Abstract
Aggression is common after traumatic brain injuries (TBI) in acute and chronic settings. However, there is limited guidance regarding its assessment and effective management. Whilst a number of pharmacological options are available for long term treatment, the evidence base is not of an adequate strength to support a unified practice. This article will explore the currently available guidelines and recommendations for treating chronic aggression after TBIs and evaluate the evidence for its pharmacological management.
Introduction
Aggression is a long term neurobehavioural sequelae of TBIs with incidences quoted from 11.5-33.7%.1 In TBI patients, aggressive behaviour tends to be impulsive rather than premeditated and can manifest as episodic dyscontrol syndrome, disinhibition or exacerbated premorbid antisocial traits.2 The underlying mechanisms of aggression are complex allowing numerous and diverse interventions targeting various pathways.
In acute settings, Lombard and Zafonte (2005) describe non-pharmacological measures to manage aggression including environmental alterations and ensuring minimal or non-contact restraints. Screening for systemic causes, optimising pain control and patients’ sleep-wake cycle are also advocated. In the event of failed non-pharmacological treatment, Lombard and Zafonte (2005) recommend that medication choice should be tailored to individuals; with side effect profiles taken into consideration.3
For chronic aggression, psychological therapies are used as a first line with pharmacological interventions trialled in later stages.4 Psychological therapy options include cognitive behavioural therapy (CBT), behavioural management utilising operant learning theory and contingency management. However, a review by Alderman (2013) concluded that further evidence using scientific methods is needed to analyse these approaches.5 Comparatively, there is a diverse body of literature addressing long term pharmacological treatment although quality among studies are varied. This article will focus on the aetiology for chronic post TBI aggression, current management guidelines and the evidence for long term pharmacological interventions.
Aetiology
Post TBI aggression has been associated with lesions affecting the prefrontal cortex – particularly the orbitofrontal and ventromedial areas – causing a loss of behavioural regulation. Disruption to inhibitory pathways between the prefrontal cortex and limbic system also results in limbic kindling and inappropriate emotional responses to negative stimuli thus facilitating aggressive behaviour.2 Associated neurotransmitter abnormalities include low cortical serotonin and impaired gamma amino-butyric acid (GABA)/ glutamate levels.6 Altered catecholamine and cholinergic levels are associated with cognitive impairment2 thus distorting information processing and predisposing patients to aggression.6 In TBI patients, underlying anxiety, affective disorders, seizures and frontal lobe dysfunction also increase susceptibility.10
Differentials for aggression
When identifying a cause for chronic aggressive behaviour, a patient’s previous experiences, comorbid psychiatric conditions and alcohol and/or substance abuse must be established with a collateral history.2,7 McAllister (2008) highlights the importance of determining pre-injury behaviour in order to exclude the possibility of symptoms being an exaggeration of pre-injury personality traits.8 Additionally, psychosocial factors must be deduced to identify possible triggers.2,7
Clinicians must be aware that aggression can be a presenting feature of other psychiatric disorders. Depression has a prevalence of 18.5% to 61% in post-TBI patients and is linked with aggression due to their shared association with frontal lobe lesions and serotonin level imbalance.9 Other differentials include manic disorders (which can involve a more marked aggressive component if secondary to TBIs), anxiety disorders and alcohol and/or substance abuse. Personality and behavioural disorders such as affective lability, behavioural disinhibition and acquired antisocial behaviour should also be considered.8
Management guidelines
The National Institute for Health and Care Excellence (NICE) refers to the Scottish Intercollegiate Guidelines Network (SIGN) for rehabilitating patients with acquired brain injuries (ABIs). Psychological treatments advocated by SIGN include CBT, contingency management procedures, music therapy and comprehensive neurobehavioural rehabilitation (CNR).10 Family involvement appears to be associated with better outcomes2 and is also recommended.10
