Abstract
Polyneuropathies encompass a number of diseases of the peripheral nerves. Causes vary, and some types of polyneuropathy have a chronic disease course, and some have acute onset. Polyneuropathies, such as Guillain Barré Syndrome, improve after acute deterioration, but some people are left with longer term disability.
Physical management to manage longer term impairments and maintain function, are gathering evidence of efficacy, though trials remain small in number and size. Exercise trials show some positive improvements in proximal muscle strength, aerobic capacity, balance and distal strength in children. People with polyneuropathy often present with distal weakness and joint malalignment. Orthotics interventions may address these impairments and can vary from ankle foot orthoses to insoles. Weakness and sensory impairment also lead to altered hand function which can be addressed by adaptive strategies and exercise. People with polyneuropathies can beneft from rehabilitation interventions through addressing the impact of impairments and compensatory strategies necessary for optimised function.
Key take home messages:
- Aerobic exercise and resistance training of less affected muscles show moderate effect in people with polyneuropathy
- Resistance training for more affected muscles may show improvement if the muscle scores above 4/5 MRC score at baseline. More trials are required
- Orthotics can be used to treat a range of gait deviations for people with polyneuropathy.
- A thorough assessment and identifcation of patient goals are key to a successful orthotic prescription
- Early education is essential in providing strategies aiming to maintain hand function for people with polyneuropathy
- Consider splinting to support grip patterns for people with neuropathy with mild to moderate impairment
Introduction
Polyneuropathies are common neurological disorders affecting the peripheral nerves. There are a number of causes of damage to these structures, and they can be categorised as inherited: e.g. Charcot-Marie-Tooth disease (CMT); or acquired: e.g. diabetic or inflammatory neuropathies. Motor and sensory impairments are commonly encountered in these conditions leading to altered balance, gait and upper limb function.1 Inherited neuropathies tend to come on earlier in life and are slower progressing. Acquired neuropathies have a more variable rate of onset and disease course. Many polyneuropathies tend to affect the distal sensorimotor functions first, but inflammatory neuropathies can be patchy with earlier proximal involvement. Common impairments are primary muscle weakness and wasting due to denervation, and impairments of proprioception and nociception. Deformities of the feet are associated with early onset of disease due to muscle imbalance and soft tissue shortening.2 Altered hand posture and grip is also observed with greater weakness of intrinsic muscles.3 Rehabilitation interventions aim to optimise function, support weakness and accommodate deformity. Acute onset polyneuropathies, e.g. Guillain Barré syndrome, are often managed through the recovery phase with multi-disciplinary rehabilitation.4 There is evidence of good functional improvement and intensity of early intervention appears to be important to people with the disease.5,6 Not all people with GBS make a full recovery and some are left with long term disability. Other types of polyneuropathy are long term conditions. A vital component in maximising function and participation in people with chronic polyneuropathies is targeting rehabilitation interventions in an effective and timely manner. Although pathways of optimal physical management are not yet available, combinations of rehabilitative and management approaches are gathering evidence, specifcally in exercise, orthotics and adaptive upper limb strategies.
