Epilepsy is amongst the most common neurological conditions with incidence rates, in developed countries, ranging between 40 and 70/100,000 persons/year and even higher rates in children and elderly people. As captured by the new definition,1 epilepsy is now recognised as a disorder of the brain characterised not only by recurrent seizures, but also by its neurobiological, cognitive, psychological and social consequences. For a long time the mutual relationships among epilepsy, seizures and behaviour have been matter of debate, fascinating generations of clinicians and neuroscientists. In his famous quotation, Hippocrates reported that “melancholics ordinarily become epileptics, and epileptics, melancholics: what determines the preference is the direction the malady takes; if it bears upon the body, epilepsy, if upon the intelligence, melancholy”. This early observation has been recently revitalised by modern epidemiological studies pointing out a bidirectional relationship between epilepsy and psychiatric disorders.2
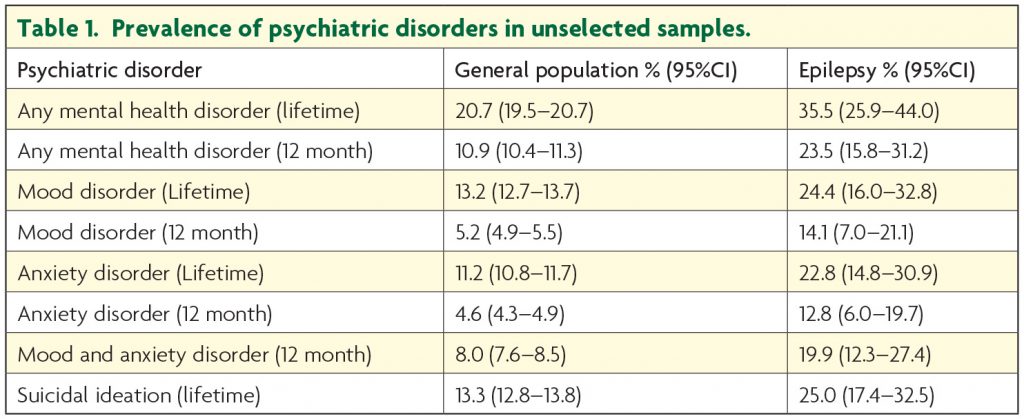
In general terms, psychiatric problems show a uniformly increased prevalence in epilepsy as compared to the general population3 (Table 1). In some cases, this partially reflects the severity of the seizure disorder as prevalence rates are higher in subjects with refractory syndromes as compared to patients with well controlled epilepsies but in other cases the clinical scenario is more complex than that.4 In fact, for example, a population-based study showed that the rate ratio of suicide in people with epilepsy remains doubled even after excluding patients with psychiatric comorbidities and adjusting for various factors.5 Data from the SANAD trial showed that newly diagnosed untreated patients with epilepsy are already cognitively compromised before any treatment is started, independently by the underlying cause.6 It is clearly evident that epilepsy is characterised by a number of clinical manifestations that comprise also cognitive and behavioural symptoms that, in same selected cases, can even precede the onset of seizures themselves.
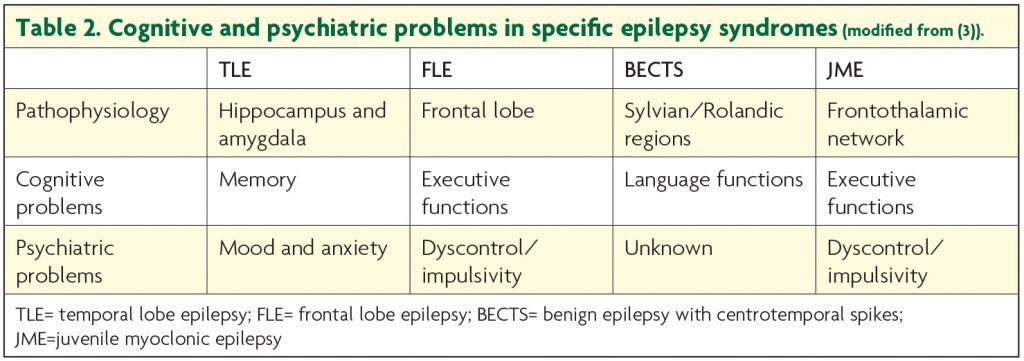
As any epileptologist is aware of, treatment and prognosis of epilepsy rely on the accurate identification of the specific syndrome defined by a collection of clinical variables (e.g. age of onset, seizure pattern) and laboratory findings (e.g. EEG and MRI). Although it sounds logical to apply the same model for cognitive and behavioural problems of epilepsy (Table 2), much remains unknown regarding the contribution of shared versus syndrome-specific variables and clinical evidence suggests that especially behavioural problems do not necessarily respect such boundaries.