Of the studies quoted by SIGN, CNR was found to cause a positive effect in ABI patients in one systematic review although inconsistent results were obtained for the other three methods. Regarding pharmacological treatment, SIGN advises propranolol and pindolol as first line options.10
Pharmacological treatment
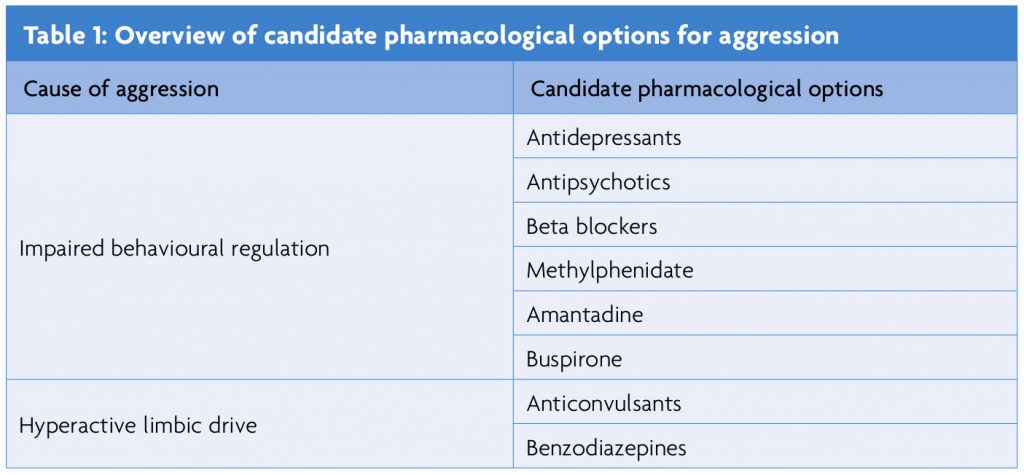
The aberrant neurotransmitter changes in the cortex and limbic areas as a result of TBIs2 provide targets for pharmacological therapy (as summarised in Table 1). Theoretically, cortical behavioural regulation can be enhanced by serotonergic agents and antagonists of dopaminergic and noradrenergic neurotransmission. Limbic hyperactivity can be dampened by the use of gamma aminobutyric acid (GABA) agonists, glutamatergic antagonists and anticholinergics.6
Impaired behavioural regulation
Antidepressants
Selective serotonin reuptake inhibitors (SSRIs) are indicated for their increase in dopamine and serotonin availability and the treatment of depression contributing to aggressive behaviour. In a trial conducted by Kant et al (1998), sertraline reduced aggression within one week of treatment although TBI severities were variable within the population.11 These results are mirrored in other trials presenting sertraline as a viable treatment option.12 Citalopram used in conjunction with carbamazepine successfully treated behavioural symptoms in a clinical trial of 22 patients conducted by Perino et al (2001)13 although the separate effects of both drugs are impossible to differentiate. A case study by Sloan et al (1992) found that fluoxetine improved emotional lability in one patient within a week.13
Tricyclic antidepressants have been shown to be useful for managing both post-traumatic and chronic aggression. Amitriptyline has reduced aggression with good tolerability despite its strong anticholinergic side effects in several studies and is suggested as the best option for treating behavioural disorders secondary to frontal lobe injuries without impairing cognition.13
Antipsychotics
There is a wide body of literature advocating antipsychotics for managing aggression due to their sedative effects.13 Nevertheless, the cognitive and extrapyramidal side effects of typical antipsychotics limit their value for chronic use. Comparatively, atypical antipsychotics have a milder side effect profile and are preferred although their cognitive impact in TBI patients is unclear.2 Furthermore, unlike older generations, atypical antipsychotics antagonise 5HT2 receptors and are therefore implicated in reduced aggression.9
Of the typical antipsychotics, chlorpromazine reduced explosiveness in one case study conducted by Sandel et al (1993). Various case studies also report haloperidol improving chronic agitation in TBI patients although significant side effects were encountered.13 Of the atypical antipsychotics the level of evidence is low. Quetiapine reduced aggression and irritability in seven patients in a trial conducted by Kim and Bijlani (2006).11 Olanzapine significantly reduced aggression within six months in a case study conducted by Umansky and Geller (2000). Clozapine was associated with varying levels of improvement in six case studies conducted by Michals et al (1993) however seizures were experienced in two patients.13
Overall, there is no reliable evidence advocating antipsychotic use for managing chronic post-TBI aggression. If antipsychotics are commenced for this purpose, it is suggested that their use is restricted to patients with psychosis.13
Beta blockers
Beta blockers are useful for cases where aggression is caused by underlying anxiety13 due to its inhibition of noradrenergic levels.9 A Cochrane review of four RCTs found that pindolol and propranolol reduced aggression within two to six weeks of starting treatment in ABI patients however no recommendations were made due to heterogeneity between samples, a small number of trials and small sample sizes. The authors acknowledge that the trials involved high doses and so recommend caution when prescribing beta blockers for aggression.4
Methylphenidate
Methylphenidate is a psychostimulant indicated for its enhancement of dopamine and noradrenaline in the frontal lobe improving arousal and alertness.13 Mooney (1993) found in a single RCT that methylphenidate significantly improved anger scores in TBI patients.4 However other studies have yielded mixed results12,13 and no firm conclusion can be made.
