Abstract
It has long been recognised that sleep and deprivation of it have important consequences for cortical excitability, the electroencephalogram and seizure control. However, in the management of people with epilepsy, it is also important to recognise that epilepsy and its treatment may also have significant implications for sleep. Lack of consideration for this bidirectional relationship between sleep and epilepsy may have negative consequences on individuals’ seizure control, quality of life, and other aspects of their health.
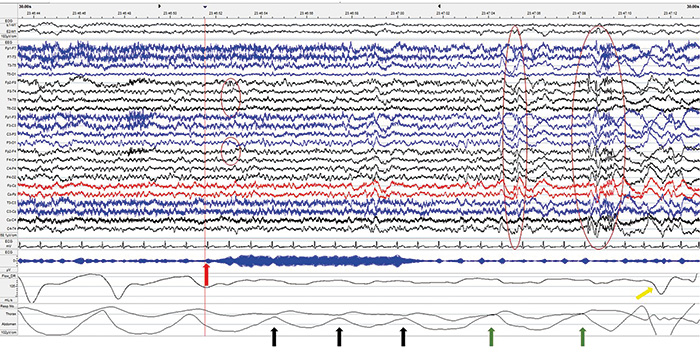
The fact that sleep and epilepsy are intimately related is evident in clinical practice. Many patients in the epilepsy clinic exhibit close links between sleep and their seizures. Indeed, this association extends to our investigation of epilepsy, with the recognition that sleep deprivation and sleep itself may accentuate epileptic features on the electroencephalogram (EEG), and that EEG recordings in these states may increase sensitivity and yield.
There is growing evidence that management of sleep disorders and the improvement of sleep quality may influence seizure frequency and other outcome measures. Despite this, for persons with epilepsy and sleep complaints, there is a tendency to ascribe symptoms such as fatigue, tiredness or excessive daytime sleepiness, to anti-seizure medications, rather than questioning whether they may be due to a sleep disorder. Conversely, epilepsy and its management may also influence sleep. Insomnia as an adverse effect of anti-epileptic drugs (AEDs) is also frequently under-recognised, and epileptic discharges may disrupt sleep or even trigger parasomnias.
It is clear therefore that the relationship between sleep and epilepsy is bidirectional. In view of the prevalence of sleep disorders, consideration of sleep should be included in the routine management of patients with epilepsy.
The effects of sleep on epilepsy
Beyond specific epilepsy syndromes, seizures often follow a circadian pattern, presumably related to the effects of circadian rhythms on brain activity. Seizures arising from different brain locations appear to have different patterns. For example, mesial temporal and occipital lobe seizures in adults are more likely to occur in the mid-afternoon, while seizures of parietal or frontal lobe origin are more likely to occur in the early hours of the day [2]. These data have been gathered both from the analysis of in-hospital telemetry and long-term out-patient recordings from implanted neurostimulators [3].
Two mechanisms have been proposed to mediate the influence of the circadian rhythm on seizures [4]. Firstly, clock genes such as BMAL1 and CLOCK contribute to epileptic excitability. Secondly, the mammalian target of rapamycin (mTOR) pathway is regulated by the circadian timing system. The mTOR pathway has been implicated in a range of neurological disorders, including epilepsy.
The stages of sleep also have a profound impact on epilepsy. Seizures, and indeed epileptic abnormalities on the EEG, are rarely seen in rapid eye movement (REM) sleep [5]. Even in non-REM sleep, seizures are more likely to arise from non-REM stage 1 (N1) and stage 2 (N2) sleep, and occasionally patients do exhibit a marked tendency to have seizures when non-REM sleep is unstable, particularly when transitioning from deeper to lighter stages of non-REM sleep.
