Abstract
Older and frail patients are prone to falls, with a propensity to sustain injuries to the cervical spine. As the population ages, cervical spine fractures will become more prevalent. Similar to hip fractures; cervical fractures are associated with frailty. Research and service change has improved management of older and frail patients with hip fractures, improving outcomes, but similar progress has not been realised for cervical spine fractures. Here we outline current issues in management of cervical fractures and consider how improved prevention, diagnostics, management strategies and outcome measures could enhance patient care and outcomes.
Introduction
W
ith an ageing population, low impact trauma secondary to falls in older or frail adults is increasing in the United Kingdom (UK) [1]. The incidence of falls increased 70% from 2010 to 2017, with 220,160 hospital admissions for falls in patients over 65 years old and an estimated annual cost of £4.4 billion for fragility fractures related to falls [2]. Much has been done to improve the management of patients with hip fractures in this cohort [3]. Cervical spine injuries have received less attention, perhaps because of their lower incidence. One study of Medicare patients from the United States identified that in 2011 the rate of cervical fractures in patients over sixty-five years of age was 5.3/10,000 compared to hip fractures occurring in 63.5/10,000.[4] However, they identified that over their study period (2007-2011) the incidence of cervical spine fractures had increased whilst that of hip fractures had decreased (4.6/10,000 cervical spine fractures vs. 77.3/10,000 hip fractures in 2007) [4].
Crucially, a statistically significant greater mortality rate was noted in patients with a cervical fracture, with or without spinal cord injury (SCI) (41.7%, 24.7%, respectively), compared to those with hip fractures (22.7%) [4]. In the UK, Baxter et al identified a greater incidence of delirium and pressure sores, a longer duration of hospital stay, and an increased chance of discharge to a care facility rather than home, when comparing cervical to hip fractures in patients over sixty years old [4,5]. Unlike the cervical fracture cohort, the hip fracture cohort in this study had early structured input from Orthogeriatric specialists, which is now standard care in the NHS and has been demonstrated to reduce 30-day mortality [5]. In contrast, there has not been an impetus for standardisation of care and improvements in care for patients with cervical fractures.
In the elderly/frail patient, the upper cervical spine (C1-2) is the site of injury in almost 70% of cervical fractures. This is likely because of degenerative changes in the subaxial spine that cause ankylosis and transmit traumatic forces through the upper spine. In patients over the age of 80, half of these injuries are fractures of the odontoid process of the C2 vertebra [6]. The majority of these injuries are managed non-operatively in the UK.
Despite the rising incidence of cervical spine fractures in the elderly, only 14% of the cervical spine fracture research pertains to patients over the age of 65 [7]. Moreover, only 6% relates to conservative management strategies [7], with a heavy focus on surgical interventions. The aim of this article is to identify challenges to improving the care of these vulnerable patients and delineate how these challenges might be addressed.
Prevention and risk factors
The main cause of a cervical spine fracture in the older/frail population is a fall from standing height [8]. Prevention of falls should not be overlooked as an important consideration for improving outcomes. The PROFET study (prevention of falls in the elderly trial) randomised British patients over sixty-five years of age who had previously presented to the emergency department following a fall to either multimodal intervention (n=184) or usual therapy (n=213). Multimodal intervention included outpatient physician led medical assessment of falls risks with interventions directed at counteracting these, and a single home visit by an occupational therapist with resultant advice/education/home modifications. At one-year follow-up, the risk of recurrent falls was significantly reduced in the intervention arm (183 vs. 510 falls) with an odds ratio of falling again being 0·39 [95% CI 0·23–0·66] and requirement for re-hospitalisation being 0·61 [95% CI 0·35–1·05].
Whilst chronological age is often used as a surrogate, frailty is a better identifier of patients at risk of falls than age alone. Frailty scores could help target specialist input at an earlier stage for patients most likely to benefit from the targeted therapies shown to be effective [9,10]. Community delivered services may be cost effective in reducing falls and their sequelae, including fractures. The financial benefit of screening and intervention needs to be further evaluated.
Pre-existing degenerative disease and spinal stenosis has been identified as an important risk factor for development of fracture after falling. One study demonstrated that more than 90% of patients with odontoid (C2) fractures had evidence of atlanto-odontoid degeneration on imaging [11]. Special attention must be paid to certain conditions that cause ankylosis (fusion) across the spine and render the subject more susceptible to injury, including ankylosing spondylitis and diffuse idiopathic skeletal hyperostosis (DISH). Imaging-based assessments of ageing and disease processes of the spine may elucidate further risk factors for injuries. This may inform enhanced injury prevention and management strategies. In the future, artificial intelligence approaches may be able to automatically quantify patient risk for a cervical fracture after routine imaging, supporting risk stratification and tailored interventions for at-risk patients.