Mood and anxiety disorders
Mood and anxiety disorders are the most frequently reported psychiatric problems with prevalence rates up to 50% in selected populations, such as tertiary referral centres or surgery programmes.1,3 Mood and anxiety problems were historically attributed due to the number of social limitations (e.g. driving licence, job opportunities etc.), discrimination and stigmatisation even today connected with a diagnosis of epilepsy.7 It is now evident that there is a solid neurobiological ground linking epilepsy to mood disorders such as the involvement of the mesiotemporal structures (hippocampus and amygdala) and the modulation of major neurotransmitter pathways (especially serotonin) by the epilepsy process and the antiepileptic drug treatment. Nonetheless, mood disorders are still unrecognised and untreated due to multiple reasons: i) lack of time during busy clinics, ii) lack of specific training by the treating neurologist in recognising mood disorders, iii) reluctance of the patient in acknowledging mental health issues. In addition, psychiatrists may also fail to diagnose mood disorders in epilepsy due to the high frequency of atypical clinical presentations, not fulfilling DSM or ICD criteria for a major depressive episode. In fact, up to 50% of patients with epilepsy and depression present with symptoms which are not considered diagnostic8 because they are either too short in duration or they come in isolation. This notion has been eloquently discussed by Dietrich Blumer when he described the interictal dysphoric disorder (IDD).9 The concept of IDD goes back to the original observations of Kraepelin and Bleuler, who described a pleomorphic pattern of depressive symptoms, intermixed with euphoric moods, irritability, fear and anxiety in patients with untreated epilepsy. Although the concept of IDD still remains controversial,10 it is clearly evident that, for example, looking for typical biological symptoms of depression (e.g. insomnia or hypersomnia, reduced or increased appetite, sexual dysfunction etc.) is of limited value in patients with epilepsy as these symptoms can be influenced by the underlying disorder or the antiepileptic drug treatment. In addition, patients may often present with isolated or atypical symptoms (e.g. irritable/unstable moods, somatic symptoms) that are part of a mood disorder, deserving clinical attention and proper management even if it does not fulfil a categorical diagnosis. Recent research focused on screening instruments specifically developed for patients with epilepsy in order to overcome most of these problems. The Neurological Depression Inventory of Epilepsy (NDDIE) is an example.11 In this context, it is easy to understand why suicide in epilepsy is still underestimated. Suicide represents, in the general population, the 11th cause of death, the 2nd in the group aged 25 to 34 years, but the overall risk is about three times higher in patients with epilepsy.3 A number of studies tried to clarify potential reasons for that and there is still an on-going debate about the potential role of antiepileptic drugs. Many years after the Food and Drug Administration (FDA) issued the alert on a potential increased risk of suicide ideation and behaviour in people with epilepsy treated with AEDs, it seems now evident that the FDA warning was based on data affected by a number of methodological limitations.12 Suicide in epilepsy is likely to be multifactorial in origin with biological, constitutional and psychosocial factors implicated, but specific programmes for screening and prevention are urgently needed.
