Abstract
This article describes the pain neuro-matrix and shows how hypnotic suggestions can be used directed at each part of this in order to be maximally effective. Although inducing the hypnotic state may be relatively simple, it is important to know how to utilise it effectively using suggestion and imagery. An understanding of the patient’s clinical condition and some counselling or psychological training are essential.
Over the last sixty years huge progress has been made into our understanding of the biological, psychological and social determinants of acute and chronic pain. However, many questions about the nature of the experience of pain and suffering are so fundamental to the nature of our lived experience, that they are no more amenable to our current modes of enquiry, be they scientific, philosophical or spiritual, than the nature of consciousness itself. This creates difficulties and uncertainty for both patients and health professionals, with advances in effective treatments being frustratingly slow. It is in this context that psychosocial approaches have taken on an increasingly important role with hypnotherapy being part of this movement.
Western biological theories on how pain is generated have existed for a very long time with theories of specific peripheral pathways being traced through the ideas of Descartes to the ideas of Von Frey with different peripheral receptors encoding different sensations. From Plato through to Erb and Livingstone, theories of intensity and ultimately central summation emerged. In the 1920s and 1930s Nafe proposed that patterns of neural activity encoded painful sensations. This was developed and in the late 1950s Noordenbos introduced the concept of fast conducting pathways of fibres modulating the effects of slow conducting pain generating pathways.1 This laid the ground for Melzack and Wall’s gate control theory of 1965 following behavioural research by Melzack and physiological experiments on the spinal cord by Wall, that led on to their collaboration.2 Their work had shown that the outer layers of the spinal cord dorsal horn was a site where fast conducting peripheral nerve fibres could inhibit the transmission of slow conducting unmyelinated fibres. Subsequent experimental work led to the introduction of the concept of descending inhibitory control whereby supraspinal pathways descending from the brain could modulate nociceptive peripheral input.3
Ideas that led to the theories and evidence of the role of central neuroplasticity in chronic sensitisation to pain began in the 1880s, with much development from the 1970s onwards.4 Then starting in the early 1990s modalities for functional brain imaging began to be developed. SPECT and then PET studies appeared as well as MEG studies. Soon however, paradigm-based fMRI studies began to dominate the field.5 More latterly resting state fMRI studies have become possible as well as anatomical mapping of white fibre brain tracts with MRI diffusion tensor imaging.6 The well-known patterns of anterior cingulate activation, primary and secondary somatosensory cortex activation, as well as activation of thalami nuclei, were reported in some of the earliest functional imaging studies. At that stage, as now, albeit to a much lesser extent, the nature of the fMRI signal and its temporal and spatial resolution, set limits on what these studies could achieve. For example, imaging of small brain stem and spinal cord structures is very difficult, although advances in ultra-high field MRI may begin to change that.
Over the last fifty years our understanding of the pharmacology of pain and its modulation has also increased out of all recognition. Starting with the revelation of Hughes and Kosterlitz’s identification of enkephalins in 1975, the role of other neuromodulatory endogenous systems has been identified including cannabinergic systems, the role of serotonin and noradrenaline in descending inhibitory pathways and many other systems. This has led to the development of new analgesics such as the gabapentinoids and the repurposing of old ones such as tricyclic antidepressants.7,8 It also paved the way for research into the pharmacological mechanisms of the placebo response with the involvement of both opioid and Cholecystokinin (CCK) pathways being identified.9
In 1968 Melzack and Casey introduced a new conceptual pain model with three axes – cognitive, sensory–discriminative and motivational-affective.10 This multidimensional approach was based in part on Melzack and Torgerson’s research into the language of pain which in turn led to the development of the McGill pain questionnaire.11,12
In 1999 Melzack proposed a more generalised theory of pain that he called the neuromatrix and neurosignature whereby the body, peripheral and central nervous system with all its internal and external stimuli, and social, genetic and other influences produce our sense of embodiment (neuromatrix), with disturbances both external and internal, producing the neurosignature of pain.13
While biological models of pain have become more sophisticated, they still cannot explain all the many experiences of pain that people report. This has been compounded by the failure of many biological approaches to the relief of pain with perhaps the current opioid crisis perhaps being the most egregious example.
