Few neurologists will be unfamiliar with referral letters stating that the patient has “Rhomberg’s sign” or some “mild rhombergism” (capitalisation variable), a particularly irritating misnomer for the pedants among us. As Henry Higgins the fictional Professor of Phonetics [1] observed:
‘Does the same thing hold true in India, Pickering? Is there the peculiar habit of not only dropping a letter like the letter “h”, but using it where it doesn’t belong, like “hever” instead of “ever”?’ My Fair Lady – Act 1, Scene 5, p58 [1].
Or Rhomberg instead of Romberg!
So, who was “Rhomberg,” and what did he describe?
The Neurologist: a brief biography [2,3,4]
Of course, all neurologists know (or should know) that the eponymous clinician is in fact Romberg, specifically Moritz Heinrich Romberg (Figure 1A). Born in Saxony in 1795, he studied in Berlin and Vienna before pursuing his career in Berlin (at the Charité Universitätsmedizin) from 1820 until his retirement in 1867. He has been described as one of the founders of neurology, principally on account of his book, Lehrbuch der Nervenkrankheiten des Menschen, published between 1840 and 1846. This has been characterised as the first formal treatise on diseases of the nervous system, which aimed to link pathology and physiology systematically. Therein, Romberg gave one of the enduring accounts of tabes dorsalis and described the pupillary findings in tertiary syphilis (before the eponymous Argyll Robertson).
Elsewhere he gave a classic description of achondroplasia, and published on diverse medical and surgical topics, co-authoring papers with his nephew Eduard Heinrich Henoch (Figure 1B, C) [5].
Eponymous signs [4,6,7]
Romberg is surely best known for his sign, or signs: static, sharpened, psychogenic, and dynamic variants of Romberg’s sign have been described, although only the first of these originates with Romberg himself.
His particular contribution was to develop a clinically elicited neurological sign based on the observation that eye closure in patients with tabes dorsalis resulted in a tendency to sway and fall. Others had also observed this phenomenon before Romberg, such as Marshall Hall and Bernardus Brach, but not developed it for use as a sign.
Hence, Romberg’s sign, or Rombergism, is adjudged present (or positive) when there is a dramatic increase in unsteadiness, sometimes with falls, after eye closure when a patient is standing comfortably. This is sometimes known as the static Romberg’s test, in contrast to dynamic Romberg’s test (vide infra). Before asking the patient to close his or her eyes, it is necessary to position one’s arms in such a way as to be able to catch the patient should they begin to fall. Patients may fall forward immediately on eye closure (“sink sign”).
These phenomena result from sensory ataxia i.e. loss of proprioception from the feet, which occurs most commonly with posterior column spinal cord disease, not limited to patients with tabes dorsalis, in whom Romberg originally described his sign, but which may also occur in other forms of deafferentation.
There is no standardised method of “how to do it” (i.e. operationalisation of the sign), for example whether the feet should be positioned together or apart; whether the feet should be positioned heel to toe, so-called “sharpened Romberg’s sign” (narrowing the standing base); whether or not shoes should be worn; the duration of observation; and how much sway indicates a positive sign. Posturography is an attempt to quantify the Romberg test.
A modest increase in sway on closing the eyes may be seen in normal subjects, and in patients with cerebellar ataxia, frontal lobe ataxia, and vestibular disorders (toward the side of the involved ear); on occasion these too may produce an increase in sway sufficient to cause falls. Hence, Romberg’s test is not specific.
Large amplitude sway without falling, due to the patient clutching hold of furniture or the neurologist, has been labelled “psychogenic Romberg’s sign”, an indicator of functional stance impairment.
It has been argued that Romberg’s sign is neither highly sensitive nor specific (no dedicated test accuracy study has been reported to our knowledge) and, because of the risk of falling, should be abandoned in favour of testing proprioception at the big toe [8].
Heel-toe or tandem walking, walking along a straight line by putting one foot directly in front of the other, heel to toe, as on a tight-rope, is sometimes known as the “dynamic Romberg’s test”. Impairment in this test may be a consequence of ataxia of either cerebellar or sensory origin.
Pryse-Phillips also lists “Romberg’s spasm” as a form of masticatory spasm of unknown cause, probably dystonic [9].
Eponymous syndromes
Romberg’s name is recorded (second) in at least two syndromes, both somewhat esoteric.
Parry-Romberg syndrome is progressive hemifacial atrophy due to loss of subcutaneous tissues [10,11]. In addition to the cosmetic features, ipsilateral intracerebral abnormalities may also occur, producing neurological features such as migraine, facial pain, focal seizures, hemiparesis, hemianopia, and cognitive impairment. The condition was first described by the English physician Caleb Hillier Parry (1755-1822) in the posthumously published Collections from the unpublished medical writings of the late Caleb Hillier Parry MD FRS (1825; volume I, p.478-80). Romberg’s account appeared over 20 years later, in 1846.
