Abstract
Whether surgical intervention benefits patients or patient subgroups with intracerebral haemorrhage (ICH) remains controversial, despite numerous randomised controlled trials. However, ICH without intervention has an extremely high mortality rate, with significant disability in many survivors. Consequently, there are a wide variety of practices worldwide, from near-routine intervention in large ICH to near-complete avoidance of surgery. We review the evidence behind ICH surgical intervention, discuss peri-operative management, and also mention ongoing trials of early minimally-invasive surgery, which may strengthen the evidence base in this challenging field.
Intracerebral haemorrhage (ICH), despite being proportionally far less common than ischaemic stroke, causes a greater global burden of disease, due to mortality approaching 40%, and high disability rates in survivors [1]. Apart from stroke unit care, evidence for ICH surgical and medical interventions is weak, leading to large variations in clinical practice. This review covers current surgical controversies, techniques used for ICH, current guidelines for perioperative management, and outlines current trials aiming to strengthen the surgical intervention evidence base.
Surgical trial evidence overview
Surgical intervention for ICH is controversial. Excepting strong evidence of a mortality reduction for ventricular draining in patients with intraventricular haemorrhage (IVH) and hydrocephalus, there is no RCT-based Class 1 evidence for any surgical intervention, whether via minimally invasive surgery (MIS) or conventional craniotomy [2]. A key challenge faced in ICH Randomised Controlled Trial (RCT) design is navigating clinical equipoise in a highly fatal and comorbid condition. Investigators may deem enrolment unethical, or alternately, deem intervention a priori futile, limiting trial recruitment to narrow patient subpopulations. As clinical deterioration from mass effect is common, patient crossover to emergency surgical treatment may contaminate surgical trials.
The landmark (but neutral) craniotomy-based Surgical Trial in IntraCerebral Haemorrhage (STICH) found early surgery of patients with ICH (versus initial conservative treatment) was not associated with functional improvement. However, patients were only randomised if treating clinicians felt equipoise existed. Furthermore, screening logs were not kept and 25% of patients crossed over to surgical treatment, limiting interpretation [3]. Subsequent craniotomy trial individual patient meta-analysis suggested early (<8 hours) intervention may be beneficial [4]. Additionally there was potential benefit for patients aged<70, with moderate neurological deficits and ICH volumes, with superficial clots benefiting most [4]; however the STICH-2 trial which targeted some of these characteristics was neutral [5]. Despite a dearth of RCT-based evidence, surgical intervention for deteriorating patients with large cerebellar ICH is routinely performed on the basis of observational data strongly suggesting a mortality reduction; an RCT is unlikely.
Meta-analyses of MIS trials suggests overall benefit, although analysis is complicated by differing surgical techniques [6]. The largest MIS trial (MISTIE-III) did not demonstrate functional improvement benefit [7], however a mortality benefit was observed. Nevertheless, functional outcome seemed improved in patients with optimal evacuation (predefined as <15 mL residual volume) [7]. This suggested that surgical efficacy (influenced by technique and experience) may be a key determinant of functional outcome.
Surgical Techniques
Lacking clear evidence of optimal target population or technique, ICH surgical cohorts and approaches differ significantly between regions and institutions. For instance, craniopuncture-based craniotomy is reported as ‘standard of care’ for ICH in China, but is largely not performed elsewhere [8].
The two main aims of surgery (which may overlap) are (1) to treat or prevent intracranial hypertension and (2) to limit perihematomal brain injury.