Presentation and diagnosis
In the acute setting, following a fall, patients may present with a range of symptoms including pain, radiculopathy or evidence of SCI. They may also be entirely asymptomatic, especially if they have an associated, painful distracting injury elsewhere. Imaging can assess for potential spinal instability. Even in a neurologically intact subject, deformity caused by the fracture upon physiological loading can compromise structural integrity of the spine and causes compression of the spinal nerves or cord. Clinicians must have a low index of suspicion for cervical fractures in older and frail patients after a fall.
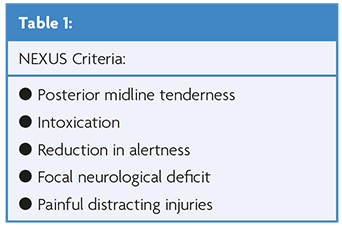
Diagnosis of a fracture requires cervical spine imaging. The Canadian C-spine rules mandate that all patients over sixty-five years of age be immobilised following trauma and imaged if there is concern of cervical spine injury [12]. By contrast, the national emergency X-Radiography utilisation study (NEXUS) stated that in the absence of five criteria, no imaging is required (see Table 1) [13]. However, the NEXUS criteria may not be applicable in the older and frail population because of difficulty in clinical examination.
One prospective cohort study assessing 596 patients over sixty-five years old reported a 100% sensitivity and specificity when using the NEXUS criteria [14]. A larger study analysing a single institute’s trauma registry of 4,035 patients aged over sixty-five demonstrated a sensitivity of 94.8% using the NEXUS criteria to exclude a fracture [15]. A systematic review identified a 66-100% sensitivity using the NEXUS criteria in patients aged over 65 [16], with bias in all included studies. This compares to the original NEXUS study, which found a sensitivity of 99.6% when the criteria was used for 34,069 patients of any age, although the patients were mostly young adults (mean, 37; interquartile range, 23 to 47). The lack of high quality evidence for sensitivity of NEXUS criteria in the elderly/frail suggests further research is required in determining the suitability of current decision-making tools and whether a novel one for this population is required.
Plain radiographs alone are inadequate, because osteoporosis and degenerative processes reduce sensitivity in detection of cervical fractures. National Institute for Health and Care Excellence (NICE) guidelines suggest patients over the age of sixty-five sustaining a head injury should have the cervical spine included in their computed tomography (CT) head examination where there is concern of a cervical injury [17]. For patients sustaining a fall without head injury, plain radiographs can be used initially but there should be a low threshold for CT if injury is suspected, especially if adequate three view radiographs cannot be obtained. Technically adequate radiographs in this population were obtained in only 79.5-89.4% cases in one study because of degenerative changes, body habitus and inability to open the mouth wide enough to obtain radiographs of the odontoid peg [18]. CT is the gold-standard diagnostic modality, providing rapid, high quality imaging of the bony spine. Up to 40% of elderly patients with cervical fractures may harbour other fractures of the spine, which may be non-contiguous, and examination/imaging to screen for these should be carried out [19].
Concomitant traumatic vertebral artery injury (TVAI) may affect patient outcomes and therefore management [19]. The incidence is approximately 6% in all patients with blunt injury to the cervical spine causing a fracture or ligamentous injury. However, the incidence of ischaemia secondary to TVAI is low, with only 3/34 elderly patients (>65years) suffering an ischaemic stroke in one large study [20]. High-risk features suggestive of TVAI include: fractures of the foramen transversarium, facet dislocations and vertebral body subluxation, with positive predictive values of 44%, 45%, 80%, respectively. Two or more of these fracture patterns in combination have a sensitivity of >92% for TVAI [21]. Imaging should be performed in these at risk patients with consideration of antiplatelet/anticoagulant therapy in the presence of TVAI.
