Definition and anatomy
Sciatica is a misnomer freely used to describe lumbar nerve root pain, rather than specific unilateral leg pain in a radicular distribution corresponding to the sciatic nerve (L4,L5,S1,S2). It is caused by nerve root compression in the lumbar spine due to either disc prolapse, osteophytes or ligamentous hypertrophy. These can all be accentuated by spondylolisthesis.
The annual incidence of low back pain is estimated at 5%, but only 1% develops radiculopathy [1]. Lumbar disc prolapse is a disease most common between 30 and 50 years of age, with a male preponderance, as well as an association with repeated mechanical forces and smoking. It may occur at any level, but 95% occur at L4/5 or L5/S1. In the older population, with chronically degenerative discs, compression of the nerve root is more likely to be due to facet joint or ligamentum flavum hypertrophy.
Nerve roots exit the spinal canal, below the pedicle of the same numbered vertebrae, but above the disc of the next caudal disc space. Nerve root compression can occur in three locations (Figure 1a and 1b):
a. A central disc prolapse compresses the thecal sac and the roots of the cauda equina that are contained within.
b. A lateral disc prolapse or lateral recess stenosis compresses the transiting nerve root just after it has bifurcated from the dural sac. For example a lateral L4/5 disc compresses the L5 nerve root.
c. A far lateral disc prolapse compresses the nerve root that exits the foramen at the level of the involved disc. For example a far lateral L4/5 disc prolapse can compress the L4 root.
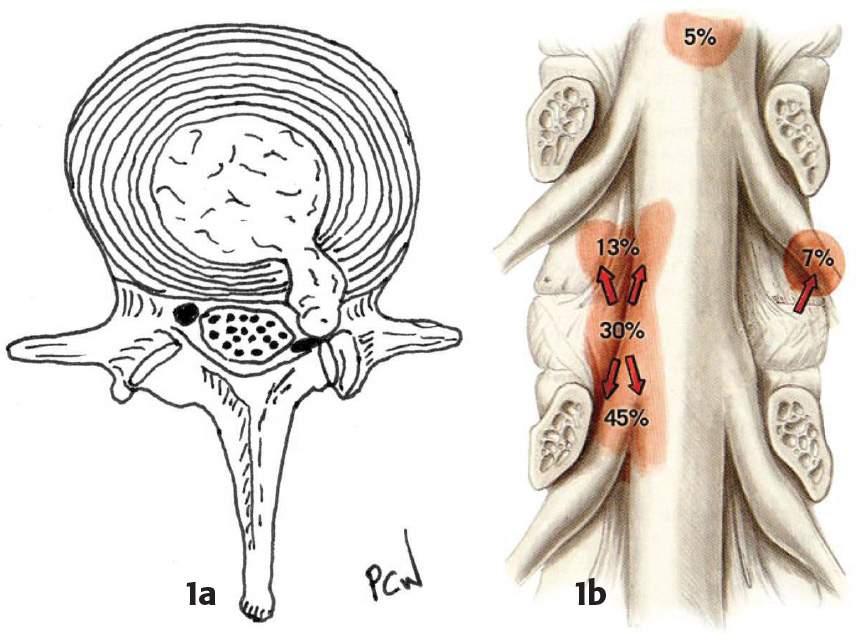
Figure 1b: A coronal view to demonstrate the anatomical relationship (and relative frequencies) of lumbar disc prolapse to the exiting and transiting nerve roots. Picture courtesy of http://www.spine-health.com
Presentation
1) Most patients present with low back pain, often of long duration, with a more recent onset of acute pain radiating into the lower limb. Frequently the pain may be accompanied by numbness, parasthesiae or weakness. The dermatomal distribution of the pain may give an indication of the level of the pathology but frequently the pain is myotomal being described as a severe, deep sited muscular ache associated with cramps (Table 1). Awkward movements or Valsalva manœuvres often exacerbate the pain (e.g. sneezing). Sudden resolution of leg pain, accompanied by motor or sensory deficit, is more likely to represent nerve root infarction than disc resorption.