The Howship-Romberg syndrome [12], or phenomenon (widely and incorrectly referred to as a sign [13,14]) is pain or paraesthesia in the hip or groin radiating along the antero-medial thigh to the knee provoked by extension, abduction and medial rotation of the lower limb (and thus an inability to adduct the thigh) due to irritation/compression of the obturator nerve by an obturator hernia. The association of small bowel obstruction and the Howship-Romberg phenomenon is recognised amongst general surgeons to be pathognomonic of an incarcerated obturator hernia [14]. The condition was originally described by the English surgeon John Howship (1781-1841), whilst working at St George’s Hospital (Lanesborough House, Hyde Park Corner, London), around 1840.
We suspect that few neurologists will have encountered either of these syndromes during their careers.
So why the confusion?
Why confuse “Romberg” with “Rhomberg”? The frequency of misspelling has been previously noted [8], and indeed it has been claimed that this is the most misspelled eponym in neurology [4]. We suggest some possible explanations.
Firstly, very simplistically: homophony. In neurology, terminology incorporating the word ‘rhombus’ (Figure 2) is more frequent. For example, the rhomboid muscles, major and minor, and the rhombencephalon (Figure 3) [15]. Moreover, the letter rho (ρ) is also used as both the mathematical symbol for density and to denote Spearman’s correlation coefficient.
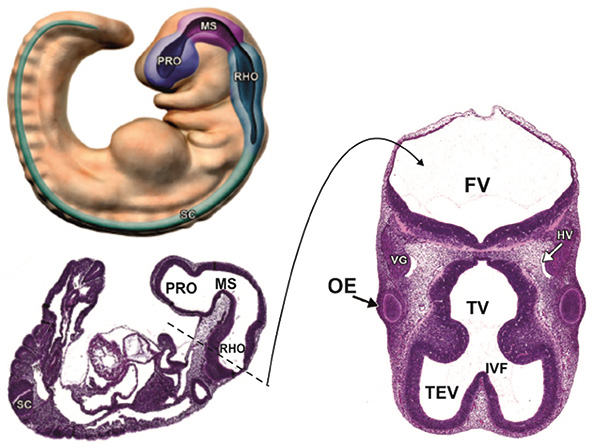
HV = head vein; IVF = interventricular foramen; MS = mesencephalon; OE optic eminence; PRO = prosencephalon; SC = spinal cord; TEV = telencephalic vesicle; TV = third ventricle; VG = trigeminal ganglion (adapted from Figures 3 and 11 of Chen et al., 2017) [15].
Secondly, and probably related to the first point: familiarity. Whilst we do not suggest that rhombus is a high frequency word, Romberg is certainly lower frequency. Whereas Romberg is unlikely to be encountered prior to medical school or even, possibly, neurological training, the rhombus is a staple of even primary school geometry. Hence the latter is more familiar and this might account for the substitution. The hint of the esoteric or mathematical might link to the general unfamiliarity (or unwillingness to become familiar) with matters neurological.
Thirdly, and related to the previous point: as a medical community we have become increasingly ignorant of our history, collectively consigning many of the great Neurologists of the past, including Professor Moritz Heinrich Romberg, to obscurity. Although, as shown by the preceding brief biography, a case can be made for including him in the neurological pantheon, he is not well known, or well-served by eponymous association, even though his textbook was translated into English in 1853 by Edward Sieveking, a physician at Queen Square. Sadly, his German origin might also account for his obscurity in the Anglophone world, wherein ignorance of other languages approaches the normative (and may also account for such lapses as “L’hermitte” for “Lhermitte”, and hence to references to “the hermit’s sign” [16]).
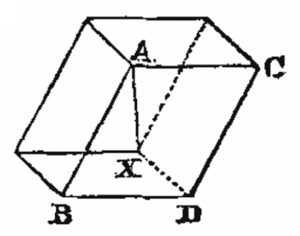
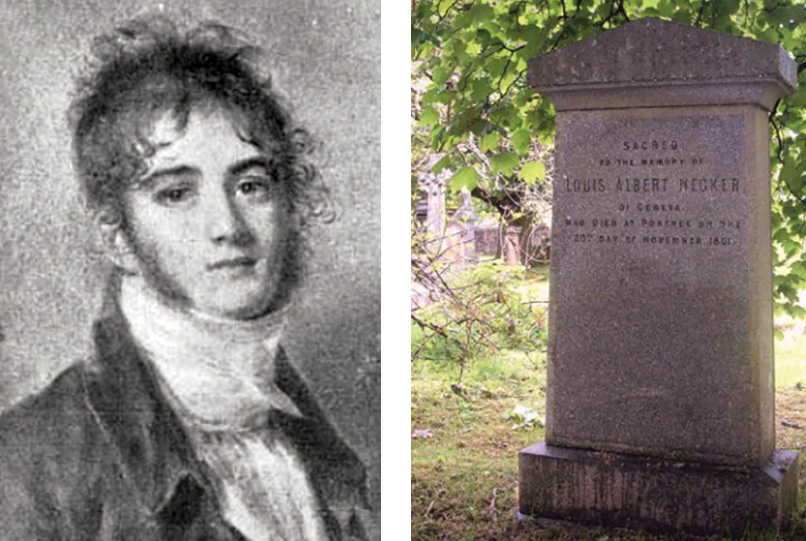
For those sorry to lose “Rhomberg” from the neurological lexicon, we offer some possible consolation. Necker’s cube, the optical illusion, drawing or copying of which features in certain cognitive screening instruments (e.g. the various iterations of the Addenbrooke’s Cognitive Examination), was in fact a rhombohedron, or what is more commonly termed a rhomboid, rather than a cube (Figure 4A) [17] in the original publication of 1832 by Louis Albert Necker (1786-1861; Figure 4B & 4C) [18,19]. As cube is to rhomboid as square is to rhombus, perhaps we should (more correctly) rename this “Necker’s rhomboid”.