Exercise in polyneuropathy
Exercise training to improve function for people with polyneuropathy falls into three main areas: aerobic training, general strength training and specifc proprioceptive training. The overall evidence for the effcacy of exercise is limited, as demonstrated by systematic reviews,7,8,9 but it is an expanding area of research focus. In diabetic neuropathy, intensive aerobic exercise may regenerate intra-epidermal nerve fibre density in pre-diabetic metabolic syndrome, and walking activities can slow the progression of diabetic neuropathy.10 There are fewer studies in other rarer polyneuropathies, but cycle ergometry has been shown to improve cardiorespiratory fitness and fatigue in CMT.11 There is more robust evidence for proximal muscle strength training in polyneuropathy with improved strength and function with structured programmes.7,8 Most trials target the less affected muscles groups. A more recent study of distal strengthening in children with CMT showed sustained improvements over two years compared to controls who declined over the same period, as expected with the natural history of the disease.12 This suggests that earlier interventions may impact disease progression, but this is yet to be explored in adults or in people with more severe weakness. Specific balance training interventions have been explored in polyneuropathies, often as a combination of multi-sensory and proprioceptive exercises plus strength training. In diabetic neuropathy there is evidence of efficacy with this more standard type of rehabilitation, but also novel methods such as perturbation platforms, dynamic target tasks and dynamic movement control with activities such as Tai Chi.13 In the rarer neuropathies the evidence is more sparse, but positive effects have been seen with multi-modal training in sensory neuropathy14 and CMT.15
Orthotic interventions
Patients with polyneuropathy who are referred to an orthotics clinic can present with symptoms including weakness, malalignment of the joints, reduced balance or pain. These symptoms can lead to gait abnormalities and people with neuropathy often benefit from orthotic interventions. The International Organization for Standardization [Prosthetics and orthotics]16 defines an orthoses as ‘an externally applied device used to modify the structural and functional characteristics of the neuromuscular and skeletal system’. Ankle dorsifexion weakness will lead to ‘foot drop’ and an increased risk of trips and falls. Plantarfexion weakness will result in reduced propulsion during gait. Both will lead to compensatory movement patterns and an inefficient gait. Patients with CMT 1A have been found to have a higher energy cost of walking than healthy individuals even if they have very mild impairment.17
Orthotic prescription will be determined by a discussion with the patient and an assessment of gait kinetics, manual muscle testing and joint range of motion. Patient goals should be set and orthotic prescription agreed with the patient. Orthotic prescription may be influenced by patient preference to the detriment of gait biomechanics due to factors such as cosmesis, environment and footwear. Ankle foot orthoses (AFO’s) are commonly used for polyneuropathy patients with distal weakness. These can be custom made or off the shelf, and are usually made from either thermoplastic or carbon fibre. The style and rigidity of the device will be determined and must be considered carefully for the best outcome.
The optimum stiffness of AFO is related to factors such as muscle weakness, ankle joint range of motion and body weight.18 Increased AFO stiffness reduces ankle movement during walking. Stiffer AFOs limit peak knee extension and increase knee flexion, there is low evidence for its effects on hip or pelvis kinematics and kinetics.19 Due to ability to return energy for propulsion, carbon fibre AFOs may increase walking speed and plantarfexor power compared to a thermoplastic AFO.20 Some patients may also identify their walking problem as due to knee instability. This may be due to the knee giving way or related to hyperextension, which can cause pain. There is a lack of evidence on orthotics for the management of knee instability related to neuromuscular disorders on pain and falls21 but control of knee alignment through use of rigid AFOs or through knee braces can be successful.
Patients with polyneuropathy commonly present with changes to the alignment of joints, which can lead to pain, instability or callous build ups under the feet. Custom insoles are an effective treatment of cavus foot pain and its associated limitation in function by reducing and redistributing abnormal ground reaction forces.22
Management of hand weakness
Intrinsic muscles of the hand, dexterity, grip strength and sensory function are most commonly affected in polyneuropathies. These are key components of hand function.23,24,25 These studies report that activities which require finger grips such as pulp pinch and lateral pinch are the most limited. Often compensatory movement patterns develop as the level of impairment increases.23,26 Despite the prevalence of hand dysfunction there is limited evidence base for upper limb rehabilitation in neuropathy. For upper limb orthotics Videler and colleagues concluded that a thumb opposition splint can be effective in improving upper limb functioning in their pilot study.27 Opinion papers recommend adaptive equipment to compensate for hand deformities, sensory loss, and weakness and intervention should aim to preserve or enhance manual dexterity.28
Recent guidelines published by the Charcot Marie Tooth Association (2018)29 recommend the following interventions: 1. Resistance training for the hand and wrist muscles 2. Activities that engage hands in coordination, fne-motor and manipulation 3. Splinting to support hand function and/or to provide a stretch to prevent contractures 4. Stretching to prevent soft tissue shortening 5. Adaptive equipment when remedial options are no longer indicated.