Magnetic Resonance Imaging (MRI) provides excellent visualisation of neural structures and is useful if there are abnormal neurological findings on examination to assess for cord/root compression. MR can also assess for disc/ligamentous injury, which, in combination with the morphology of the bony injury (best seen on CT), are indicators of potential instability. MRI may also be useful to exclude a pathological fracture following diagnosis on CT, where red flags indicate an underlying pathological cause such as malignancy or infection. Drawbacks of MR include the requirement of a cooperative patient, that it takes time to complete, and that it is relatively expensive. One study assessing the role of MR in this population investigated whether an MRI altered medical management according to expert opinion. The study found that MR altered management in the presence of neurological signs or symptoms but in the absence of neurological deficit rarely identified evidence of instability occult on CT [22]. In another retrospective study of 64 patients over sixty-five years old sustaining falls from standing height with a normal neurological examination, 8 patients (12.5%) had ligamentous injury on MR, with all being determined to be stable injuries and only two of these being managed in a collar, although the reason for managing in a collar was not recorded [23]. No guidelines exist for when to use MRI in elderly/frail patients with a cervical spine fracture, and perhaps further research is required to determine the best role for this imaging modality based on clinical and CT findings. At present, individualised decision-making by an expert in spinal surgery is recommended.
Optimising current management strategies
Current management standards recommended by NICE relate to injuries of the spine in general and are not tailored to the elderly/frail patient [24]. The London major trauma system guidelines for the management of older major trauma patients may be a more applicable framework as they describe facets of management pertinent to elderly patients with more holistic and practical guidance [25]. Recommendations include the use of a standardised ‘A to E’ trauma assessment, immobilisation of the neck and investigation for neurological deficit. Cervical collars may be placed until a fracture has been excluded. However, in patients with ankylosing disorders (e.g. ankylosing spondylitis/DISH) or with severe cervical kyphosis this may be detrimental, thus in such cases or where a collar cannot be safely fitted then immobilisation in the position of the patients deformity, with blocks and tape if possible, is a safer option.
Prolonged bed rest is detrimental to a patient’s health, and even within 24 hours the process of deconditioning occurs [26]. Immobilisation of patients can be extremely harmful, with risks including pneumonia and cardiorespiratory compromise. Over a quarter of patients admitted to hospital lose independence in activities of daily living within three days which will affect their discharge destination and longer term rehabilitation [27]. Prompt diagnosis and specialist assessment of the stability of a patient’s cervical fracture is therefore vital to expedite treatment and the process of rehabilitation. If the fracture is to be managed in a cervical orthosis then this should be provided in the emergency department and the patient should be sat upright and mobilised once other spinal injuries have been excluded.
Hyper-acute rehabilitation is an evolving concept of early mobilisation often within a dedicated multidisciplinary rehabilitation unit with close ties to the acute care unit where the patient was initially managed. In spinal cases, this ensures that spinal medical/surgical expertise continues in a seamless manner from the acute care unit to the rehabilitation unit. Such specialist rehabilitation centres have been demonstrated to improve functional independence and reduce the care-burden in a cost-effective manner within the NHS [28]. Whilst these resources are often already in place for patients with SCI or neurological injury, patients with a fracture without neurological injury may also benefit from intensive multidisciplinary therapy to help improve the chance of getting them back to their baseline state. Community rehabilitation may aid in falls prevention and reduce the risk of re-hospitalisation.
The input of a medical geriatric specialist within a multi-disciplinary team caring for elderly patients following injuries has been demonstrated to reduce complications and length of hospital stay with resultant financial gain for the healthcare system [4]. Orthogeriatric input in patients with hip fractures improved the likelihood of ability to perform activities of daily living independently up to one year following their injury [29]. These results may be mirrored in patients with cervical spine fractures, though this still needs to be formally measured. Specialists in managing elderly/frail patients will provide a holistic assessment of the patient. They can assist in optimising medical management, including pre-operatively which may reduce the risk of subsequent complications. They are also well placed to identify barriers to rehabilitation and how these can be addressed, including factors related to comorbidities, polypharmacy, and sensory deprivation. The role of a structured Orthogeriatric service for cervical spine fractures needs to be better defined, and its cost-effectiveness within the NHS setting needs to be evaluated to help guide future management of these patients.