Amantadine
Amantadine increases dopamine availability and acts on glutamatergic pathways. An advantage of its use is its non-sedating qualities however there is contradicting evidence for its efficacy.13 An RCT conducted by Schneider (1999) found no significant improvement4 however the trial was limited by a small sample size and large heterogeneity. Interestingly, studies of a lower level of evidence demonstrate favourable results.13 Due to this variability, its efficacy is still in question.
Buspirone
Buspirone – a serotonergic agonist licensed for treating anxiety13 – has also reduced aggression in several case studies2,12,14 warranting further research. Its side effects are amenable for use in TBIs although one disadvantage is its delayed onset.13
Hyperactive limbic drive
Anticonvulsants
The mood stabilising effects of anticonvulsants are mediated through their enhancement of GABA transmission.2 Carbamazepine has been demonstrated in studies to be effective for managing acute and chronic post- TBI aggression.12,13 Its side effects include impaired balance, sedation13 and cognitive impairment particularly in brain injured patients2 due to their heightened sensitivity. In a trial conducted by Mattes (2005), Oxcarbazepine reduced impulsive aggression however the number of TBI participants in the sample was unclear. Nine of the 48 participants also dropped out due to adverse effects11 suggesting more research is needed into its tolerability in TBI patients. Valproate has also been demonstrated to effectively manage behavioural and affective disorders13 with a milder cognitive impact compared to carbamazepine.2 Regarding other anticonvulsants, the evidence is of a lower standard. Pachet et al (2003) found that lamotrigine reduced aggression with good tolerability in one case study.11 Topiramate has been demonstrated to effectively treat manic symptoms but due to its side effects of psychosis and cognitive impairment,2 may be inappropriate for TBI patients. Case reports reference lithium to reduce post – TBI agitation however it may be unsuitable as a first line option due to its neurotoxicity.13
Benzodiazepines
Benzodiazepines are indicated for their anticonvulsive, anti-anxiety and sedative qualities facilitated by stimulation of the GABA receptor.13 There is limited literature on their chronic use in TBI patients due to their side effects of agitation, cognitive impairment and tolerance2 thus they are recommended to be more appropriate for cases of acute agitation or anxiety.11
Conclusion
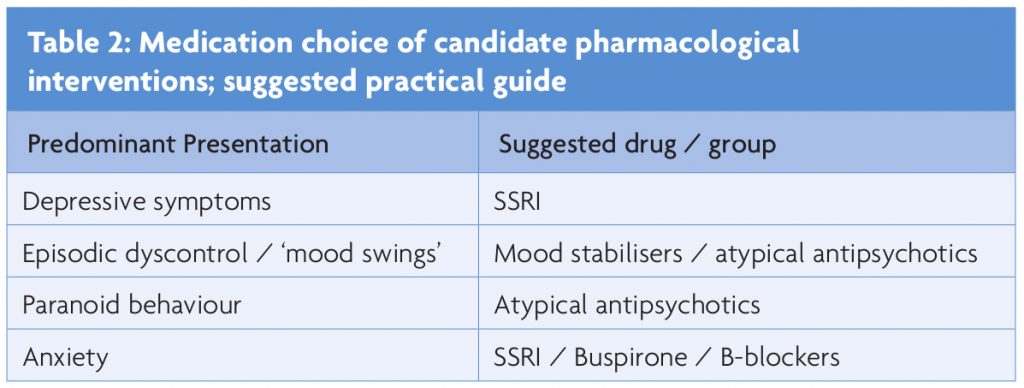