This deficit in our understanding and response to those in pain was highlighted in Engel’s introduction of the biopsychosocial model in a seminal paper in 1977.14 This was about the time that Fordyce at the University of Seattle was introducing psychological models of managing pain using Beck’s, then still new, model of cognitive behavioural therapy. Since that time pain management programmes based on Fordyce’s model have become ubiquitous in the West.15 They are based on good empirical evidence. Other forms of psychological intervention have also been used to manage chronic pain. There is a growing body of work on mindfulness, and now also a large body of work on hypnosis, the subject of this paper.
Hypnosis in the context of pain management is closely allied to placebo mechanisms although there are important differences. Both depend on manipulation of expectancy with suggestion on some level being required.16 Over the last decade research on placebo has accelerated taking our understanding far beyond its pharmacological substrates and seeing it as a semiotic epiphenomenon of a social-neural system evolved for the defence of the organism.17,18
Hypnosis has been defined as “A social interaction in which one person, designated the subject, responds to suggestions offered by another person, designated the hypnotist, for experiences involving alterations in perception, memory and voluntary action”19 or “A state of consciousness involving focused attention and reduced peripheral awareness characterized by an enhanced capacity for response to suggestion.”20
In the clinical context hypnosis is always a collaborative process between the caregiver and client. It is also always undertaken in the context of overall management – it is never a treatment in itself and good rapport and the client’s understanding of the means and aims of the process are essential for its success. This is why psychoeducation is so important, especially in chronic pain. Most patients’ ideas about pain are still informed by our predominately biomedical culture where there must always be a physical cause for symptoms and if investigations are negative, then it is assumed symptoms are imaginary, or worse, invented. Doctors are often not immune from this process and will keep on searching for a ‘cause’ for the pain, doing more and more investigations and treatments (manipulations / steroid injections), although sometimes this is because they feel helpless if they cannot ‘cure’ their patient’s pain, rather than ignorance of the mechanisms involved.
Nociception can produce structural and physiological changes in the brain that alter future pain processing21 such that pain as a result of nociception becomes more easily triggered over time. But nociception is not pain and the activation of nociceptors and neurones in the spinothalamic tract is neither necessary nor sufficient to produce the perception of pain. Pain is perceived when complex, integrated cortical (supraspinal) systems are engaged and this can occur with or without nociception.
Hypnosis has been used to treat every type of pain condition over centuries and across cultures22 and can be an extremely effective treatment for both acute and chronic pain. It is one of the most well researched areas in clinical hypnosis.23,24,25
Inducing hypnosis itself, without any other suggestions for comfort, results in a shift in brain activity globally, increasing relative alpha rhythms and decreasing beta.26 This matches the pattern that can be seen in the brain waves of someone experiencing pain relief.
Suggestions given in hypnosis to help ease pain can work at all levels involved in the pain matrix.27 There is no one single mechanism underlying hypnotic analgesia, rather hypnotic suggestions can be tailored to work at specific levels in the matrix, if one area is particularly troublesome. Suggestions given to reduce intensity of pain show activation in the primary sensory cortex28 whilst suggestions to reduce the unpleasantness activated the anterior cingulate cortex.29 Suggestions to increase feelings of wellbeing (activating the insula), letting go pain and allowing in feelings of comfort (activating STT) can be useful. Suggestions to reduce fear and possible negative connotations of the pain work at the level of the pre-frontal cortex.