From a surgical standpoint, the principal goal of fracture management is stabilisation to allow healing across the fracture site; utilising a hard collar, halo brace or surgical fixation. The evidence base for different management modalities in elderly/frail patients is weak. In the UK, hard collars are the most commonly used strategy for cervical fracture management in the elderly/frail, but are still associated with risks including: skin breakdown, breathing or swallowing difficulties, limited mobility, increased risk of falls, and can contribute to delirium [30,31]. Collars may affect the patient and carers’ willingness to mobilise due to fear of causing further damage and exacerbate the effects of prolonged bed-rest/hospitalisation. The long-term physiological and psychosocial sequelae of immobilisation in a collar in this group are also poorly understood. For example, the degree to which the cervical muscles atrophy after a prolonged period in a collar, the long-term physiological effect of this, and to what extent patients recover over time. There is also a paucity of research exploring the psychological sequelae of collar use in this vulnerable group. A current UK randomised control trial (DENS, Duration of External Neck Stabilisation) is investigating whether management of older or frail patients with odontoid fractures without any collar actually improves their quality of life [32].
Where they are used, collars should be regularly checked for adequate fit and the underlying skin checked for pressure sores. Caregivers may be unfamiliar with collars and evidence has demonstrated that appropriate training can dramatically decrease development of pressure ulcers in the inpatient setting [33]. Better communication from specialist centres, education/training and audit may help improve collar care across the NHS in order to reduce complication rates. Collars are usually utilised for 6-12 weeks and discontinued at the discretion of the spinal specialist once safe to do so. Further imaging to assess fracture healing and stability (including dynamic radiographs) may help in this decision-making.
Halo braces are a form of more rigid fixation, with a halo ring that is secured to the skull with pins and attached via pillars to a vest, aiming to achieve a greater reduction of fracture movement and improve bony healing, when compared with a hard collar. However, the complication rate of halo fixation in the elderly/frail patient is particularly high [34], with the use of these devices in spinal surgery generally declining over the last decade [35].
The role of surgical intervention in this cohort of patients is disputed, with disparate views across different healthcare settings. Some authors argue that operative outcomes are satisfactory, with low rates of complications and that operative intervention avoids the requirement for immobilisation and its sequelae [36-38]. Others argue that complication rates are unacceptably high, precluding surgical intervention, and that often patients are satisfied with external immobilisation [39-41]. Mortality rates in some series were similar despite management, with frailty being associated with higher risk of death regardless of treatment modality [42-43].
Often research has focused on the degree of bony fusion across the fracture site, for example fusion is achieved in only 23-82% of type two odontoid fractures managed in a collar, with surgical intervention approaching 100% fusion rates [43]. However, bony fusion has been demonstrated to not be associated with improved functional outcomes in older patients [45-47]. Better-designed research is required in order to understand the outcomes important to patients themselves. This will allow them to better compare treatment options available. Cost effectiveness of management strategies also needed to be assessed, with one study from North America identifying operative treatment of type two odontoid fractures being cost effective in patients 65-84 years old, but not in patients older than 85 years [48]. Further research should examine differences across different cultures and healthcare settings, with a greater focus on frailty indices rather than age and an examination of longer-term outcomes pertinent to patients, alongside cost-efficacy.
Many elderly/frail patients with cervical spine fractures suffer from osteoporosis. One study identified 57% of patients over the age of 70 sustaining a fracture of the odontoid peg had evidence of osteoporosis [11]. Rates of screening for osteoporosis following a spinal fracture are low [49]. In the UK NICE guidelines address the diagnosis and management of osteoporosis, and there is clear evidence of reduction in the risk of vertebral fracture with therapy [50]. Specific interventions encouraging patients and physicians to be cognizant of osteoporosis have been demonstrated to dramatically increase the rate of diagnosis and treatment [51]. Routine imaging studies provide a wealth of information that at present is possibly under recognised and one example is opportunistic assessment for potential underlying osteoporosis. This has been demonstrated as feasible on CT imaging of the spine by assessing the attenuation of the vertebral body in Hounsfield units [8]. This may be beneficial in the context of routine scans in prevention of vertebral fractures, but also in achieving rapid screening following a cervical fracture. Diagnostic bone density scans take time to organise and using existing imaging to screen for osteoporosis may allow earlier treatment of patients in a resource/cost effective manner.
Improving Outcomes for patients
A national cervical fracture database could help drive research and health improvements as the hip fracture database did. It would also make standardisation of care across the NHS, and audit of departmental care, much easier to implement. The national hip fracture database was initially formed by collaboration between the British Orthopaedic Association and the British Geriatric Society, before being commissioned by the Healthcare Quality Improvement Partnership. It is utilised for audit and for payment to NHS trusts by incentivising best practice tariffs for secondary care services. Collaboration of such stakeholder organisations may be necessary to create a similar set of best practice targets for cervical spine fractures that can be audited with a resultant push to improve standards of care.
