Summary
- Social cognition difficulties include problems with understanding the mental perspectives and intentions of others (mentalising), emotion recognition, affective responses to social cues, affect regulation and social problem-solving and decision making.
- The assessment and rehabilitation of social cognition difficulties is a relatively embryonic and underdeveloped field in neuro-rehabilitation, despite the widespread prevalence of such difficulties across neurological conditions.
- The currently small range of interventions offered have diverged from initial social skills training approaches to include the specific training of component social cognitive abilities, approaches that use the body to aid in the comprehension of social information and approaches that use live interactions in social relationships as a core focus of the intervention.
Abstract
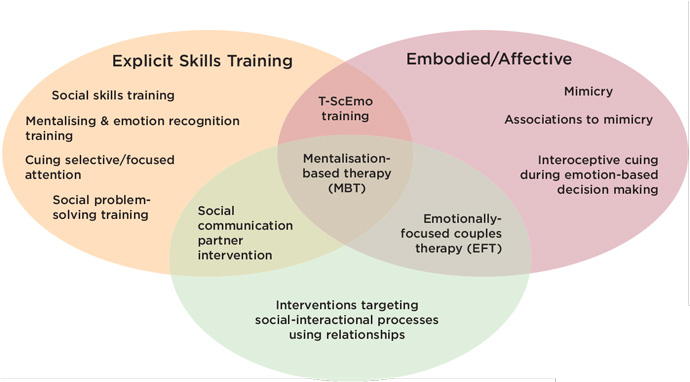
This article provides an overview of interventions developed and trialled in the embryonic field of social cognition neuro-rehabilitation. Interventions are categories under the headings of explicit skills training, embodied/relational interventions, and relational approaches.
The assessment and treatment of social neuropsychological impairments have received comparably less attention and development than other domains of cognition. These include difficulties in representing the intentions and perspectives of others (mentalising), recognising emotions, inferring nuanced social communications such as sarcasm and deceit, accessing social knowledge, and emotion-based decision-making. Founded on distributed neuroanatomical substrates, impairments of these functions have been found to be present and enduring across major sub-groups of acquired brain injury (for review see [1]). The theoretical richness of the social neuroscience revolution has not been matched by the translation of concepts and findings into rehabilitation practice. This article will review the embryonic field of social cognition rehabilitation, categorised into three intervention clusters: a) explicit skills training, b) embodied and affective interventions and c) relational approaches.
Explicit skills training
Social skills training for various clinical groups predates neuro-rehabilitation of social functioning. These were initially focused on teaching and role-playing social and communicative behaviours without an underlying neuropsychological rationale, and examples of these approaches did feature in the neuro-rehabilitation literature over two decades ago [2,3]. More recently, both simple instructions and multi-media packages (using audio-visual interactive computer software stimuli) have been used to target specific social cognitive functions such as emotion recognition from face and/or voice, across a range of clinical groups, including psychosis [4] and acquired brain injury [5-8]. Other interventions have focused on multiple social receptive and behavioural functions, including emotion recognition and mentalising abilities [9-10]. Elsewhere, clinical and experimental studies have reported gains from training cognitive control operations adjunctive to mentalising and emotion recognition, such as focusing attention to certain parts of the face [11-12] and social problem-solving [13].
These approaches are indirectly informed by theoretical frameworks that emphasise the intentional elements of social cognition functions [14], such as mentalising and emotion recognition. Skills in accurately inferring/comprehending the perspectives of others (from visual, auditory and contextual aspects of communication) or identifying essential facial features (e.g., eyes, mouth) and matching with intact or relearned knowledge of differing emotional expressions. While some of the social-cognitive abilities supported in this way have become more diverse over time, they may not have a significant impact on the spontaneous, intense and changing nature of real-world social interactions. In addition, the studies above report mixed results in terms of intervention efficacy. However, some aspects of neuro-rehabilitation would clearly benefit from incorporating such approaches. An example would be vocational rehabilitation, where post-injury work performance involving formalised or scripted sets of narrowly defined social interactions with customers would be amenable to these social cognition rehabilitation packages.
Embodied & affective interventions
New theories and paradigms gaining prominence in social neuroscience, particularly following the discovery of neural mirroring systems, are accounts of embodied simulation, contagion and resonance [15]. These collectively emphasise the body-based affective / emotional and non-intentional dimensions of social cognition, such as the involuntary mimicry of facial musculature in response to the emotional expressions of others. In some scenarios, such as the experience of intense love for another, there is a deactivation of brain areas associated with intentional mentalising systems alongside activation of these automatic, affective processes.