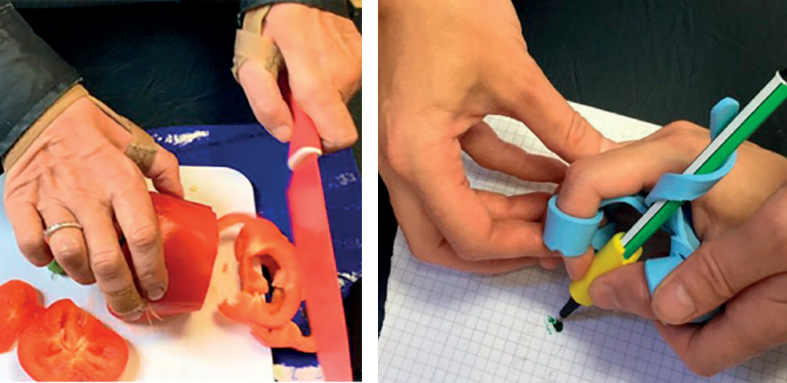
In the early stages of diagnosis, encouraging normal grip patterns aims to delay overreliance on the stronger extrinsic muscles and encourage the use of the intrinsic muscles within activities. With mild weakness education alone can be effective in promoting precision grips. Where education is not adequate, functional splints are frequently used. Thumb spica splints can improve palmar abduction to facilitate pinch grip.27,29
Figure-of-eight splints provide stability at the proximal interphalangeal joint for pure pinch and finger push grips.
Metacarpophalangeal joint block splints prevent hyperextension and can promote active interphalangeal extension during tasks such as typing. Custom made functional splints support more complex grip patterns such as a tripod grip for handwriting. Acceptance should be considered when prescribing splints to ensure they are effective. Functional splints can hinder function if prescribed at the later stages due to established compensatory movement patterns which they are reliant on for function. Experience in other neuromuscular diseases has demonstrated splints are less successful with severe muscle wasting.30
Splints are used for the prevention of contractures29 and maintenance of skin integrity. Patients may find resting splints heavy and bulky and therefore customised lightweight resting splints which target the joints at risk may promote compliance.
Task adaptation and equipment is another key component to promote hand function.
This approach is useful for more severe weakness for maintenance of independence. Task adaptation is also beneficial in the early stages to help facilitate normal grip patterns and improve efficiency to limit the impact of muscle fatigue and altered sensation.
Summary
People with polyneuropathies can beneft from rehabilitation interventions to improve, maintain or support function. Understanding the impact of impairments and compensatory strategies necessary for function enables clinical reasoning and optimised outcomes.
References
- England JD, Asbury AK. Peripheral Neuropathy. Lancet. 2004;363(9427):2151–61. https://doi.org/10.1016/S0140-6736(04)16508-2.
- Burns J, Ryan MJ, Ouvrier RA. Evolution of Foot and Ankle Manifestations in Children with CMT1A. Muscle & Nerve. 2009;39(2):158–66. https://doi.org/10.1002/mus.21140.
- Videler AJ, Beelen A, Nollet F. Manual Dexterity and Related Functional Limitations in Hereditary Motor and Sensory Neuropathy. An Explorative Study. Disability and Rehabilitation. 2008;30(8):634-38. https://doi.org/10.1080/09638280701400755.
- Khan F, Amatya B. Rehabilitation interventions in patients with acute demyelinating infammatory polyneuropathy: a systematic review. Eur. J. Phys. Rehabil. Med. 2012;48:507–522.