Disruption of sleep as a result of behaviour or through sleep disorders is a frequent precipitant of seizures. Of the provoking factors described by almost all patients with epilepsy, acute and probably chronic sleep loss is the most frequently cited, and of course in the clinical setting, acute sleep deprivation is utilised in an attempt to provoke seizures or to accentuate interictal epileptiform discharges on the EEG. Obstructive sleep apnoea (OSA) is also increasingly recognised as an important factor in epilepsy control. Several studies have reported a high prevalence of OSA in epilepsy patients [6], with some indication that prevalence is higher than in the general population [7]. Approximately one third of patients with drug-resistant epilepsy have obstructive sleep apnoea (OSA), and OSA is correlated with poorer epilepsy control. A recent pilot study comparing continuous positive airway pressure (CPAP) against sham demonstrated a larger reduction of seizure frequency in the CPAP group, and in a further study, CPAP adherence resulted in a reduction of seizure frequency that was not seen in those patients that were non-adherent. Similar findings have been reported in children with epilepsy and OSA; adenotonsillectomy was associated with a reduction in seizure frequency. Proposed mechanisms for this association include sleep fragmentation and chronic sleep loss, EEG arousals and intermittent hypoxaemia. Insomnia has also been associated with more frequent seizures, depressive symptoms and poorer quality of life [8].
Effects of epilepsy on sleep
Epilepsy may directly or indirectly – through its management – influence sleep. In individuals with epilepsy, both excessive daytime sleepiness and sleep fragmentation are common complaints, and up to half report insomnia. Sleep disorders are common in the general population, and thus it is not surprising that they are common in patients with epilepsy either. However, there are some sleep issues specifically related to individuals with epilepsy. Nocturnal seizures may result in significant sleep fragmentation, and may precipitate arousals generating non-REM parasomnias such as confusional arousals or even sleep-walking. Furthermore, nocturnal epileptic activity may be mistaken for non-REM parasomnias.
Daytime seizures may also influence sleep architecture and levels of sleepiness, both subjectively as reported by patients and through objective measures such as maintenance of wakefulness testing [9].
The treatment of epilepsy is also a common cause of sleep disturbance. It is well-recognised that the majority of AEDs may cause sleepiness, but the weight gain associated with some AEDs may increase the risk of sleep-disordered breathing, and drugs like lamotrigine and levetiractam can precipitate severe insomnia in a small proportion of individuals. AEDs can also have varying effects on sleep architecture, differentially altering proportions of light and deep non-REM sleep and REM sleep [10]. Vagus nerve stimulation may also disrupt sleep, with stimulation triggering central or obstructive apnoeic events or stridor [11].
Evaluation of sleep in the individual with epilepsy
In the management of persons with epilepsy and sleep complaints, particularly sleepiness, it is important to recognise that co-morbid sleep disorders are more likely to be the driver than the epilepsy or the AEDs prescribed [12]. Therefore, while it is obviously relevant to focus on the epilepsy and medication regimen, a clinical assessment in the form of a sleep history should be undertaken. While many validated sleep questionnaires exist, there are none specific to epilepsy. These can be used for screening purposes, e.g. the Sleep Condition Indicator (an eight-item rating scale for insomnia), or the Pittsburgh Sleep Quality Index (useful for prompting an exploration of several different domains of sleep). These questionnaires however should not be seen to replace a full history. The Epworth Sleepiness Scale is a useful clinical tool for measuring subjective sleepiness, with a score of 10 or more viewed as pathological, and a very low score perhaps suggesting insomnia. Short questionnaires such as STOP-BANG can aid screening for OSA.
In addition to correlating the temporal relationship between sleep symptoms, seizure control and medication changes, the history should focus on the rapid identification of co-morbid sleep disorders, for the purposes of a consultation in the epilepsy clinic. Areas of particular relevance include the ascertainment of adequate sleep opportunity, difficulties in initiating or maintaining sleep, features of obstructive sleep apnoea such as loud snoring, witnessed apnoeas, nocturia, or a dry mouth, sore throat or headache on waking, or symptoms of restless legs syndrome such as nocturnal urge to move and periodic limb movements of sleep or wake.
The investigation of sleep disorders in patients with epilepsy does not necessarily require expensive specialist technology, although for some patients combined polysomnography and EEG is necessary; it should be noted that standard polysomnography only provides four channels of EEG, which is rather limited for the full evaluation of patients with epilepsy. A simple sleep diary may help identify those patients who are behaviourally sleep-restricted or have insomnia, while home respiratory testing ranging from simple overnight oximetry to full-respiratory polygraphy will be sufficient to diagnose most cases of sleep-disordered breathing and periodic limb movement disorder. In-patient or home video-telemetry is generally utilised in those individuals with unusual behaviours at night, where epileptic arousals or seizures are suspected, or in those in whom a co-morbid hypersomnia of central origin is in the differential.