One essential element in improving care is accurate and meaningful measurement of patient outcomes. Much of the cervical spine injury literature employs outcomes chosen by physicians rather than patients [7]. The choice of measure, and cut-off values vary between studies, which complicates comparisons between differing populations. One of the commonest used outcomes is bony fusion, which may have little value for the patient and seems to be disparate from functional outcomes [40,46,47]. A re-evaluation of the outcomes that should be measured in research is necessary. Many outcome measures have not been validated by key stakeholders and there is a paucity of literature assessing patients’ beliefs and values regarding the definition of a ‘good outcome’ following a cervical fracture [52]. Patients’ self-assessment and expectations regarding their recovery will be greatly context specific, and depend on the injury, their age, pre-existing frailty and comorbidities, alongside their values and beliefs. Each domain of the outcome measures used needs to be relevant, which for many instruments developed for younger patients is not the case when applied to older and frail patients [53]. Thus, to avoid item bias careful selection of the outcome measure tool is imperative [54]. The outcome instrument used should be validated in order to be able to ‘capture change’ [54]. Where fracture is associated with a SCI, patients’ capabilities may evolve during rehabilitation and the rate and extent of change varies between patients, making standardisation of outcomes and comparison difficult [55]. Often there is a dis-concordance between physician- and patient-reported outcomes [56], and patient reported outcome measures (PROMs) assessing patients’ reported quality of life across various domains is vital [57].
Core outcome sets (COS) are “an agreed, standardised set of outcomes to be measured and reported, as a minimum, in all trials” for a particular disease or ‘health area’ [58]. A COS provides consistency in reporting of studies and helps achieve better comparisons of different datasets across differing contexts. The development of a COS for elderly/frail patients with cervical fractures is required. A range of healthcare professionals, patients themselves, and their caregivers should help design this COS, with the aim being to improve future research endeavours.
Conclusions
Learning from the success of innovations in hip fracture management, a coordinated strategy is required to improve the care of elderly/frail patients with cervical spine fractures. The input of a standardised framework that should be adhered to when such a patient is admitted to hospital would improve overall care. Multidisciplinary care including Orthogeriatrics will be instrumental in this. Future research in this field needs to better define the needs of the patient or their caregivers, and assess outcomes that are meaningful to this population in order to compare different management strategies and better serve the individual patient.
References
- Kehoe A, Smith JE, Edwards A, Yates D, Lecky F. The changing face of major trauma in the UK. Emerg Med J. 2015;32(12):911-5. https://doi.org/10.1136/emermed-2015-205265
- Office for Health Improvement and Disparities. Guidance: Falls: applying All Our Health. 2022. https://www.gov.uk/government/publications/falls-applying-all-our-health/falls-applying-all-our-health
- Middleton M. Orthogeriatrics and Hip Fracture Care in the UK: Factors Driving Change to More Integrated Models of Care. Geriatrics (Basel). 2018;3(3). https://doi.org/10.3390/geriatrics3030055
- Cooper Z, Mitchell SL, Lipsitz S, Harris MB, Ayanian JZ, Bernacki RE et al. Mortality and Readmission After Cervical Fracture from a Fall in Older Adults: Comparison with Hip Fracture Using National Medicare Data. J Am Geriatr Soc. 2015;63(10):2036-42. https://doi.org/10.1111/jgs.13670
- Baxter J, Lisk R, Osmani A, Yeong K, Robin J, Fluck D et al. Clinical outcomes in patients admitted to hospital with cervical spine fractures or with hip fractures. Intern Emerg Med. 2021;16(5):1207-13. https://doi.org/10.1007/s11739-020-02567-x
- Delcourt T, Begue T, Saintyves G, Mebtouche N, Cottin P. Management of upper cervical spine fractures in elderly patients: current trends and outcomes. Injury. 2015;46 Suppl 1:S24-7. https://doi.org/10.1016/S0020-1383(15)70007-0
- Copley PC, Tadross D, Salloum N, Woodfield J, Edlmann E, Poon M et al. A systematic review identifying outcome measures used in evaluating adults sustaining cervical spine fractures. Eur Spine J. 2022. https://doi.org/10.1007/s00586-022-07369-7
- Emohare O, Dittmer A, Morgan RA, Switzer JA, Polly DW, Jr. Osteoporosis in acute fractures of the cervical spine: the role of opportunistic CT screening. J Neurosurg Spine. 2015;23(1):1-7. https://doi.org/10.3171/2014.10.SPINE14233
- Mulla E, Orton E, Kendrick D. Is proactive frailty identification a good idea? A qualitative interview study. Br J Gen Pract. 2021;71(709):e604-e13. https://doi.org/10.3399/BJGP.2020.0178
- British Geriatric Society. Fit for frailty part 1. Consensus best practice guidance for the care of older people living in community and outpatient settings. 2017.