- Davidson I, Wilson C, Walton T., Brissenden S. 2009. Physiotherapy and Guillain-Barré syndrome: results of a national survey. Physiotherapy 2009;95:157-163. https://doi. org/10.1016/j.physio.2009.04.001
- Novak P, Šmid S, Vidmar G. Rehabilitation of Guillain-Barré syndrome patients: an observational study. Int. J. Rehabil. Res. Int. Z. Rehabil. Rev. Int. Rech. Readaptation. 2017. https://doi.org/10.1097/MRR.0000000000000225
- White CM, Pritchard J, Turner-Stokes L. 2004. Exercise for People with Peripheral Neuropathy. Edited by The Cochrane Collaboration and Claire Margaret White. Cochrane Database of Systematic Reviews. October. 2004.
- Sman AD, Hackett D, Fiatarone Singh M, Fornusek C, Manoj P. Menezes P, Burns J. 2015. Systematic Review of Exercise for Charcot-Marie-Tooth Disease. Journal of the Peripheral Nervous System. JPNS. May. https://doi.org/10.1111/jns.12116.
- Simatos Arsenault N, Vincent PO, Yu BH, Bastien R, Sweeney A. Infuence of Exercise on Patients with Guillain-Barré Syndrome: A Systematic Review. Physiotherapy Canada. Physiotherapie Canada. 2016;68 (4):367–76. https://doi.org/10.3138/ptc.2015-58.
- Singleton J, Robinson A, Smith G, Marcus RL. Exercise as Therapy for Diabetic and Prediabetic Neuropathy. Current Diabetes Reports 2015;15 (12): 120. https://doi. org/10.1007/s11892-015-0682-6.
- Wallace A, Pietrusz A, Dewar E, Dudziec M, Jones K, Hennis P, Sterr A, et al. Community Exercise Is Feasible for Neuromuscular Diseases and Can Improve Aerobic Capacity. Neurology. 2019;92(15): e1773–85. https://doi.org/10.1212/WNL.0000000000007265.
- Burns J, Sman AD, Cornett KMD, Wojciechowski E, WalkerT, MenezesMP, Mandarakas MR, et al. Safety and Effcacy of Progressive Resistance Exercise for Charcot-Marie-Tooth Disease in Children: A Randomised, Double-Blind, Sham-Controlled Trial. The Lancet. Child & Adolescent Health 1 2017;(2): 106–13. https://doi.org/10.1016/S2352- 4642(17)30013-5.
- Chapman A, Meyer C, Renehan E, Hill KD, Browning CJ. Exercise Interventions for the Improvement of Falls-Related Outcomes among Older Adults with Diabetes Mellitus: A Systematic Review and Meta-Analyses. Journal of Diabetes and Its Complications. 2017;31(3):631–45. https://doi.org/10.1016/j.jdiacomp.2016.09.015.
- Missaoui B, Thoumie P. Balance Training in Ataxic Neuropathies. Effects on Balance and Gait Parameters. Gait & Posture 2013;38(3):471–76. https://doi.org/10.1016/j.gaitpost.2013.01.017.
- Dudziec M, Lee LE, Massey C, Skorupinska M, Laura M, Reilly MM, Ramdharry GM. Preliminary Falls and Functional Balance Data from the BALTiC Study: A Feasibility Analysis of Home Based BALance Training in People with Charcot-Marie-Tooth Disease. Journal of Neuromuscular Diseases 6 (Supplement 1): S44. 2019.
- International Organization for Standardization. 1989. Prosthetics and orthotics — Vocabulary — Part 1: General terms for external limb prostheses and external orthoses. ISO 8549-1:1989 https://www.iso.org/obp/ui/#iso:std:15800:en
- Menotti F, Felici F, Damiani A, Mangiola F, Vannicelli R, Macaluso A. Charcot-Marie-Tooth 1A Patients with Low Level of Impairment Have a Higher Energy Cost of Walking than Healthy Individuals. Neuromuscular Disorders. 2011;21 (1): 52–57. https://doi.org/10.1016/j. nmd.2010.09.008.