These theoretical emphases have begun to influence innovations in the rehabilitation of emotion recognition. Skye McDonald and colleagues in Australia [11] have evaluated a protocol where survivors of traumatic brain injury first approximate their facial expression to a task stimulus (e.g., an angry face) prior to identifying that emotion. Jacoba Spikman and colleagues in the Netherlands recently reported details of their multi-modal ‘T-ScEmo’ intervention [10]. This includes emotion recognition training involving instructed facial mimicry, together with additional cues to associate the proprioceptive feeling of the survivor’s facial expression with previous memories of similar sensations.
However, these studies have reported mixed findings across participants and weak group effects. This may be related to sample characteristics, but also these approaches are necessarily making a process intentional (e.g., the experimenter instructing a survivor to mimic their face to a stimulus) that in natural occurrence, in healthy populations, is considered to happen involuntarily. The question is raised as to whether the same underlying process is being exploited in both healthy functioning and clinical rehabilitation.
Experimental studies of survivors’ autonomic nervous system, bodily-mediated responses to both social cues (e.g., displays of distress), and during emotion-based decision-making tasks have highlighted blunted responsivity [16]. Some authors have explored the hypothesis of a raised threshold for a triggered autonomic response conducive to adaptive social cognitive functioning, rather than a complete absence of such [1]. Evans, Bowman and Turnbull [17] have reported improvements on an emotion-based decision-making task if clinical participants are directed to amplify their internal monitoring of bodily feelings (interoception) during task performance.
Relational approaches
The few approaches described thus far have focused on the individual survivor, conceptualising isolated social inputs and outputs, and their remediation/compensation. Fewer approaches still have actively used the relationships and presence of significant others themselves within social cognition rehabilitation. There is some evidence that this may be an important new direction for rehabilitation innovation, truly social cognitive interventions.
In mental health psychotherapy literature, an approach known as mentalisation-based therapy (MBT18) has been developed in use with clinical groups who also demonstrate varied social cognition impairments, such as those with a Borderline Personality Disorder diagnosis. In MBT the therapeutic relationship with the clinician is used as the main vehicle to identify breaks in accurate mentalising, together with the characterising features of mentalising errors. MBT is practiced both as an individual and family therapy, and while yet to be formally evaluated within neuro-rehabilitation, offers significant face validity as a potential intervention.
Togher and colleagues [19] reported an RCT of the provision of communication partners to train survivor social communication skills through live interactions and a stable social relationship. Finally, Yeates and colleagues [20] report the use of a couples therapy intervention for survivors with both executive and social cognition impairments and their partners (who have been shown in previous research to emotionally withdraw and so provide fewer cues for survivors). Using case study quantitative evaluations of changes in measures of psychological distress and relationship functioning in survivors and partners, these findings tentatively support the ‘raised threshold for autonomic responsivity’ hypothesis mentioned above. In this case, both survivor bodily responses and the socio-emotional cuing of the partner is amplified to maximise affective empathic survivor responses and adaptive relationship functioning.
Conclusions
This is an area of rehabilitation in its very infancy, with a significantly limited evidence base. On the one hand, trials of social skills, emotion recognition and mentalising interventions have not used sufficiently ecologically-valid or meaningful outcomes. On the other hand, approaches informed by contemporary social neuroscience theories that aim to support a natural embodied process have reported mixed group findings or case study data, limited in its generalisability. However, the range of approaches and conceptual frameworks being developed in this young field is notably diverse, at last in dialogue with current exciting developments in social neuroscience. These approaches, represented in Figure 1, signpost the range of possible directions for future innovation in social cognition rehabilitation.
References
- Yeates GN. Towards the neuropsychological foundations for couples therapy following acquiredbrain injury (ABI): A review of empirical evidence and relevant concepts. Neuro-Disability & Psychotherapy, 2013;1(1):117-50.
- Boake C. Social skills training following head injury. In J.S. Kreutzer & P.H. Wehman (Eds.), Cognitive Rehabilitation for Persons with Traumatic Brain Injury: A Functional Approach. 1991. Baltimore, MD: Paul H. Brookes.
- Brotherton FA, Thomas, LL, Wisotzek IE & Milan MA. Social skills training in the rehabilitation of patients with traumatic closed head injury. Archives of Physical Medicine and rehabilitation; 1988:69:826-32.