- Lakshmanan P, Jones A, Howes J, Lyons K. CT evaluation of the pattern of odontoid fractures in the elderly–relationship to upper cervical spine osteoarthritis. Eur Spine J. 2005;14(1):78-83. https://doi.org/10.1007/s00586-004-0743-z
- Stiell IG, Wells GA, Vandemheen KL, Clement CM, Lesiuk H, De Maio VJ et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286(15):1841-8. https://doi.org/10.1001/jama.286.15.1841
- Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-9. https://doi.org/10.1056/NEJM200007133430203
- Jambhekar A, Lindborg R, Chan V, Fulginiti A, Fahoum B, Rucinski J. Over the hill and falling down: Can the NEXUS criteria be applied to the elderly? Int J Surg. 2018;49:56-9. https://doi.org/10.1016/j.ijsu.2017.12.009
- Paykin G, O’Reilly G, Ackland HM, Mitra B. The NEXUS criteria are insufficient to exclude cervical spine fractures in older blunt trauma patients. Injury. 2017;48(5):1020-4. https://doi.org/10.1016/j.injury.2017.02.013
- Paykin G, O’Reilly G, Ackland H, Mitra B. Review article: NEXUS criteria to rule out cervical spine injury among older patients: A systematic review. Emerg Med Australas. 2018;30(4):450-5. https://doi.org/10.1111/1742-6723.12880
- The National Institute for Health and Care Excellence (NICE). Quality standard [QS74]: Head Injury. 2014. https://www.nice.org.uk/guidance/qs74/chapter/quality-statement-3-ct-cervical-spine-scans. Accessed 11/09/22 2022.
- Tebby-Lees S HP. R.C.R. standards for cervical spine x-rays in trauma – a tall order! A case for direct CT scan for elderly falling from standing. 2016. https://www.rcr.ac.uk/sites/default/files/cervical_spine_xrays_trauma.pdf.
- Sadro CT, Sandstrom CK, Verma N, Gunn ML. Geriatric Trauma: A Radiologist’s Guide to Imaging Trauma Patients Aged 65 Years and Older. Radiographics. 2015;35(4):1263-85. https://doi.org/10.1148/rg.2015140130
- Page PS, Josiah DT. Traumatic vertebral artery injuries in the geriatric population: a retrospective cohort study. J Neurosurg Spine. 2020:1-4. https://doi.org/10.3171/2019.11.SPINE191055
- Harrigan MR, Hadley MN, Dhall SS, Walters BC, Aarabi B, Gelb DE et al. Management of vertebral artery injuries following non-penetrating cervical trauma. Neurosurgery. 2013;72 Suppl 2:234-43. https://doi.org/10.1227/NEU.0b013e31827765f5
- Pourtaheri S, Emami A, Sinha K, Faloon M, Hwang K, Shafa E et al. The role of magnetic resonance imaging in acute cervical spine fractures. Spine J. 2014;14(11):2546-53. https://doi.org/10.1016/j.spinee.2013.10.052
- Cushing CH, Holmes JF, Tyler KR. Cervical Spine Injuries in Older Patients with Falls Found on Magnetic Resonance Imaging After Computed Tomography. West J Emerg Med. 2021;22(5):1190-5. https://doi.org/10.5811/westjem.2021.5.51844
- The National Institute for Health and Care Excellence (NICE). Spinal injury: assessment and initial management (NG41). 2016. https://www.nice.org.uk/guidance/ng41/resources/spinal-injury-assessment-and-initial-management-pdf-1837447790533.
- London Major Trauma system. Management of Older Major Trauma Patients, 3rd ed. 2021. p. https://www.c4ts.qmul.ac.uk/downloads/pan-london-major-trauma-system-management-of-older-trauma.-third-editionapril-2021.pdf.
- Guedes LPCM, Oliveira MLCd, Carvalho GdA. Deleterious effects of prolonged bed rest on the body systems of the elderly – a review. Rev bras geriatr gerontol 2018;21(4):499-506. https://doi.org/10.1590/1981-22562018021.170167
- King BD. Functional decline in hospitalized elders. Medsurg Nurs. 2006;15(5):265-71; quiz 72.
