efficacy of acyclovir and corticosteroids in the treatment of HSV encephalitis; it is recruiting at present.34
Challenges ahead
Despite numerous advances in the field of encephalitis, many challenges remain. Cases of unknown aetiology still form the largest subgroup. Virus discovery methods, which sought to amplify nucleic acid sequences of novel pathogens, did not prove fruitful in the HPA study. However, almost a quarter of unknown cases were shown to have intrathecal synthesis of IgG, for which antigenic specificity was not found following screening against of battery of microbial antigens.25 The presence of intrathecal IgG gives weight to an inflammatory or infective pathogenesis in these cases – they are less likely to be non-inflammatory syndromic mimics. Studying the antigenic specificity of intrathecal IgG could provide clues to the cause in these cases.35 Future studies could use peptide libraries to seek putative antigenic targets for CSF antibodies: such a technique might reveal novel infectious or autoimmune aetiologies.
For sporadic and epidemic causes of infectious encephalitis it is not understood why only a minority of individuals exposed to an infection develop encephalitis – the majority of encephalitic patients are not immunosuppressed. Host and pathogen-related factors are likely to be important. It has been shown in horses that a naturally occurring variation in a single amino acid position of the viral DNA polymerase enzyme results in differing pathogenic potential of a herpesvirus.36,37 Whether distinct strains of human HSV differ in their pathogenic capacity has yet clearly to be established in cases of HSV encephalitis. Host factors are increasingly implicated in encephalitis. Alleles in the innate immune effectors TLR3 and UNC93B have been identified that mediate susceptibility to herpes encephalitis in children.38,39 Further studies to address both pathogen neurovirulence and host susceptibility could increase our understanding of the pathogeneses of encephalitis, perhaps even providing potential targets for novel treatment strategies.
The HPA study showed that rigorous and systematic laboratory testing in a prospective study reduced the proportion of cases of unknown aetiology. Now a standard diagnostic algorithm for laboratory investigation is needed incorporating testing for infectious and antibody-associated causes. Such a development should be combined with improved access to specialist diagnostic tests performed in centres participating in rigorous quality control programmes.
Research and development programmes are currently underway in the UK addressing some of these issues. A major new NIHR programme grant on “Understanding and improving the outcome of encephalitis” is being co-ordinated by the Brain Infections Group in Liverpool. Further research co-ordinated by the HPA is underway to better define associations between neuroimaging results and specific encephalitis aetiologies, and to assess specific post-encephalitic morbidities in the UK. Furthermore, multicentre prospective studies in other parts of the world, including Australia, are underway to study aetiology seeking emerging infections.
Conclusions
Encephalitis has only recently become a priority for researchers, funders and policy makers. Recent research, particularly the emerging field of antibody-mediated CNS disease, has decreased the proportion of cases of unknown aetiology. But the proportion of encephalitic patients for whom no aetiology is found remains unacceptably high. Both novel infectious aetiologies and new antigenic targets for immune-mediated encephalitis could underlie these cases. Recent advances are encouraging but there is still a way to go.
References
- Sydenham T. Of the continued fever of the years 1673, 1674, 1675. Wallis G, ed. The work of Thomas Sydenham MD on acute and chronic disease with annotations by George Wallis. London: Robinson, Otridge, Hayes & Newbery; 1788. 299.
- Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D et al. Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis 2010;10(12):835-44.
- Mailles A, Stahl JP. Infectious encephalitis in France in 2007: a national prospective study. Clin Infect Dis 2009;49(12):1838-47.
- Glaser CA, Honarmand S, Anderson LJ, Schnurr DP, Forghani B, Cossen CK et al. Beyond viruses: clinical profiles and etiologies associated with encephalitis. Clin Infect Dis 2006;43(12):1565-77.
- Huppatz C, Durrheim DN, Levi C, Dalton C, Williams D, Clements MS et al. Etiology of encephalitis in Australia, 1990-2007. Emerg Infect Dis 2009;15(9):1359-65.