- Waterval NFJ, Nollet F, Harlaar J, et al. Precision orthotics: optimising ankle foot orthoses to improve gait in patients with neuromuscular diseases; protocol of the PROOF-AFO study, a prospective intervention study. BMJ Open 2017;7:e013342. doi: 10.1136/bmjopen-2016- 013342.
- Totah D, Menon M, Jones-Hershinow C, Barton K, Gates DH. The impact of ankle-foot orthosis stiffness on gait: A systematic literature review. Gait Posture. 2019 Mar;69:101-111. doi: 10.1016/j.gaitpost.2019.01.020.
- Zou D, Tao H, Dailey M, Smith KE, Silva MJ, Sinacore DR, Mueller MJ, Hasting MKs. Experimental and Computational Analysis of Composite Ankle-Foot Orthosis. Journal of Rehabilitation Research and Development. 2014;51(10):1525–36. https://doi.org/10.1682/ JRRD.2014-02-0046.
- McDaid C, Fayter D, Booth A, O’Connor J, Rodriguez-Lopez R, McCaughan D, Bowers R, et al. 2017. Systematic Review of the Evidence on Orthotic Devices for the Management of Knee Instability Related to Neuromuscular and Central Nervous System Disorders. BMJ Open 2017;7 (9): e015927. https://doi.org/10.1136/bmjopen-2017-015927.
- Burns J, Crosbie J, Ouvrier R, Hunt A. Effective Orthotic Therapy for the Painful Cavus Foot: A Randomized Controlled Trial. Journal of the American Podiatric Medical Association. 2006;96(3): 205–11.
- Eklund E, Svensson E, Häger-Ross C. Hand Function and Disability of the Arm, Shoulder and Hand in Charcot-Marie-Tooth Disease. Disability and Rehabilitation. 200931 (23): 1955–62. https://doi.org/10.1080/09638280902874170.
- Videler AJ, Beelen A, van Schaik IN, Verhamme C, van den Berg LH, de Visser M, Nollet F. Tripod Pinch Strength and Thumb Opposition Are the Major Determinants of Manual Dexterity in Charcot-Marie-Tooth Disease Type 1A. Journal of Neurology, Neurosurgery, and Psychiatry. 2010;81(8):828–33. https://doi.org/10.1136/jnnp.2009.187302.
- Videler AJ, Beelen A, van Schaik IN, de Visser M, Nollet F. Manual Dexterity in Hereditary Motor and Sensory Neuropathy Type 1a: Severity of Limitations and Feasibility and Reliability of Two Assessment Instruments. Journal of Rehabilitation Medicine: Official Journal of the UEMS European Board of Physical and Rehabilitation Medicine. 2008;40(2):132–36. https://doi.org/10.2340/16501977-0143.
- Svensson E, Häger-Ross C. Hand Function in Charcot Marie Tooth: Test Retest Reliability of Some Measurements. Clinical Rehabilitation. 2006;20(10):896–908. https://doi. org/10.1177/0269215506072184.
- Videler A, Eijffnger E, Nollet F, Beelen A. A Thumb Opposition Splint to Improve Manual Dexterity and Upper-Limb Functioning in Charcot-Marie-Tooth Disease. Journal of Rehabilitation Medicine: Offcial Journal of the UEMS European Board of Physical and Rehabilitation Medicine. 2012;44(3):249–253. https://doi.org/10.2340/16501977-0932.
- Videler A J, Beelen A, van Schaik AN, Verhamme C, van den Berg LH, de Visser M, Nollet F. Tripod Pinch Strength and Thumb Opposition Are the Major Determinants of Manual Dexterity in Charcot-Marie-Tooth Disease Type 1A. Journal of Neurology, Neurosurgery, and Psychiatry. 2010;81(8): 828-33. https://doi.org/10.1136/jnnp.2009.187302.
- Charcot Marie Tooth Association. A Guide to Physical and Occupational Therapy for CMT https://www.cmt.org.au/uploads/pdf/CMTA_PT_OT_Guidel_9_2018_DT.pdf 2018.