(1) Preventing and treating intracranial hypertension
ICH can increase intracranial volume by multiple mechanisms (mass effect from the haematoma and perihematomal oedema, hydrocephalus from IVH and/or secondary hydrocephalus from herniation). IVH-related hydrocephalus can be acute (from blood clot-related obstruction) or delayed (a post-IVH inflammatory response reducing cerebrospinal fluid resorption) [9]. Hydrocephalus may exist in isolation or complicate mass effect. While medical approaches to intracranial hypertension are largely ineffective [2], surgical intervention can ameliorate hydrocephalus and potentially prevent fatal transtentorial herniation by ICH debulking (reducing mass effect), and/or increasing intracranial volume (the latter is the focus of the SWITCH trial (Swiss Trial of Decompressive Craniectomy Versus Best Medical Treatment of Spontaneous Supratentorial Intracerebral Hemorrhage (www.clinicaltrials.gov NCT02258919)). It is probable (though it remains unproven) that surgical intervention can be life-saving. This is reflected in stroke guidelines internationally (for instance, the most recent American Heart Association guidelines state it might be considered in deteriorating patients as a lifesaving measure (Class 2B, Level of Evidence-C)). A combination of significant midline shift and deteriorating conscious state portends intervention, where deemed appropriate [10]. However, as summarised previously, it is uncertain whether and to what degree intervention may improve functional outcome beyond reducing mortality.
Ventricular drainage is strongly advised to reduce mortality in patients with hydrocephalus secondary to ICH +/- IVH contributing to impaired conscious state [2]. A recent meta-analysis suggests concurrent administration of intraventricular fibrinolysis may both decrease mortality and improve functional outcomes, especially when administered early [11], however in the CLEAR-III trial, a mortality benefit from fibrinolytic-enhanced ventricular drainage was accompanied by increased severe disability in survivors [12].
(2) Limiting perihaematomal injury
Excepting reduction of above mass effect benefits of haematoma evacuation are theoretical. It is possible, with ultra-early intervention, that haematoma expansion may be directly curtailed, however with most ICH expansion occurring in the first 2-3 hours [13], the optimal time-window for this benefit seems currently unfeasible. Haematoma evacuation may prevent ICH-related secondary injury. Intra-haematomal cytotoxic substances (most notably thrombin in the earlier time-frame and, later, iron from haemolysis) seem experimentally to mediate peri-haematomal injury and oedema [14]. Therefore their removal may be beneficial. Haematoma evacuation can occur via craniotomy or MIS, which is technically varied.
MIS techniques
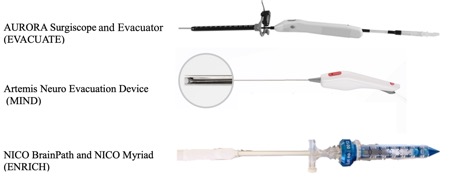
Figure 1: The devices used in current and upcoming minimally invasive surgical trials: The AURORA Surgiscope and Evacuator are being used in the EVACUATE trial. The Artemis Neuro Evacuation Device is being used in the MIND trial. The NICO BrainPath and Myriad are being used in the ENRICH trial.
The three main approaches are craniopuncture, stereotactic thrombolysis and endoscopic removal. Craniopuncture is mostly utilised in China, and involves intra-haematomal placement of a YL-1 needle, skull fixation of the cannula and then hematoma aspiration, initially freely followed by fibrinolytic-augmented aspiration over several days. This approach is untested outside Chinese settings [8].
An analogous approach was tested in the Western MISTIE-III trial, enrolling patients with large (≥30mL) supratentorial ICH within 72 hours of onset, following a stability scan ≥6 hours after initial imaging. A 4.8mm cannula was inserted and 8-hourly fibrinolytic-augmented aspiration ensued (9 doses maximally) aiming for <15mL residual [15].
Direct MIS ICH removal can occur via several stereotactic endoscopic or endoscope-like approaches. Such techniques have included combining a Storz endoscope (Tuttlingen, Germany) via a 6.3mm introducer sheath with the Artemis evacuation system (Penumbra, CA, USA); combining the Aurora Surgiscope and Evacuator (Integra Lifesciences, NJ, USA. 11.5mm external diameter); and combining the BrainPath Endoport with the Myriad handpiece (Nico Corp, IN, USA, 15.8 mm external diameter) (Figure 1). These techniques allow direct visually-guided haematoma evacuation and facilitate direct surgical haemostasis, thus minimising rebleeding risk. The best balance of surgical visibility (via a large port) versus minimising invasiveness (via a smaller port) remains unclear.
Peri-operative management
Regardless of approach, recommended perioperative care of patients includes facilitation of haemostasis, management of blood pressure, glucose, and temperature and thromboprophylaxis, although direct evidence of benefit in surgical cohorts is scant [2].