Management
In patients with epilepsy with a sleep complaint, the first step is to ensure that a possible iatrogenic cause is reversed if possible. Phenobarbital is considered the most sedating, but most AEDs can precipitate or worsen sleepiness, and a temporal relationship between symptoms and prescribing should be sought. Insomnia is particularly associated with lamotrigine and levetiracetam, but may also be seen with other drugs that are more typically associated with sedation, such as pregabalin [13].

In the absence of clear drug causality, co-morbid sleep disorders should be treated [14]. Insomnia may be improved through cognitive behavioural therapy for insomnia [15] (CBTi), the gold-standard first line treatment for insomnia disorder [16]. In epilepsy however, standard CBTi should be modified to replace sleep restriction, which may provoke seizures, with sleep compression. Group CBTi, widely practised in the NHS, may not be appropriate for this cohort of patients as a result. Pharmacological approaches include utilising AEDs that may shorten sleep latency, e.g. pregabalin, gabapentin, perampanel, or standard treatments for insomnia such as melatonin, or sedating antidepressants. Prolonged release melatonin in particular is viewed as a relatively safe long-term pharmacological therapy for insomnia, although its efficacy in epilepsy has thus far only been demonstrated in children [17]. Benzodiazepines and Z-drugs such as zopiclone should only be prescribed for up to two weeks where the primary indication is insomnia, although occasionally clobazam can be helpful.
OSA should be managed in the same vein as in the general population, with one or two exceptions. Weight loss is effective in the management of OSA [18], and this can sometimes be facilitated by the weaning of AEDs predisposing to weight gain, or rarely initiation of topiramate (topiramate in conjunction with phentermine has been demonstrated to show both reduction in body-mass index and apnoea-hypopnoea index in a placebo-controlled trial [19]). Mandibular advancement devices are widely used for mild OSA, but the author’s own practice is to studiously avoid usage in an individual with epilepsy, for fear of obstructing the airway during a nocturnal seizure, unless there is no alternative. Epilepsy is usually seen as a contraindication, but there are some case reports of well-fitting devices being used, and the author is aware that not all clinicians take this view, particularly with bespoke devices that fit well and are less likely to be displaced. Continuous positive airway pressure is the treatment of choice, and as described above, may have significant benefits on seizure control.
Other conditions like restless legs syndrome (RLS) and periodic limb movement disorder are best managed utilising alpha-2-delta ligand (gabapentinoid) AEDs that are also widely adopted, if unlicensed, treatments. These drugs are increasingly being proposed as first-line treatments for RLS in international guidelines [20]. There are obviously concerns regarding illicit use, and these drugs should be given once nightly, and at the lowest dose possible. However, these drugs should be used cautiously in patients with primary epilepsy syndromes as they may worsen or indeed precipitate the new onset of absences and myoclonic seizures. In these cases, treatment with dopa agonists or clonazepam (also unlicensed) may be preferable.
Conclusion
Sleep problems are extremely common in patients with epilepsy, and beyond simply influencing quality of life, can have a significant impact on seizure control, cognition and mood. Therefore, the recognition and management of sleep disorders should be an essential aspect of the review of patients in the epilepsy clinic.