Numerous controlled studies demonstrate physiological responses associated with hypnosis, which are not demonstrated with role playing and imagination alone. Neuroscience has shown that using imagery in the ‘hypnotic state’ triggers similar fMRI changes to those that occur when the suggested experience is performed in reality. 30,31
Although there is a spread of hypnotic ability within the general population, clinically it is found that most people can benefit in some way. Tailoring the hypnotic induction and the way suggestions are given can maximise the potential effect for the individual patient. Suggestion can be given verbally or more often by using imagery, which may be visual, auditory, kinaesthetic or simply an awareness. This is important for patients who are not very visual, as working with ‘just knowing it’s there’ can also be effective. Another important point is the difference between associated imagery, where one is ‘in’ the image (which increases emotional impact and is used for giving positive suggestion) and dissociated or third person imagery where one observes from a distance, which reduces emotional impact and is useful when working with negative scenarios.
Imagery to help let go of negative feelings and to access strengths is always useful, as is imagery of a special, calm place where the patient can go in their imagination to connect with feelings of calmness and peace, or retreat to, when undergoing some unpleasant procedure. The patient decides on their own imagery and explores it using all their senses, to really ‘be there’.
Imagery can be used to alter how patients see others or a procedure, from threatening and fear provoking, to something that they can cope with calmly. Positive mental rehearsal of an exercise or procedure is often helpful – getting the patient to imagine (associate) with their desired outcome. While in hypnosis ‘stepping into’ how they wish to feel not only gives positive suggestion but acts as a goal, helping to move them towards this state.
Using imagery to change patient’s internal representation of themselves and their pain can help give them back control and have a marked effect on the intensity and ‘bothersomeness’ of their pain. Classic imagery (dials, scales, numbers, healing fluid) can be used in a guided visualisation to ‘turn down’ discomfort and ‘turn up’ comfort and calmness.
The patient can go down “into the control centre of their mind” and find the control for pain/comfort and by altering it give themselves suggestions of increasing comfort and ease.
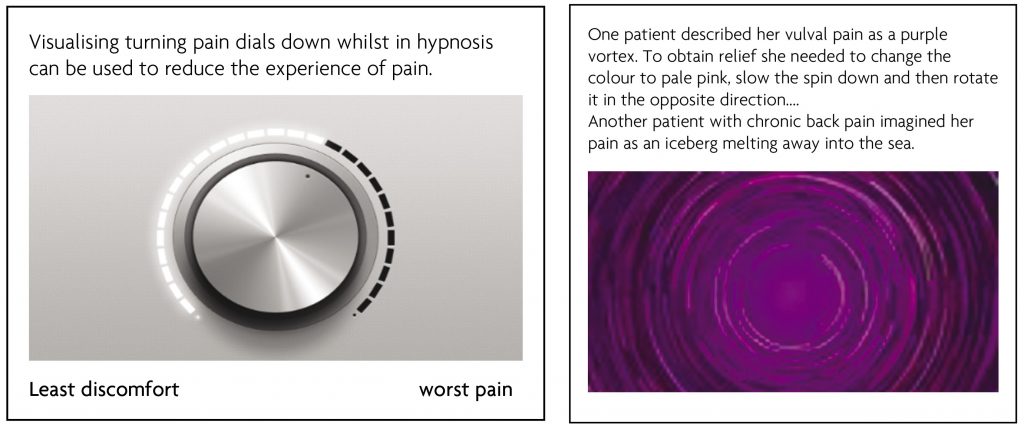
Another approach is to ask the patient in hypnosis to shrink themselves down and go and visit the painful area and describe what they see. Alternatively, they can imagine painting a picture or making a model of their pain. Details of the image are elicited such as its texture, colour, motion, size, sound and then they are asked what change can they make that would be helpful; that might help it feel easier?
Sometimes in hypnosis it is relatively easy to ‘talk to that part of your mind that knows all about your pain’ and establish that the pain no longer serves a necessary function. If this is the case, then agreement can be obtained that the pain can ease unless it is needed.
Although much can be done with simple suggestion and use of imagery in the hypnotic state many patients have underlying issues that need resolution. It is beyond the scope of this article to elaborate on these but in my experience many patients with chronic pain, especially those with conditions such as fibromyalgia, will not get a lot better unless these are addressed.