- Turner-Stokes L, Bavikatte G, Williams H, Bill A, Sephton K. Cost-efficiency of specialist hyperacute in-patient rehabilitation services for medically unstable patients with complex rehabilitation needs: a prospective cohort analysis. BMJ Open. 2016;6(9):e012112. https://doi.org/10.1136/bmjopen-2016-012112
- Dakhil S, Thingstad P, Frihagen F, Johnsen LG, Lydersen S, Skovlund E et al. Orthogeriatrics prevents functional decline in hip fracture patients: report from two randomized controlled trials. BMC Geriatr. 2021;21(1):208. https://doi.org/10.1186/s12877-021-02152-7
- Peck GE, Shipway DJH, Tsang K, Fertleman M. Cervical spine immobilisation in the elderly: a literature review. British journal of neurosurgery. 2018;32(3):286-90. https://doi.org/10.1080/02688697.2018.1445828
- Sime D, Pitt V, Pattuwage L, Tee J, Liew S, Gruen R. Non-surgical interventions for the management of type 2 dens fractures: a systematic review. ANZ journal of surgery. 2014;84(5):320-5. https://doi.org/10.1111/ans.12401
- Woodfield J, Edlmann E, Black PL, Boyd J, Copley PC, Cranswick G et al. Duration of External Neck Stabilisation (DENS) following odontoid fracture in older or frail adults: protocol for a randomised controlled trial of collar versus no collar. BMJ Open. 2022;12(7):e057753. https://doi.org/10.1136/bmjopen-2021-057753
- Alphons M. Reduce Incidences of Pressure Ulcers due to wearing rigid collars. 2019. https://www.gloshospitals.nhs.uk/media/documents/Alphons_Mathew.pdf. Accessed 11/09/22 2022.
- Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005;59(2):350-6; discussion 6-8. https://doi.org/10.1097/01.ta.0000174671.07664.7c
- Kurucan E, Sulovari A, Thirukumaran C, Greenstein A, Molinari R, Mesfin A. Volume-outcome relationship in halo vest utilization for C2 fractures. Spine J. 2020;20(10):1676-84. https://doi.org/10.1016/j.spinee.2020.05.543
- Issa M, Kiening KL, Unterberg AW, Scherer M, Younsi A, Fedorko S et al. Morbidity and Mortality in Patients over 90 Years of Age Following Posterior Stabilization for Acute Traumatic Odontoid Type II Fractures: A Retrospective Study with a Mean Follow-Up of Three Years. J Clin Med. 2021;10(17). https://doi.org/10.3390/jcm10173780
- Schoenfeld AJ, Bono CM, Reichmann WM, Warholic N, Wood KB, Losina E et al. Type II odontoid fractures of the cervical spine: do treatment type and medical comorbidities affect mortality in elderly patients? Spine (Phila Pa 1976). 2011;36(11):879-85. https://doi.org/10.1097/BRS.0b013e3181e8e77c
- Godat LN, Kobayashi LM, Chang DC, Coimbra R. Improving life expectancy: A ‘broken neck’ doesn’t have to be a terminal diagnosis for the elderly. Trauma Surg Acute Care Open. 2018;3(1):e000174. https://doi.org/10.1136/tsaco-2018-000174
- Rizvi SAM, Helseth E, Ronning P, Mirzamohammadi J, Harr ME, Brommeland T et al. Odontoid fractures: impact of age and comorbidities on surgical decision making. BMC Surg. 2020;20(1):236. https://doi.org/10.1186/s12893-020-00893-7
- McIlroy S, Lam J, Khan MF, Mirza AB, Philip JA, Grahovac G et al. Conservative Management of Type II Odontoid Fractures in Older People: A Retrospective Observational Comparison of Osseous Union Versus Nonunion. Neurosurgery. 2020;87(6):E648-E54. https://doi.org/10.1093/neuros/nyaa256
- Fam MD, Zeineddine HA, Nassir RM, Bhatt P, Kamel MH. Patient-reported outcome following nonsurgical management of type II odontoid process fractures in adults. J Craniovertebr Junction Spine. 2017 Jan-Mar;8(1):64-69. https://doi.org/10.4103/0974-8237.199871
- Borsotti F, Starnoni D, Ecker T, Coll JB. One-year follow-up for type II odontoid process fractures in octogenarians: Is there a place for surgical management? Surg Neurol Int. 2020;11:285. https://doi.org/10.25259/SNI_376_2020