There are many challenges in assessing and managing chronic aggression due to its complex aetiology. Previous literature presents a selection of pharmacological options however, their effect on TBI patients has not been confirmed resulting in limited guidance. The heterogeneity between samples also renders it impossible to predict treatment outcomes in the TBI population warranting the need for low doses, slow titration and frequent monitoring.13 A six-week trial period is advised by Fleminger et al (2006) to ascertain effects of treatment before trialling a new medication.4 Patient and family education regarding realistic treatment outcomes and side effects of treatments is also necessary to ensure treatment compliance.2 In future, a clarification of the underlying neurochemical changes is needed to identify further treatment targets. Additional larger scale RCTs are also needed to guide decision making and predict treatment outcomes. Table 2 offers a practical guide on medication choice in relation to aggressive behaviour in ABI.
References
- Tateno A, Jorge RE, Robinson RG. Clinical correlates of aggressive behaviour after traumatic brain injury. J Neuropsychiatry Clin Neurosci. 2003;15(2):155-60.
- Kim E. Agitation, aggression and disinhibition syndromes after traumatic brain injury. NeuroRehabilitation 2002;17:297-310.
- Lombard LA, Zafonte RD. Agitation after traumatic brain injury: considerations and treatment options. Am J Phys Med Rehabil. 2005;84(10):797-812.
- Fleminger S, Greenwood RJ, Oliver DL. Pharmacological management for agitation and aggression in people with acquired brain injury. Cochrane Database Syst Rev. 2006;18(4):CD003299.
- Alderman N, Knight C, Brooks J. Rehabilitation Approaches to the Management of Aggressive Behaviour Disorders after Acquired Brain Injury. Brain Impairment. 2013;14(1):5-20.
- Siever LJ. Neurobiology of Aggression and Violence. Am J Psychiatry. 2008;165(4):429-42.
- McAllister TW. Neurobehavioral sequelae of traumatic brain injury: evaluation and management. World Psychiatry. 2008;7(1):3-10.
- Schwarzbold M, Diaz A, Martins ET, Rufino A, Amante LN, Thais ME et al. Psychiatric disorders and traumatic brain injury. Neuropsychiatr Dis Treat. 2008;4(4):797-816.
- Coccaro EF, Siever LJ. Pathophysiology and treatment of aggression. In: Davis KL, Charney D, Coyle JT, Nemeroff C, editors. Neuropsychopharmacology: The Fifth Generation of Progress. 5th ed. Pennsylvania: Lipincott, Williams & Wilkins; 2002:1709-23.
- Scottish Intercollegiate Guidelines Network. Brain injury rehabilitation in adults. Edinburgh: SIGN; 2013. 68 p. Report no.:130.
- Luauté J, Plantier D, Wiart L, Tell L, the SOFMER group. Care management of the agitation or aggressiveness crisis in patients with TBI. Systematic review of the literature and practice recommendations. Ann Phys Rehabil Med 2016;59(1):58-67.
- Warden DL, Gordon B, McAllister TW, Silver JM, Barth JT, Bruns J, et al. Guidelines for the Pharmacological Treatment of Neurobehavioral Sequelae of Traumatic Brain Injury. J Neurotrauma 2006;23(10):1468-501.
- Levy M, Berson A, Cook T, Bollegala N, Seto E, Tursanski S, et al. Treatment of agitation following traumatic brain injury: A review of the literature. NeuroRehabilitation 2005;20(4):279-306.
- Chew E, Zafonte RD. Pharmacological management of neurobehavioral disorders following traumatic brain injury – a state-of-the-art review. J Rehabil Res Dev 2009;46(6):851-79.