2) Neurogenic claudication (from compression on the cauda equina) is the term attached to the syndrome of usually, bilateral leg pain or ache and increasing unsteadiness or loss of balance, precipitated by a progressively decreasing amount of walking. The symptoms are relieved by rest and/or forward flexion of the lumbar spine. It is this final relieving factor that, along with the absence of positive features or risk factors for vascular claudication, helps differentiate the two conditions. Both occur in the elderly population and without intervention are likely to be gradually progressive.
On examination, limited straight-leg raising and a positive stretch test on the affected side is often the only demonstrable sign (Lasegue) of a prolapsed disc. Patients with mid- or high lumbar or far lateral disc prolapse do not generally demonstrate these signs. Patients with lumbar canal stenosis usually do not harbour abnormal neurological signs. An L5/S1 disc prolapse is frequently associated with a reduced or absent ankle jerk. In the elderly, absent ankle jerks are of low diagnostic specificity. L5 root compression frequently causes weakness of extensor hallucis longus, but occasionally profound foot drop and weak ankle eversion are evident. Significant motor deficits and abnormal sphincter function should precipitate urgent radiological investigation, as prompt surgical intervention may be indicated.
Investigation
The goal of imaging is to demonstrate or exclude correlation of clinical and radiological abnormalities amenable to treatment. Plain radiographic imaging is of limited value, although often performed as an initial investigation. Such imaging can help in the assessment of stability and diagnosis of metastatic disease.
MR imaging is currently the modality of choice (Figure 2). If no abnormality is seen at L4/5 or L5/S1 the nerve roots should be scrutinised up to the conus medullaris to exclude unexpected lesions such as an ependymoma.
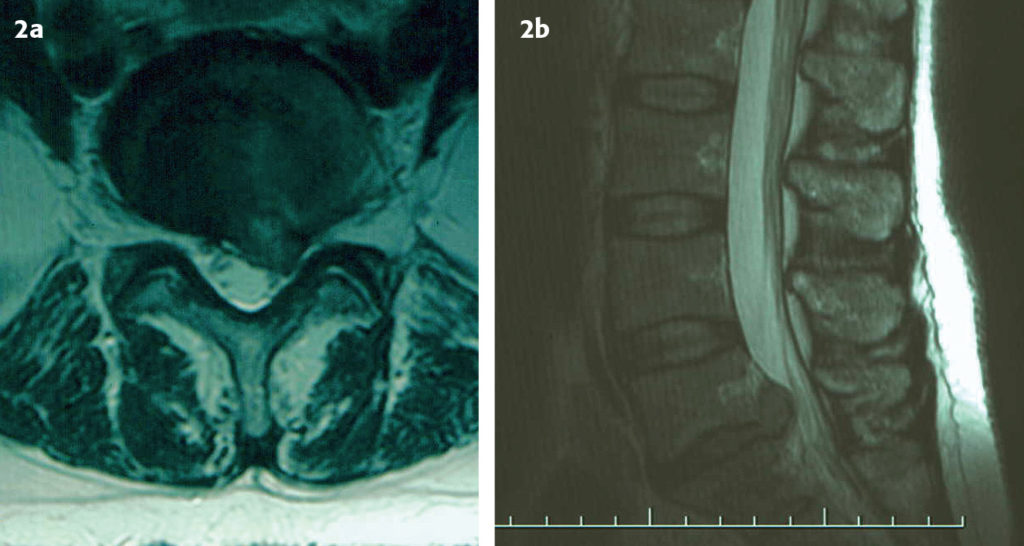
Figure 2b: Sagittal MRI scan showing compression of the cauda equina by a large central disc prolapse.
Treatment
The natural history of unilateral sciatic pain is of spontaneous resolution in 80% of patients without neurological sequelae, beginning within 1 – 2 months. A trial of conservative management should be undertaken initially and investigation is not recommended within this time period.