References
- Kothare SV, Kaleyias J. Sleep & epilepsy in children & adolescents. Sleep Medicine. 2010;11:674-685. https://doi.org/10.1016/j.sleep.2010.01.012
- Hofstra WA, Grootemarsink BE, Dieker R, van der Palen J, de Weerd AW. Temporal distribution of clinical seizures over the 24-h day: a retrospective observational study in a tertiary epilepsy clinic. Epilepsia. 2009;50(9):2019-26. https://doi.org/10.1111/j.1528-1167.2009.02044.x
- Spencer D, Sun F, Brown S, Jobst B, Fountain N, Wong V, Mirro E, Quigg M. Circadian and ultradian patterns of epileptiform discharges differ by seizure-onset location during long-term ambulatory intracranial monitoring. Epilepsia. 2016;57(9):1495-1502. https://doi.org/10.1111/epi.13455
- Khan S, Nobili L, Khatami R, Loddenkemper T, Cajochen C, Dijk DJ, Eriksson SH. Circadian rhythm and epilepsy. Lancet Neurol. 2018;17:1098-108. http://dx.doi.org/10.1016/ S1474-4422(18)30335-1
- Ng M, Pavlova M. Why are seizures rare in rapid eye movement sleep? Review of the frequency of seizures in different sleep stages. Epilepsy Res Treat. 2013:932790. https://doi.org/10.1155/2013/932790
- Malow BA, Levy K, Maturen K, Bowes R. Obstructive sleep apnea is common in medically refractory epilepsy patients. Neurology 2000; 55(7): 1002-7. https://doi.org/10.1212/WNL.55.7.1002
- Lin Z, Si Q, Xiaoyi Z. Obstructive sleep apnoea in patients with epilepsy: a meta-analysis. Sleep Breath. 2017;21(2):263-270. https://doi.org/10.1007/s11325-016-1391-3
- Quigg M, Gharai S, Ruland J, Schroeder C, Hodges M, Ingersoll KS, Thorndike FP, Yan G, Ritterband LM. Insomnia in epilepsy is associated with continuing seizures and worse quality of life. Epilepsy Res 2016;122:91-6. https://doi.org/10.1016/j.eplepsyres.2016.02.014
- Bazil CW, Castro LH, Walczak TS. Reduction of rapid eye movement sleep by diurnal and nocturnal seizures in temporal lobe epilepsy. Arch Neurol. 2000;57(3):363-8. https://doi.org/10.1001/archneur.57.3.363
- Shvarts V, Chung S. Epilepsy, antiseizure therapy, and sleep cycle parameters. Epilepsy Res Treat. 2013;670682. https://doi.org/10.1155/2013/670682
- Perez-Carbonell L, Faulkner H, Higgins S, Koutroumanidis M, Leschziner G. Vagus nerve stimulation for drug-resistant epilepsy. Pract Neurol. 2020;20(3):189-98. https://doi.org/10.1136/practneurol-2019-002210
- Malow BA, Bowes RJ, Lin X. Predictors of sleepiness in epilepsy patients. Sleep. 1997;20(12):1105-10. https://doi.org/10.1093/sleep/20.12.1105
- Piedad J, Rickards H, Besag FMC, Cavanna AE. Beneficial and adverse psychotropic effects of antiepileptic drugs in patients with epilepsy: a summary of prevalence, underlying mechanisms and data limitations. CNS Drugs. 2012;26(4):319-35. https://doi.org/10.2165/11599780-000000000-00000
- Latreille V, St Louis EK, Pavlova M. Co-morbid sleep disorders and epilepsy: a narrative review and case examples. Epilepsy Res. 2018;145:185-197. https://doi.org/10.1016/j.eplepsyres.2018.07.005
- Van der Zweerde T, Bisdounis L, Kyle SD, Lancee J, van Straten A. Cognitive behavioral therapy for insomnia: a meta-analysis of long-term effects in controlled studies. Sleep Med Rev. 2019;48:101208. https://doi.org/10.1016/j.smrv.2019.08.002
- Wilson S, Anderson K, Baldwin D, Dijk DJ, Espie A, Espie C, Gringras P, Krystal A, Nutt D, Selsick H, Sharpley A. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders: an update. J Psychopharmacology. 2019;33(8):923-947. https://doi.org/10.1177/0269881119855343
- Jain SV, Horn PS, Simakajornboon N, Beebe DW, Holland K, Byars AW, Glauser TA. Melatonin improves sleep in children with epilepsy: a randomized, double-blind, crossover study. Sleep Med. 2015;16(5):637-44. https://doi.org/10.1016/j.sleep.2015.01.005
- Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep-disordered breathing. JAMA. 2000;284(23):3015-21. https://doi.org/10.1001/jama.284.23.3015
- Winslow DH, Bowden CH, DiDonato KP, McCullough PA. A randomize, double-blind, placebo-controlled study of an oral, extended-release formulation of phentermine/topiramate for the treatment of obstructive sleep apnea in obese adults. Sleep. 2012;35(11):1529-39. https://doi.org/10.5665/sleep.2204
- Manconi M, Garcia-Borreguero D, Schormair B, Videnovic A, Berger K, Ferri R, Dauvilliers Y. Restless legs syndrome. Nature Reviews Disease Primers 2021;7:80. https://doi.org/10.1038/s41572-021-00311-z
