Spasticity is defined as a motor disorder with failure to inhibit velocity-sensitive stretch reflexes leading to exaggerated muscle resistance. It is a cardinal feature of upper motor neuron lesions and can affect patients with congenital and acquired brain and spinal cord injuries of variable aetiologies (traumatic, vascular, neoplastic, and demyelination).
The exact incidence and prevalence of spasticity are unknown. A consensus of experts in Britain believes it to be about 20% of stroke patients and 75% of patients with severe brain injury [1]. Spasticity varies in severity from muscle stiffness to severe, painful, and uncontrollable muscle spasms. Spasticity can be general, involving multiple limbs and trunk muscles, regional, affecting a group of muscles in one or more limbs, or focal, affecting a single muscle.
Spasticity can affect the ability to feed and dress oneself, bladder and bowel control, hygiene, and mobility. It also predisposes to complications such as pressure sore formation due to poor seating / laying posture and contracture.
General principles of spasticity management
Spasticity management is an interdisciplinary team approach that requires a thorough assessment of the individual to exclude factors that would trigger spasticity, for example; infection, painful stimuli, poor posture, and constipation. Formulating a management plan aims to address those factors that would contribute to and are influenced by the increased muscle tone. The medical treatment of spasticity should be tailored to the individual as part of the interdisciplinary plan of management, with clearly identified goals. The choice of treatment would depend on the set goals and on the distribution of the involved muscles [2]. It can range from the following:
- Systemic oral muscle relaxants work directly on the CNS or the skeletal muscle receptors for generalised spasticity e.g. Baclofen, Tizanidine, Dantrolene
- Intrathecal administration of muscle relaxants achieves selective spinal inhibition of the stretch reflex for lower limb spasticity. This can be administered via an electronic or pneumatic pump e.g. Baclofen, clonidine or morphine
- Blocking the acetyl-choline re-uptake at the neuromuscular junction using Botulinum toxins
- Motor outflow block using chemical neurolysis at the peripheral nerve for regional spasticity e.g. phenol
The latter is a method reserved for selected individuals with progressive or stable neurology in whom spasticity involves large muscle groups affecting the lower limbs. The use of Phenol in upper limb spasticity or as a motor point block will not be discussed in this article.
Phenol nerve block
Mechanism of action:
Phenol (carbolic acid) in concentrations of more than 3% acts as a neurolytic agent [3]. This can be used to manage spasticity by impairing the spastic muscle innervations. Phenol also has a local anaesthetic property, which explains the transient muscle relaxation within the hour following phenol block. However, the desired neurolytic effect usually starts five to seven days following a motor nerve block [4].
Available preparations and recommended dosage:
Phenol in water is the recommended preparation for peri-neural block and is available in 5, 6 or 7% concentrations [3]. There are no clear studies about the recommended dose but the consensus from the literature recommends no more than 1200mg in total (e.g. 20mls of 6% concentration). The available data, from industrial toxicity with phenol show side effects if systemic absorption in adults is of 100mg/kg or more [5].
Indications:
Phenol is reserved for regional lower limb spasticity involving large muscles for which treatment with botulinum injections will not be appropriate due to the need for high doses of botulinum [6]. The following scenarios are examples of the use of phenol nerve block.
An individual diagnosed with a chronic neurological disorder (e.g. multiple sclerosis) with bilateral adductor and or hamstring spasticity. This spasticity pattern can lead to difficulties in achieving seating posture and maintaining personal care and hygiene (e.g. perineal access for dressing and washing) Detailed assessment is important to establish that the residual muscle and joint contractures will not be significant enough to prevent seating or personal care.
In the above example, phenol nerve block can be used on the obturator nerve to address hip adductor spasticity or on the sciatic nerve to address hamstring spasticity. The sciatic nerve is a mixed sensory-motor nerve and therefore it is preferable to do selective block to the hamstring branches to avoid nerve causalgia post-injection.
Similarly, a femoral nerve block can be used for the management of quadriceps muscle spasticity. This pattern of spasticity can be a hindrance for wheelchair users as accommodating knee extension on a wheelchair increases the turning circle and impairs chair manoeuvrability.
A tibial nerve block can be used in the management of equinovarus posture due to soleus, tibialis posterior and / or tibialis anterior muscles. The diagnostic local anaesthetic block may be required to assess the effect of the tibial nerve block if the individual is able to stand or step.