References
- Lerner AJ, Loewe F. My Fair Lady – A Musical Play in Two Acts Based on Pygmalion by Bernard Shaw. Published by Signet Books, The New American Library of World Literature, Inc. 501 Madison Avenue, New York 1958
- Schiffter R. Moritz Heinrich Romberg (1795-1873). J Neurol 2010;257:1409-10. https://doi.org/10.1007/s00415-010-5552-1
- Housman B, Bellary SS, Walters A, Mirzayan N, Tubbs RS, Loukas M. Moritz Heinrich Romberg (1795-1873): early founder of neurology. Clin Anat. 2014;27:147-9. ttps://doi.org/10.1002/ca.22112
- Pearce JM. Romberg and his sign. Eur Neurol 2005;53:210-3. https://doi.org/10.1159/000086732
- Romberg MH, Henoch EH. Affection of the Heart, Thyroid Gland, and Eyeballs. Edinb Med Surg J. 1854;81:423-7.
- Lanska DJ, Goetz CG. Romberg’s sign: development, adoption, and adaptation in the 19th century. Neurology 2000;55:1201-6. https://doi.org/10.1212/WNL.55.8.1201
- Larner AJ. A dictionary of neurological signs (4th edition). London: Springer; 2016:287. https://doi.org/10.1007/978-3-319-29821-4
- Turner MR. Romberg’s test no longer stands up. Pract Neurol. 2016;16:316. https://doi.org/10.1136/practneurol-2016-001365
- Pryse-Phillips W. Companion to clinical neurology (2nd edition). Oxford: Oxford University Press; 2003:832.
- Larner AJ, Bennison DP. Some observations on the aetiology of progressive hemifacial atrophy (“Parry-Romberg syndrome”). J Neurol Neurosurg Psychiatry 1993;56:1035-6. https://doi.org/10.1136/jnnp.56.9.1035-a
- Stone J. Parry-Romberg syndrome. Pract Neurol. 2006;6:185-8. https://doi.org/10.1136/jnnp.2006.089037
- Schopf (Wien. Klin. Woch., No. 8, 1903). Obturator Hernia: Tube and Ovary in Sac. BMJ 1903;2(2233):E58-9.
- Temple DF, Miller RE. Incarcerated obturator hernia: two case reports and review of the literature. J Natl Med Assoc. 1980;72:513-5.
- Saeed R, Ahmed M, Lara G, Mahmoud A, Nurick H. Howship-Romberg sign and bowel obstruction: a case report. Cureus 2019;1:e5066. https://doi.org/10.7759/cureus.5066
- Chen VS, Morrison JP, Southwell MF, Foley JF, Bolon B, Elmore SA. Histology atlas of the developing prenatal and postnatal mouse central nervous system, with emphasis on prenatal days E7.5 to E18.5. Toxicol Pathol. 2017;45:705-44. https://doi.org/10.1177/0192623317728134
- Williams TL, Bates D, Baker MR. The phenomenon of Lhermitte. Pract Neurol. 2021;21:246-8. https://doi.org/10.1136/practneurol-2020-002918
- Necker LA. Observations on some remarkable optical phaenomena [sic] seen in Switzerland; and on an optical phaenomenon [sic] which occurs on viewing a figure of a crystal or geometrical solid. London and Edinburgh Philosophical Magazine and Journal of Science, third series 1832;1:329-37. https://doi.org/10.1080/14786443208647909
- Eyles VA. Louis Necker of Geneva and his geological map of Scotland. Transactions of the Edinburgh Geological Society. 1948;14:93-27.https://doi.org/10.1144/transed.14.2.93
- Wade NJ, Campbell RN, Ross HE, Lingelbach B. Necker in Scotch perspective. Perception. 2010;39:1-4. https://doi.org/10.1068/