Many studies have shown that, as well as reducing the intensity and ‘bothersomeness’ of chronic pain, with both immediate and long-term effects, the benefits of hypnosis go far beyond simple pain relief32. So, time spent giving appropriate suggestions, teaching a patient self-hypnosis and the use of imagery is time well spent and gives the patient a lifelong tool with which to help themselves.
Hypnosis Training
There is no statutory regulation of hypnosis in the UK and many organisations offer hypnosis training of varying standards. There is only one not for profit organisation in England that is run solely for and by healthcare professionals. BSCAH (The British Society of Clinical & Academic Hypnosis) runs training courses for qualified healthcare professionals and also a university Advanced Diploma with the City of Birmingham University. Details of trainings can be found at https://www.bscah.com/about-training
References
1. Moayedi M & Davis K. Theories of Pain: from specificity to gate control. Journal of neurophysiology. 2013;109:5-12. https://doi.org/10.1152/jn.00457.2012
2. Melzack R & Wall P. Pain mechanisms: A new theory. Science. 1965;150:971-9. https://doi.org/10.1126/science.150.3699.971
3. Le Bars D, Dickenson AH & Besson JM. Diffuse noxious inhibitory controls (DNIC). II. Lack of effect on non-convergent neurones, supraspinal involvement and theoretical implications. Pain. 1979;6(3):305-27. https://doi.org/10.1016/0304-3959(79)90050-2
4. Coderre TJ & Melzack R. The contribution of excitatory amino acids to central sensitization and persistent nociception after formalin-induced tissue injury. Neuroscience. 1992; 12 (9): 3665-70. https://doi.org/10.1523/JNEUROSCI.12-09-03665.1992
5. Morton D, Sandhu J, Jones A. Brain imaging of pain: state of the art. Journal of Pain Research. 2016; 9: 613-624. https://doi.org/10.2147/JPR.S60433
6. Gronemann D, Koch K & Bantel CP. Diffusion tensor imaging of white matter microstructure in chronic pain: a tract-based spatial statistics study and a systematic review. 2020 Preprint https://doi.org/10.1101/2020.04.16.20068197
7. Hughes J, Smith TW, Kosterlitz HW, Fothergill LA, Morgan BA & Morris HR. Identification of two related pentapeptides from the brain with potent opiate agonist activity. Nature. 1975;258:577-579. https://doi.org/10.1038/258577a0
8. Agarwal N, Pacher P, Tegeder I, Amaya F, Constantin CE, Brenner GJ, Tiziana R, Michalski CW, Marsicano G, Monory, Mackie K, Marian C, Batkai S, Parolaro D, Fischer MJ, Reeh P, Kunos G, Kress M, Lutz B, Woolf CJ & Kuner R. Cannabinoids mediate analgesia largely via peripheral type 1 cannabinoid receptors in nociceptors. Nature Neuroscience. 2007;10(7):870-9. https://doi.org/10.1038/nn1916
9. Benedetti F. (2021) Placebo effects. 3rd edition. Oxford University Press.
10. Melzack R & Casey K. (1968) Sensory, Motivational and central Control Determinants of Pain – A new conceptual model Proceedings of the First International Symposium on the Skin Senses, Tallahasee Florida. Kenshalo D ed p 423-439 Charles Thomas, Springfield Illinois USA.
11. Melzack R and Torgerson W. On the language of pain Anesthesiology. 1970;34(1):50-59. https://doi.org/10.1097/00000542-197101000-00017
12. Melzack R. The McGill Pain questionnaire: major properties and scoring methods. Pain 1975;(1):277-299. https://doi.org/10.1016/0304-3959(75)90044-5
13. Melzack R. From the gate to the Neuromatrix. Pain Supplement. 1999;6:S121-S126. https://doi.org/10.1016/S0304-3959(99)00145-1
14. Engel G. The Need for a New medical Model: A Challenge for Biomedicine. Science 1977;196(4286):129-135. https://doi.org/10.1126/science.847460