- Russell TA, Chu E & Phillips ML. A pilot study to investigate the effectiveness of emotion recognition remediation in schizophrenia using the micro-expression training tool. The British Journal of Clinical Psychology, 2006;45:579-84. https://doi.org/10.1348/014466505X90866
- Bornhofen C & McDonald S. Comparing strategies for treating emotion perception deficits in traumatic brain injury. Journal of Head Trauma and Rehabilitation, 2008;23(2):103-15. https://doi.org/10.1097/01.HTR.0000314529.22777.43
- Guercio JM, Podolska-Schroeder H & Rehfeldt RA. Using stimulus equivalence technology to teach emotion recognition to adults with acquired brain injury. Brain Injury, 2004;18(4);593-601. https://doi.org/10.1080/02699050310001646116
- McDonald S, Togher L, Tate R, Randall, R, English, T & Gowland, A. A randomised controlled trial evaluating a brief intervention for deficits in recognising emotional prosody following severe ABI. Neuropsychological Rehabilitation, 2012;23(2):267-86. https://doi.org/10.1080/09602011.2012.751340
- Radice-Neumann D, Zupan B, Tomita M & Willer B. Training emotional processing in persons with brain injury. Journal of Head Trauma Rehabilitation, 2009;24(5):313-23. https://doi.org/10.1097/HTR.0b013e3181b09160
- McDonald S, Tate R, Togher L, Bornhofen C, Lon, E, Gertler P, & Bowen R. Social skills treatment for people with severe, chronic acquired brain injuries: A multi-center trial. Archives of Physical Medicine & Rehabilitation, 2008;89:1648-59. https://doi.org/10.1016/j.apmr.2008.02.029
- Spikman JM, Westerhoff-Evers M, Visser-Keizer A. Neuropsychological rehabilitation of social cognitive impairments resulting in behavioural changes. Workshop presented at the Mid-Year Meeting of the International Neuropsychological Society, 2013. Amsterdam, Netherlands.
- McDonald S, Bornhofen C. & Hunt C. Enhancing emotion recognition after severe traumatic brain injury: the role of focused attention and mimicry. Neuropsychological Rehabilitation, 2009;7:1-9.
- McDonald S, Rushby J, Li S, de Sousa A, Dimoska A, James C, Tate R. & Togher L. The influence of attention and arousal on emotion perception in adults with severe traumatic brain injury. International Journal of Psychophysiology, 2011;82(1):124-31. https://doi.org/10.1016/j.ijpsycho.2011.01.014
- Rath J, Hennessy JJ. & Diller L. Social problem solving and community integration in postacute rehabilitation outpatients with a traumatic brain injury. Rehabilitation Psychology, 2003;48(3):137-44. https://doi.org/10.1037/0090-5550.48.3.137
- Frith U. & Frith CD. Development and neurophysiology of mentalizing. Philosophical Transactions of the Royal Society London B, Biological Sciences, 2003;358:459-73. https://doi.org/10.1098/rstb.2002.1218
- Gallese V, Keysers C. & Rizzolatti G. A unifying view of the basis of social cognition. Trends in Cognitive Sciences, 2004;8:396-403. https://doi.org/10.1016/j.tics.2004.07.002
- Damasio AR. Descartes’ Error: Emotion, Reason and the Human Brain. 1994; New York: Grosset/Putnam.
- Evans CEY, Bowman CH. & Turnbull OH. Subjective awareness on the Iowa Gambling Task: The key role of emotional experience in schizophrenia. Journal of Clinical & Experimental Neuropsychology, 2005;27:656-64. https://doi.org/10.1081/13803390490918354
- Bateman AW. & Fonagy P. The Handbook of Mentalization-Based Therapy in Mental Health Practice. 2012; New York: American Psychiatric Publishing.
- Togher L, McDonald S, Tate R, Power E. & Rietdjick R. Training communication partners for people with traumatic brain injury: Reporting the protocol for a clinical trial. Brain Impairment, 2009;10(2):188-204. https://doi.org/10.1375/brim.10.2.188
- Yeates GN, Edwards A, Murray C. & Creamer N. The use of emotionally-focused couples therapy (EFT) for survivors of acquired brain injury with social cognition and executive functioning impairments and their partners: A case series analysis. Neuro-Disability & Psychotherapy, 2013;1(2):151-94.