Psychoses and thought disorders
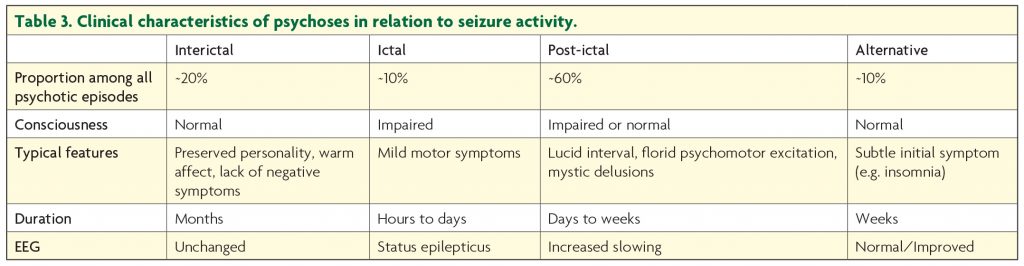
Although definitely less common than mood disorders, psychoses still represent a serious complication in patients with epilepsy affecting management and long-term prognosis. Prevalence rates for any thought disorder can be up to 4% in epilepsy, especially in hospital case series.3 Psychoses of epilepsy (POE) have fascinated neuropsychiatrists for decades. They are conveniently classified according to their temporal relationship with seizures as peri-ictal or inter-ictal. Peri-ictal psychotic symptoms are more frequent than interictal ones with post-ictal psychoses (PIP), being probably the most frequently described (Table 3). PIPs are precipitated by a cluster of convulsions and are characterised by a period of normal mental state of 24-48 hours, also known as the lucid interval.13 The pathophysiology of PIP is still unknown but seems to be related to that of the epilepsy. In fact, it is a highly stereotyped phenomenon, occurring mainly in patients with temporal lobe epilepsy and extra-temporal structural lesions.14 Although PIPs are often characterised by spontaneous remission within days or weeks, antipsychotic drug treatment is required to reduce mortality and morbidity. In fact, the phenomenology of PIPs is characterised by aggressive behaviour and a florid psychomotor excitation often accompanied by a mystic delusion.14 Chronic interictal psychoses (IIPs) represent nowadays a rare complication and the general impression is that this is probably due to a better and timely treatment of the epilepsy. IIPs usually develop subtly after many years of active lesional temporal lobe epilepsy due to, for example, hamartomas and gangliogliomas or other gross abnormalities.15 If IIPs seem to occur less frequently than before, post-surgery psychoses represent a coming complication. Some patients are probably at increased risk and this is due to a specific neuropathological process not entirely elucidated.16 The early identification of patients at risk during the pre-surgical assessment clearly deserves future research.
Finally, it is important to mention the Landolt’s phenomenon, also known as “forced normalisation” or “paradoxical normalisation”.17 Originally described as an electrophysiological phenomenon associated with a particular class of antiepileptic drugs, namely suximides, subsequent case series described a similar clinical pattern with all antiepileptic drugs, clearly pointing out that it is not drug-specific. In addition, recent case series reported the forced normalisation phenomenon in patients treated with vagus nerve stimulation and possibly after surgery. The pathophysiology is still obscure but it seems evident that, in some patients, the neurobiological mechanisms underlying seizure control antagonise normal thought processes. As already mentioned for psychoses after surgery, it will be important to identify specific biomarkers in order to recognise patients at increased risk.
The use of psychotropic medications in epilepsy
Data on treatment of psychiatric disorders in epilepsy are still limited and based mainly on clinical observations but during recent years, the International League Against Epilepsy has published a number of recommendations that represent a good reference for clinicians.18,19 In general terms, internationally accepted guidelines for treatment of psychiatric disorders outside epilepsy should be adopted, taking into account all peculiarities of this special group of patients such as drug interactions and the potential effect of some drugs on seizure threshold.