- Granerod J, Crowcroft NS. The epidemiology of acute encephalitis. Neuropsychol Rehabil 2007;17(4-5):406-28.
- Granerod J, Tam CC, Crowcroft NS, Davies NWS, Borchert M, Thomas SL. Challenge of the unknown: a systematic review of acute encephalitis in non-outbreak situations. Neurology 2010;75:924-32.
- Davison KL, Crowcroft NS, Ramsay ME, Brown DW, Andrews NJ. Viral encephalitis in England, 1989-1998: what did we miss? Emerg Infect Dis 2003;9(2):234-40.
- Mailles A, De Broucker T, Costanzo P, Martinez-Almoyna L, Vaillant V, Stahl JP. Long-term outcome of patients presenting with acute infectious encephalitis of various causes in France. Clin Infect Dis 2012;54(10):1455-64.
- Campbell GL, Hills SL, Fischer M, Jacobson JA, Hoke CH, Hombach JM et al. Estimated global incidence of Japanese encephalitis: a systematic review. Bull World Health Organ 2011;89(10):766-74.
- Lewis P, Glaser CA. Encephalitis. Pediatr Rev 2005;26(10):353-63.
- Kolski H, Ford-Jones EL, Richardson S, Petric M, Nelson S, Jamieson F et al. Etiology of acute childhood encephalitis at The Hospital for Sick Children, Toronto, 1994-1995. Clin Infect Dis 1998;26(2):398-409.
- Bitnun A, Richardson SE. Mycoplasma pneumoniae: Innocent Bystander or a True Cause of Central Nervous System Disease? Curr Infect Dis Rep 2010;12(4):282-90.
- Solomon T, Michael BD, Smith PE, Sanderson F, Davies NW, Hart IJ et al. Management of suspected viral encephalitis in adults–Association of British Neurologists and British Infection Association National Guidelines. J Infect 2012;64(4):347-73.
- Majid A, Galetta SL, Sweeney CJ, Robinson C, Mahalingham R, Smith J et al. Epstein-Barr virus myeloradiculitis and encephalomyeloradiculitis. Brain 2002;125(1):159-65.
- Ward KN, Leong HN, Nacheva EP, Howard J, Atkinson CE, Davies NW et al. Human herpesvirus 6 chromosomal integration in immunocompetent patients results in high levels of viral DNA in blood, sera, and hair follicles. J Clin Microbiol 2006;44:1571-4.
- Isaacson E, Glaser CA, Forghani B, Amad Z, Wallace M, Armstrong RW et al. Evidence of human herpesvirus 6 infection in 4 immunocompetent patients with encephalitis. Clin Infect Dis 2005;40(6):890-3.
- Granerod J, Cunningham R, Zuckerman M, Mutton K, Davies NW, Walsh AL et al. Causality in acute encephalitis: defining aetiologies. Epidemiol Infect 2010;138(6):783-800.
- Paterson BJ, Mackenzie JS, Durrheim DN, Smith D. A review of the epidemiology and surveillance of viral zoonotic encephalitis and the impact on human health in Australia. NSW Public Health Bull 2011;22(5-6):99-104.
- Warrell MJ, Warrell DA. Rabies and other lyssavirus diseases. Lancet 2004;363(9413):959-69.
- Hsu VP, Hossain MJ, Parashar UD, Ali MM, Ksiazek TG, Kuzmin I et al. Nipah virus encephalitis reemergence, Bangladesh. Emerg Infect Dis 2004;10(12):2082-7.
- de Jong MD, Bach VC, Phan TQ, Vo MH, Tran TT, Nguyen BH et al. Fatal avian influenza A (H5N1) in a child presenting with diarrhea followed by coma. N Engl J Med 2005;352(7):686-91.
- Petersen LR, Hayes EB. West Nile virus in the Americas. Med Clin North Am 2008;92:1307-22.
- Campbell GL, Marfin AA, Lanciotti RS, Gubler DJ. West Nile virus. Lancet Infect Dis 2002;2(9):519-29.