- Carlstrom LP, Helal A, Perry A, Lakomkin N, Graffeo CS, Clarke MJ. Too frail is to fail: Frailty portends poor outcomes in the elderly with type II odontoid fractures independent of management strategy. J Clin Neurosci. 2021;93:48-53. https://doi.org/10.1016/j.jocn.2021.08.027
- Pal D, Sell P, Grevitt M. Type II odontoid fractures in the elderly: an evidence-based narrative review of management. Eur Spine J. 2011;20(2):195-204. https://doi.org/10.1007/s00586-010-1507-6
- McIlroy S, Lam J, Khan MF, Mirza AB, Philip JA, Grahovac G et al. Conservative Management of Type II Odontoid Fractures in Older People: A Retrospective Observational Comparison of Osseous Union Versus Nonunion. Neurosurgery. 2020. https://doi.org/10.1093/neuros/nyaa256
- Lofrese G, Musio A, De Iure F, Cultrera F, Martucci A, Iaccarino C et al. Type II odontoid fracture in elderly patients treated conservatively: is fracture healing the goal? Eur Spine J. 2019;28(5):1064-71. https://doi.org/10.1007/s00586-019-05898-2
- Perry A, Graffeo CS, Carlstrom LP, Chang W, Mallory GW, Puffer RC et al. Fusion, Failure, Fatality: Long-term Outcomes After Surgical Versus Nonoperative Management of Type II Odontoid Fracture in Octogenarians. World neurosurgery. 2018;110:e484-e9. https://doi.org/10.1016/j.wneu.2017.11.020
- Barlow DR, Higgins BT, Ozanne EM, Tosteson AN, Pearson AM. Cost Effectiveness of Operative Versus Non-Operative Treatment of Geriatric Type-II Odontoid Fracture. Spine (Phila Pa 1976). 2016;41(7):610-7. https://doi.org/10.1097/BRS.0000000000001275
- Barton DW, Behrend CJ, Carmouche JJ. Rates of osteoporosis screening and treatment following vertebral fracture. Spine J. 2019;19(3):411-7. https://doi.org/10.1016/j.spinee.2018.08.004
- Compston J, Cooper A, Cooper C, Gittoes N, Gregson C, Harvey N et al. UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 2017;12(1):43. https://doi.org/10.1007/s11657-017-0324-5
- Majumdar SR, McAlister FA, Johnson JA, Bellerose D, Siminoski K, Hanley DA et al. Interventions to increase osteoporosis treatment in patients with ‘incidentally’ detected vertebral fractures. Am J Med. 2012;125(9):929-36. https://doi.org/10.1016/j.amjmed.2012.02.021
- Schoenfeld AJ, Bono CM. Measuring spine fracture outcomes: common scales and checklists. Injury. 2011;42(3):265-70. https://doi.org/10.1016/j.injury.2010.11.040
- Louie C, D’Agostino EN, Han D, Ryken TC. Determining an Appropriate Outcome Measure in Neurosurgical Research: Investigating Meaningful, Valid, and Practical Metrics. Cureus. 2019;11(9):e5610. https://doi.org/10.7759/cureus.5610
- Coster WJ. Making the best match: selecting outcome measures for clinical trials and outcome studies. Am J Occup Ther. 2013;67(2):162-70. https://doi.org/10.5014/ajot.2013.006015
- Duncan PW, Jorgensen HS, Wade DT. Outcome measures in acute stroke trials: a systematic review and some recommendations to improve practice. Stroke. 2000;31(6):1429-38. https://doi.org/10.1161/01.STR.31.6.1429
- Pakhomov SV, Jacobsen SJ, Chute CG, Roger VL. Agreement between patient-reported symptoms and their documentation in the medical record. Am J Manag Care. 2008;14(8):530-9.
- van der Vorst A, Zijlstra GAR, De Witte N, Vogel RGM, Schols J, Kempen G et al. Explaining discrepancies in self-reported quality of life in frail older people: a mixed-methods study. BMC Geriatr. 2017;17(1):251. https://doi.org/10.1186/s12877-017-0641-y
- Williamson PR, Altman DG, Blazeby JM, Clarke M, Devane D, Gargon E et al. Developing core outcome sets for clinical trials: issues to consider. Trials. 2012;13:132. https://doi.org/10.1186/1745-6215-13-132