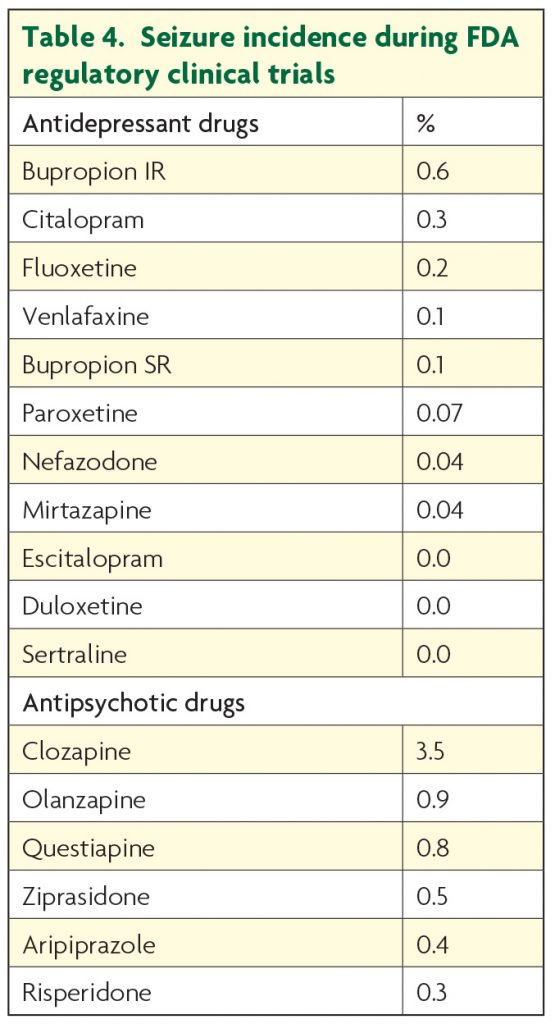
New generations of both antidepressants and antipsychotics can be considered reasonably safe in patients with epilepsy, if appropriately prescribed in terms of titration and dosages. Among antidepressants, maprotiline, high dose of clomipramine and amitriptyline (>200mg), high doses of bupropion immediate release formulation (>450mg) may represent a concern. Among all antipsychotics, clozapine is the only one associated with a significant increased risk of seizures.20 However, it is important to point out that available data comes from psychiatric samples (Table 4) and there is no data about seizure worsening in patients with epilepsy that are on a stable anticonvulsant regime. For this reason, any a priori assumption that psychotropic medications (even those just mentioned) are contraindicated in epilepsy is not based on any scientific evidence. The “start low/go slow” statement should always represent a starting point, bearing in mind that low starting doses do not necessarily correspond to low target doses and full remission from psychiatric symptoms has to be the primary goal of any psychopharmacological intervention.
Psychiatric disorders in epilepsy necessarily need to be approached by a multidisciplinary team because multiple skills and inputs from different specialists are needed. Still, true psychiatric symptoms should be distinguished from seizure-based behavioural manifestations in order to develop tailored treatment strategies. Continued clinical research and education are needed to grasp further insights into the fascinating relationship among epilepsy, seizures and behaviour and to provide the best care for patients with epilepsy.
Take home messages
- The new definition of epilepsy implies not only an enduring predisposition to generate seizures, but also its neurobiological, cognitive, psychological and social consequences.
- Epilepsy care need to be approached by a multidisciplinary team.
- The first goal in the treatment of any psychiatric problem in epilepsy should be full remission.
- Guidelines for treatment of psychiatric disorders outside epilepsy should be adopted taking into account individual patient needs, drug-drug interactions and risk of seizure relapse.
- Any psychotropic drug should be slowly introduced and slowly titrated according to clinical response bearing in mind that low starting doses do NOT necessarily mean low target doses.
References
- Fisher RS, Acevedo C, Arzimanoglou A, Bogacz A, Cross JH, Elger CE, Engel J Jr, Forsgren L, French JA, Glynn M, Hesdorffer DC, Lee BI, Mathern GW, Moshé SL, Perucca E, Scheffer IE, Tomson T, Watanabe M, Wiebe S. ILAE official report: a practical clinical definition of epilepsy. Epilepsia. 2014 Apr;55(4):475-82.