- Ambrose HE, Granerod J, Clewley JP, Davies NW, Keir G, Cunningham R et al. Diagnostic strategy used to establish etiologies of encephalitis in a prospective cohort of patients in England. J Clin Microbiol 2011;49(10):3576-83.
- Davies NWS, Brown LJ, Gonde J, Irish D, Robinson RO, Swan AV et al. Factors influencing PCR detection of viruses in cerebrospinal fluid of patients with suspected CNS infections. J Neurol Neurosurg Psychiatry 2005;76:82-7.
- Gable MS, Sheriff H, Dalmau J, Tilley DH, Glaser CA. The frequency of autoimmune N-methyl-D-aspartate receptor encephalitis surpasses that of individual viral etiologies in young individuals enrolled in the California Encephalitis Project. Clin Infect Dis 2012;54(7):899-904.
- Graus F, Dalmau J. CNS autoimmunity: new findings and pending issues. Lancet Neurol 2012;11(1):17-19.
- Zuliani L, Graus F, Giometto B, Bien C, Vincent A. Central nervous system neuronal surface antibody associated syndromes: review and guidelines for recognition. J Neurol Neurosurg Psychiatry 2012;83:638-45.
- Kneen R, Michael BD, Menson E, Mehta B, Easton A, Hemingway C et al. Management of suspected viral encephalitis in children – Association of British Neurologists and British Paediatric Allergy, Immunology and Infection Group national guidelines. J Infect 2012;64(5):449-77.
- Skoldenberg B, Forsgren M, Alestig K, Bergstrom T, Burman L, Dahlqvist E et al. Acyclovir versus vidarabine in herpes simplex encephalitis. Randomised multicentre study in consecutive Swedish patients. Lancet 1984;2(8405):707-11.
- Whitley RJ, Alford CA, Hirsch MS, Schooley RT, Luby JP, Aoki FY et al. Vidarabine versus acyclovir therapy in herpes simplex encephalitis. N Engl J Med 1986;314(3):144-9.
- Meyding-Lamade UK, Oberlinner C, Rau PR, Seyfer S, Heiland S, Sellner J et al. Experimental herpes simplex virus encephalitis: a combination therapy of acyclovir and glucocorticoids reduces long-term magnetic resonance imaging abnormalities. J Neurovirol 2003;9(1):118-25.
- Martinez-Torres F, Menon S, Pritsch M, Victor N, Jenetzky E, Jensen K et al. Protocol for German trial of Acyclovir and corticosteroids in Herpes-simplex-virus-encephalitis (GACHE): a multicenter, multinational, randomized, double-blind, placebo-controlled German, Austrian and Dutch trial [ISRCTN45122933]. BMC Neurol 2008;8:40.
- Burgoon MP, Owens GP, Carlson S, Maybach AL, Gilden DH. Antigen discovery in chronic human inflammatory central nervous system disease: panning phage-displayed antigen libraries identifies the targets of central nervous system-derived IgG in subacute sclerosing panencephalitis. J Immunol 2001;167(10):6009-14.
- Goodman LB, Loregian A, Perkins GA, Nugent J, Buckles EL, Mercorelli B et al. A point mutation in a herpesvirus polymerase determines neuropathogenicity. PLoS Pathog 2007;3(11):e160.
- Nugent J, Birch-Machin I, Smith KC, Mumford JA, Swann Z, Newton JR et al. Analysis of equid herpesvirus 1 strain variation reveals a point mutation of the DNA polymerase strongly associated with neuropathogenic versus nonneuropathogenic disease outbreaks. J Virol 2006;80(8):4047-60.
- Lauring AS, Cheng HH, Eiden MV, Overbaugh J. Genetic and biochemical analyses of Pit1determinants for FeLV-T suggest a novel mechanism for entry. J Virol 2002;76:8069-78.
- Webster DR, Hekele AG, Lauring AS, Fischer KF, Li H, Andino R et al. An enhanced single base extension technique for the analysis of complex viral populations. PLoS One 2009;4:e7453.