Pre-operatively, effective anticoagulation reversal is required, with prothrombin complex concentrate, idarucizumab, or andexanet alpha as appropriate [2]. Platelet transfusion in patients on aspirin undergoing craniotomy may lower the risk of rebleeding and improve functional outcome (in contrast with non-surgical patients, whom it may harm) [16]. Desmopressin and tranexamic acid remain investigational [2]. Systolic blood pressure targeting 140 mmHg, but not substantially below, is non-harmful and potentially beneficial. Euglycaemia and avoidance of fever is recommended [2].
Thromboprophylaxis is highly recommended, initially with intermittent pneumatic compression and then potentially low-dose unfractionated or low-molecular-weight heparin [2]. Although prophylactic antiepileptic medications are not indicated, patients with active clinical or electrographic seizures should be treated [2]. Following surgery, once safe to transfer patients, care within a stroke unit will probably improve outcomes [17].
Current RCTs and Future Directions
Given treatment-related uncertainties and clinically unmet need, there is significant global interest in further ICH surgical trials, especially MIS studies. For robust and generalisable trial results, consecutive recruitment avoiding ‘standard of care evacuation’ is optimal (and, we feel, justified given the uncertainty of evidence reflected in guidelines.)
The ENRICH trial (Early MiNimally-invasive Removal of IntraCerebral Hemorrhage (http://www.clinicaltrials.gov, unique identifier NCT02880878)) has been presented (American Association of Neurological Surgeons and European Stroke Organisation Conferences, 2023) but not yet published. A functional outcome benefit was demonstrated from relatively early (<24 hrs) clot evacuation via the Brainpath Endoport compared with medical management in 300 participants. Benefit appeared restricted to lobar ICH patients, with an anterior basal ganglia treatment subgroup terminated early for futility. The MIND study (Minimally Invasive Neuro Evacuation Device (NCT03342664)) enrols 500 patients within 72 hours of ICH onset, randomised 2:1 to minimally invasive endoscopic evacuation with the Artemis System or to medical management.
These minimally invasive techniques are combined with ultra-early time-frame intervention in several studies underway or in late-stage planning, utilising ischaemic stroke triage and evaluation pathways, and leveraging the theoretical benefits from earlier evacuation, suggested by pre-clinical studies, observational data and surgical trial meta-analysis. The EVACUATE trial (Ultra-Early, Minimally inVAsive intraCerebral Haemorrhage evacUATion Versus Standard treatment (NCT04434807)), employs the Aurora Surgiscope and Evacuator (Integra Lifesciences, NJ, USA), randomising 240-434 patients with ICH volumes ≥ 20mL to ultra-early surgery (<8 hrs) or standard care (expected reporting December 2026). The DIST trial (Dutch Intracerebral Hemorrhage Surgery Trial) enrols 600 patients with ICH volumes ≥ 10mL, randomising to similarly early surgery with any CE-approved device (currently only the Artemis system) or standard care.
Together with other ICH trials in advanced stages of planning, these results will inform the next generation of surgical ICH care and potentially (individually or combined) demonstrate patient subgroups who benefit from particular surgical interventions.
Conclusion
Surgical best-practice care for ICH patients remains controversial. Currently the best evidence for intervention is in patients with hydrocephalus, cerebellar ICH and patients with impending transtentorial herniation who may accept survival with a severe neurological deficit. Ongoing surgical treatment trials will help determine definitively whether surgical ICH evacuation (especially using minimally invasive techniques) improves functional outcomes, and which patients may maximally benefit.
References
- Krishnamurthi RV, Feigin VL, Forouzanfar MH, et al. Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. The Lancet Global Health 2013;1(5):e259-e281. https://doi.org/10.1016/S2214-109X(13)70089-5.
- Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the Management of Patients With Spontaneous Intracerebral Hemorrhage: A Guideline From the American Heart Association/American Stroke Association. Stroke 2022;53(7):e282-e361. https://doi.org/10.1161/STR.0000000000000407
- Mendelow AD, Gregson BA, Fernandes HM, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. Lancet 2005;365(9457):387-97.(In eng) https://doi.org/10.1016/S0140-6736(05)17826-X
- Gregson BA, Broderick JP, Auer LM, et al. Individual Patient Data Subgroup Meta-Analysis of Surgery for Spontaneous Supratentorial Intracerebral Hemorrhage. Stroke 2012;43(6):1496-1504. https://doi.org/10.1161/STROKEAHA.111.640284
- Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. The Lancet 2013;382(9890):397-408. https://doi.org/10.1016/S0140-6736(13)60986-1
- Hou D, Lu Y, Wu D, Tang Y, Dong Q. Minimally Invasive Surgery in Patients With Intracerebral Hemorrhage: A Meta-Analysis of Randomized Controlled Trials. Frontiers in Neurology 2022;12 (Systematic Review) (In English). https://doi.org/10.3389/fneur.2021.789757
- Hanley DF, Thompson RE, Muschelli J, et al. Safety and efficacy of minimally invasive surgery plus alteplase in intracerebral haemorrhage evacuation (MISTIE): a randomised, controlled, open-label, phase 2 trial. Lancet Neurol 2016;15(12):1228-1237. (In eng). https://doi.org/10.1016/S1474-4422(16)30234-4
- Hannah TC, Kellner R, Kellner CP. Minimally Invasive Intracerebral Hemorrhage Evacuation Techniques: A Review. Diagnostics (Basel) 2021;11(3) (In eng). https://doi.org/10.3390/diagnostics11030576
- Bu Y, Chen M, Gao T, Wang X, Li X, Gao F. Mechanisms of hydrocephalus after intraventricular haemorrhage in adults. Stroke Vasc Neurol 2016;1(1):23-27. (In eng). https://doi.org/10.1136/svn-2015-000003
- Flower O, Smith M. The acute management of intracerebral hemorrhage. Curr Opin Crit Care 2011;17(2):106-14. (In eng). https://doi.org/10.1097/MCC.0b013e328342f823
- Khan NR, Tsivgoulis G, Lee SL, et al. Fibrinolysis for Intraventricular Hemorrhage. Stroke 2014;45(9):2662-2669. https://doi.org/10.1161/STROKEAHA.114.005990
- Hanley DF, Lane K, McBee N, et al. Thrombolytic removal of intraventricular haemorrhage in treatment of severe stroke: results of the randomised, multicentre, multiregion, placebo-controlled CLEAR III trial. Lancet 2017;389(10069):603-611. (In eng). https://doi.org/10.1016/S0140-6736(16)32410-2
- Edlow BL, Bove RM, Viswanathan A, Greenberg SM, Silverman SB. The pattern and pace of hyperacute hemorrhage expansion. Neurocrit Care 2012;17(2):250-4. (In eng). https://doi.org/10.1007/s12028-012-9738-5
- Hua Y, Keep RF, Hoff JT, Xi G. Brain injury after intracerebral hemorrhage: the role of thrombin and iron. Stroke 2007;38(2 Suppl):759-62. (In eng). https://doi.org/10.1161/01.STR.0000247868.97078.10
- Hanley DF, Thompson RE, Rosenblum M, et al. Efficacy and safety of minimally invasive surgery with thrombolysis in intracerebral haemorrhage evacuation (MISTIE III): a randomised, controlled, open-label, blinded endpoint phase 3 trial. The Lancet 2019;393(10175):1021-1032. https://doi.org/10.1016/S0140-6736(19)30195-3
- Li X, Sun Z, Zhao W, et al. Effect of acetylsalicylic acid usage and platelet transfusion on postoperative hemorrhage and activities of daily living in patients with acute intracerebral hemorrhage. J Neurosurg 2013;118(1):94-103. (In eng). https://doi.org/10.3171/2012.9.JNS112286
- Langhorne P, Fearon P, Ronning OM, et al. Stroke unit care benefits patients with intracerebral hemorrhage: systematic review and meta-analysis. Stroke 2013;44(11):3044-9. (In eng). https://doi.org/10.1161/STROKEAHA.113.001564