Technique
The most common nerve blocks done for the above-mentioned indications are the obturator nerve, hamstring branches of the sciatic nerve, femoral nerve, and tibial nerve. The nerves can be located using various techniques including ultrasound scanning, X-ray, or guided electrical stimulation. The electric stimulation technique relies on a Teflon-coated needle as the negative electrode with a pulsating electric current of 1-2mA at 2Hz.
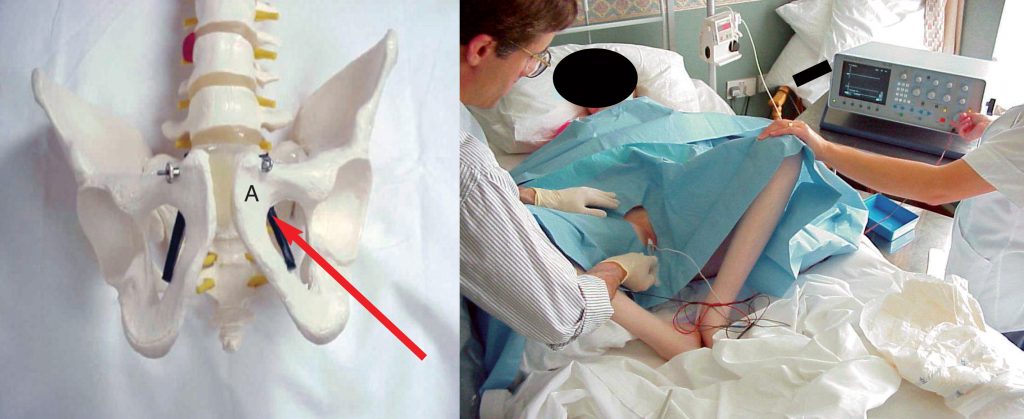
Obturator nerve [7]: (Figure 1)
The obturator nerve emerges from the obturator hiatus at the obturator internus muscles at the superior medial aspect of the obturator foramen. It divides into two branches. The anterior branch supplies the adductor longus, brevis and the gracilis muscles. The posterior branch supplies the obturator externus and the adductor magnus muscles. The posterior aspect of the adductor magnus also receives innervations from the sciatic nerve.
The obturator nerve block is achieved by introducing the needle at 45° to the anterior aspect of the thigh aimed at a point 1-2cm below and lateral to the pubic tubercle. As the needle is introduced, it should hit the superior pubic ramus, the needle is then withdrawn and reintroduced at 60° to enter the obturator foramen at its superior-medial aspect. The nerve can be located using electric stimulation guidance. Patients with associated hip adduction and flexion posture usually have associated pelvic tilt and locating the obturator foramen as above may be difficult. Another method is to follow the adductor longus tendon and insert the needle lateral to its pelvic insertion under electric stimulation guidance. The nerve is then infiltrated with 200-300mg of phenol.
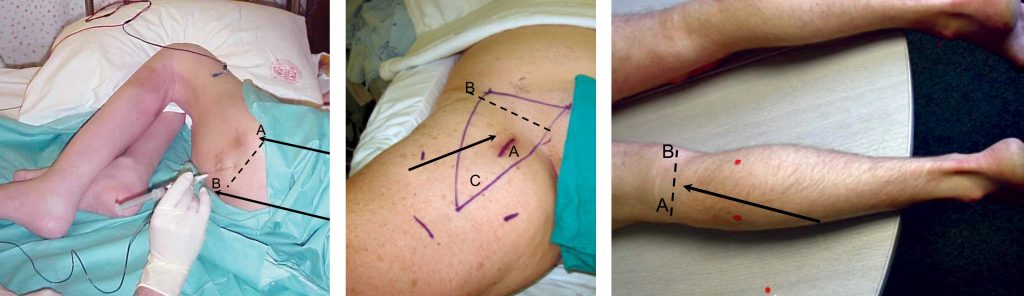
Hamstring branches of the sciatic nerve: (Figure 2)
Selective motor block to the hamstring branches is favourable in spasticity management to minimise the risk of nerve causalgia. The motor innervations of the hamstrings can be located at the mid-point of the line between the greater trochanter and the ischeal tuberosity. Locating the branches to the biceps femoris, semi-tendinosus and semi-membranosus muscles is feasible using electric stimulation technique by noticing the rhythmic contractions of the corresponding muscles. 300-500mg of phenol can be split between the branches according to the severity of muscle spasticity. There are reported anatomical variations, therefore some clinicians may use surface electrodes or USS guided techniques to localise the motor branches prior to introducing the needle.8 Injection of phenol should be avoided if there are noticeable contractions of the foot, as this would involve the sensory component of the sciatic nerve via the tibial and common peroneal nerves.