- Mula M. Epilepsy: Bidirectional link between epilepsy and psychiatric disorders. Nat Rev Neurol 2012;8:252-253.
- Lin JJ, Mula M, Hermann BP. Uncovering the neurobehavioural comorbidities of epilepsy over the lifespan. Lancet 2012;380:1180-1192.
- Tellez-Zenteno JF, Patten SB, Jette N, Williams J, Wiebe S. Psychiatric comorbidity in epilepsy: a population-based analysis. Epilepsia 2007;48:2336-2344.
- Christensen J, Vestergaard M, Mortensen PB, Sidenius P, Agerbo E. Epilepsy and risk of suicide: a population-based case-control study. Lancet Neurol. 2007;6:693-8.
- Taylor J, Kolamunnage-Dona R, Marson AG, Smith PE, Aldenkamp AP, Baker GA. Patients with epilepsy: cognitively compromised before the start of antiepileptic drug treatment? Epilepsia 2010;51:48-56.
- de Boer HM, Mula M, Sander JW. The global burden and stigma of epilepsy. Epilepsy Behav 2008;12:540-546
- Kanner AM. Depression in epilepsy: a frequently neglected multifaceted disorder. Epilepsy Behav 2003;4 Suppl 4:11-19.
- Blumer D. Dysphoric disorders and paroxysmal affects: recognition and treatment of epilepsy-related psychiatric disorders. Harv Rev Psychiatry 2000;8:8-17.
- Mula M. The interictal dysphoric disorder of epilepsy: a still open debate. Curr Neurol Neurosci Rep. 2013;13:355.
- Gilliam FG, Barry JJ, Hermann BP, Meador KJ, Vahle V, Kanner AM. Rapid detection of major depression in epilepsy: a multicentre study. Lancet Neurol. 2006;5:399-405.
- Mula M, Sander JW. Suicide and epilepsy: do antiepileptic drugs increase the risk? Expert Opin Drug Saf. 2015;14:553-8.
- Trimble MR. The psychoses of epilepsy. New York: Raven Press, 1991.
- Kanemoto K, Kawasaki J, Kawai I. Postictal psychosis: a comparison with acute interictal and chronic psychoses. Epilepsia 1996;37:551-556
- Adachi N, Akanuma N, Ito M, Okazaki M, Kato M, Onuma T. Interictal psychotic episodes in epilepsy: duration and associated clinical factors. Epilepsia. 2012;53(6):1088-94
- Thom M, Kensche M, Maynard J, Liu J, Reeves C, Goc J, Marsdon D, Fluegel D, Foong J. Interictal psychosis following temporal lobe surgery: dentate gyrus pathology. Psychol Med. 2014;44:3037-49
- Trimble MR, Schmitz B. Forced normalization and alternative psychoses of epilepsy. Petersfield: Wrightson Biomedical Pub. Ltd., 1998.
- Kerr MP, Mensah S, Besag F, de Toffol B, Ettinger A, Kanemoto K, Kanner A, Kemp S, Krishnamoorthy E, LaFrance WC Jr, Mula M, Schmitz B, van Elst LT, Trollor J, Wilson SJ, International League of Epilepsy (ILAE) Commission on the Neuropsychiatric Aspects of Epilepsy. International consensus clinical practice statements for the treatment of neuropsychiatric conditions associated with epilepsy. Epilepsia. 2011;52(11):2133-8
- Mula M, Kanner AM. Introduction–Treatment of psychiatric disorders in adults with epilepsy: what every epileptologist should know. Epilepsia. 2013;54(Suppl 1):1-2
- Alper K, Schwartz KA, Kolts RL, Khan A. Seizure incidence in psychopharmacological clinical trials: an analysis of Food and Drug Administration (FDA) summary basis of approval reports. Biol Psychiatry. 2007;62(4):345-54.