15. Fordyce W (1976) Behavioural Methods for Chronic pain and Illness. Mosby Company Sant Louis MO.
16. Kirsch I. Clinical Hypnosis as a Nondeceptive Placebo: Empirically Derived Techniques. American Journal of Clinical Hypnosis.1994;37(2):95-106. https://doi.org/10.1080/00029157.1994.10403122
17. Millar F and Collaca L. Semiotics and the placebo effect Perspectives in Biology and Medicine.2010;53(4): 509-516. https://doi.org/10.1353/pbm.2010.0004
18. Benedetti F, & Amanzio M. The neurobiology of placebo analgesia: From endogenous opioids to cholecystokinin. Progress in Neurobiology. 1997;52(2):109-25. https://doi.org/10.1016/S0301-0082(97)00006-3
19. Kihlstrom JF. Hypnosis. Annual Review of Psychology. 1985;36:385-418. https://doi.org/10.1146/annurev.ps.36.020185.002125
20. Elkins G, Barabasz A, Council J & Spiegel D. Advancing Research and Practice: The Revised APA Division 30 Definition of Hypnosis. American Journal of Clinical Hypnosis. 2015;57(4):378-385. https://doi.org/10.1080/00029157.2015.1011465
21. Saab C. Pain-related changes in the brain: diagnostic and therapeutic potentials. Trends in Neurosciences. 2012;35(10): 629-637.
https://doi.org/10.1016/j.tins.2012.06.002
22. Pintar J & Lynn S (2008) Hypnosis: A Brief History. Wiley-Blackwell.
23. Hawkins R A. Systematic meta-review of hypnosis as an empirically supported treatment for pain. Pain Reviews. 2001;8:47-73. https://doi.org/10.1191/0968130201pr175ra
24. Elkins G, Jensen M & Patterson D. Hypnotherapy for the Management of Chronic Pain. International Journal of Clinical and Experimental Hypnosis. 2007;55(3):275-287. https://doi.org/10.1080/00207140701338621
25. Thompson T, Terhune D, Oram C, Sharangparni J, Rouf R, Solmi M, Veronese N & Stubbs B. The effectiveness of hypnosis for pain relief: A systematic review and meta-analysis of 85 controlled experimental trials. Neuroscience and Biobehavioral Reviews. 2019;99:298-310. https://doi.org/10.1016/j.neubiorev.2019.02.013
26. Jensen M, Adachi T, Tomé-Pires C, Lee J, Osman Z & Miró J. Mechanisms of hypnosis: toward the Development of a Biopsychosocial Model. International Journal of Clinical & Experimental Hypnosis. 2015;63(1):34-75. https://doi.org/10.1080/00207144.2014.961875
27. Derbyshire S, Whalley M & Oakley D. Fibromyalgia pain and its modulation by hypnotic and non-hypnotic suggestion: An fMRI analysis. European Journal of Pain. 2009;13:542-550. https://doi.org/10.1016/j.ejpain.2008.06.010
28. Hofbauer R, Rainville P, Duncan G & Bushnell M. Cortical representation of the sensory dimension of pain. Journal of Neurophysiology. 2001;86(1):402-411. https://doi.org/10.1152/jn.2001.86.1.402
29. Rainville P, Duncan G, Price D, Carrier B & Bushnell M. Pain affect encoded in human anterior cingulate but not somatosensory cortex. Science. 1997;277(5328):968-971. https://doi.org/10.1126/science.277.5328.968
30. Kosslyn S, Thompson W, Constantin-Ferrando M, Alpert N & Spiegel D. Hypnotic visual illusion alters colour processing in the brain. American Journal of Psychiatry. 2000;157:1279-84. https://doi.org/10.1176/appi.ajp.157.8.1279
31. Derbyshire S, Whalley M, Stenger V & Oakley D. Cerebral activation during hypnotically induced and imagined pain. NeuroImage. 2004;27:969-78. https://doi.org/10.1016/j.neuroimage.2004.04.033
32. Jensen M & Patterson D. Hypnotic Approaches for Chronic Pain Management: Clinical Implications of Recent Research Findings. American Psychologist. 2014;69 (2):167-177. https://doi.org/10.1037/a0035644