Femoral nerve: (Figure 3)
The nerve can be easily located lateral to the palpable pulse of the femoral artery below the inguinal ligament. A teflon coated needle is introduced at 90° with electric stimulation. The nerve can be found at 2-3cm depth with associated quadriceps contractions on stimulation. 100-300mg of phenol can be infiltrated according to the response. Aspiration before the injection is an essential practice that cannot be over-emphasised, in particular, to avoid accidental injection into the femoral artery.
Tibial nerve: (Figure 4)
The nerve can be easily located about 0.5 to 1cm below the mid-point of the popliteal crease between the medial and lateral femoral condyles. This is to avoid including the sural nerve, which usually branches at a proximal level, and thus avoids sensory causalgia. The needle is introduced with stimulation and the nerve can be found at a depth of 2-3cm and superficial to the popliteal vessels. Calf muscle contractions and foot inversion is noticed once the nerve is stimulated. 100-200mg of phenol can be used to achieve a satisfactory block to the tibial nerve at this level. To minimise the possibility of nerve causalgia, ensure the patient reports no sensory symptoms at the time of the stimulation. If so, the nerve needs to be approached at a slightly distal level after the branching of the sural nerve.
Side effects
Common
- Occasional redness, discomfort or bruises at the injection site
Rare side effects
- Skin infection or abscess formation
- Haematoma
- Muscle / soft tissue fibrosis
- Nerve causalgia (in sensory-motor nerve blocks)
Very rare side effects
- Vascular injury
- Injury to pelvic organs (applicable to
- obturator nerve block)
- Systemic effects: arrhythmia, pulmonary fibrosis, confusion and renal impairment
Summary
Phenol nerve block is a treatment option in individuals with regional spasticity of the lower limbs. It can be used in cases with poor tolerability to systemic muscle relaxants and if large muscle groups that would exceed the safe dose of botulinum toxins.
References
- Barnes M. Medical management of spasticity in stroke. Journal of Age and Ageing. 2001;30:13-16. https://doi.org/10.1093/ageing/30.suppl_1.13
- Ward A. Summary of spasticity management – Treatment algorithm. European Journal of Neurology 2002;9:48-52. https://doi.org/10.1046/j.1468-1331.2002.0090s1048.x
- Garland D, Lucie R, Waters R. Current uses of open phenol nerve block for adult acquired spasticity. Clinical Orthopaedics. 1982;165:217-22. https://doi.org/10.1097/00003086-198205000-00033
- Beard S, Hunn A, Wight J. Treatments for spasticity and pain in multiple sclerosis: a systematic review. Health Technology Assessment. 2003;7(40):61-4. https://doi.org/10.3310/hta7400
- Montizan G. IPCS Environmental Health Criteria for Phenol. WHO Publications 1994(161).
- Kocabas H, Salli A, Demir AH, Ozerbil OM. Comparison of phenol and alcohol neurolysis of tibial nerve motor branches to the gastrocnemius muscle for treatment of spastic foot after stroke: a randomized controlled pilot study. European Journal of Physical and Rehabilitation Medicine. 2010;46(1):5-10.
- Akkaya T, Unlu E, Alptekin A, Gumus H, Umay E, Cakci A. Neurolytic phenol blockade of the obturator nerve for severe adductor spasticity. Acta Anesthesiology Scandinavia. 2010;54:79-85. https://doi.org/10.1111/j.1399-6576.2009.02130.x
- Paola M, et Al. Precise Localization of the Motor Nerve Branches to the Hamstring Muscles: An Aid to Conduct Neurolytic Procedures. Archive of Physical Medicine and Rehabililation. 1996;77:1157-60. https://doi.org/10.1016/S0003-9993(96)90140-9