A proportion of patients will suffer recurrent or persistent symptoms; the latter often occurring after several spontaneously resolving episodes. It is for these patients that intervention should be considered.
During the period of conservative management a short period of bed rest is only recommended where pain prevents mobilisation and should precede recommencement of low impact aerobic exercise and activity modification. Physiotherapy advice and treatment benefits a proportion of patients [2].
The mainstays of oral analgesia are NSAIDs, with additional diazepam as an antispasmodic, as well as subsequent neuropathic modulators (gabapentin and amitriptyline) where necessary.
A proportion of patients pursue manipulative therapies successfully. However, spinal manipulation is sometimes associated with an acute exacerbation of symptoms.
Epidural injections of steroid and local anaesthetics appear to help some patients and a prospective, randomised, controlled, double-blinded study has shown the efficacy of selective nerve root blocks of patients with lumbar radiculopathy and/or stenosis [3].
Surgical treatment
Less than 2% of symptomatic patients undergo operative treatment. Surgical intervention is best directed at those with unremitting nerve root symptoms.
Urgent surgical intervention is required in those with acute cauda equina compression or significant acute motor deficit (e.g. foot drop). However, urgent decompression once urinary retention and overflow incontinence has occurred seems to confer little benefit [4[.
Microdiscectomy is the gold standard operative treatment for lumbar disc prolapse. The standard approach is through a midline incision over the affected interspace with intraoperative radiographs to confirm the operative level. A fenestration of the ligamentum flavum and, if indicated minimal laminotomy exposes the thecal sac and transiting nerve root. Medial retraction of the root permits identification of the disc space and prolapse and subsequent discectomy.
Central canal, lateral recess or foraminal stenosis from facet joint or ligamentum flavum hypertrophy are surgically decompressed by removal of the offending tissue whilst maintaining stability. There are various names and terms used for the numerous surgical procedures used to achieve this goal. Whilst such nomenclature adds to the apparent mystique of lumbar decompression it can be simplified. A laminectomy (removing the spinous process and bilateral lamina) and removal of the underlying ligamentum flavum, exposes and decompresses the cauda equina in the central thecal sac. Extension of bony removal to include up to 1/3 of the medial aspect of the facet joint (thus maintaining stability) will additionally expose and decompress the transiting nerve root in the lateral recess. Performed alone and unilaterally this latter decompression is often called a medial facetectomy. Where laminectomy is to be avoided (due to the need for multiple level decompression and concern regarding post operative stability) the central canal can be decompressed more specifically where it is most compromised (usually posterior to the intervertebral disc) by removing only part of the lamina at two adjacent levels. This is termed a bilateral laminotomy or an intersegmental decompression. Foraminal stenosis requires undercutting of the offending facet joint to the lateral limit of the exit foramen. Such undercutting is preferable to facetectomy and foraminotomy in terms of post-operative spinal stability [5].
Patients with spondylolisthesis are often asymptomatic, but the resultant loss of canal and foraminal diameter can both precipitate and accentuate symptoms of compression due to the other causes. Surgical treatment is based around decompression of the affected nerve roots. However, where instability is evident on standing flexion/extension plain lateral radiographs or anticipated, fusion may be undertaken.
Outcome and complications
Patients are discharged 24-48 hours post operatively and are advised to gradually return to normal activities, initially avoiding prolonged periods sitting and activities involving heavy lifting or repetitive mechanical stress. Most patients require only inpatient physiotherapy and advice, and do not need rehabilitation after discharge.
Patients are always made aware that surgery is intended to improve symptoms of leg pain, and prevent progression of symptoms of numbness and weakness. Neurological deficits may also improve. Anecdotally, discectomy rarely improves back pain, and can exacerbate it.
Nearly 80% of patients achieve relief from sciatica at 1 year [6]. However there is evidence that at 4 and 10 years after onset of symptoms there is no difference in groups treated operatively or conservatively [7]. Discectomy may therefore simply facilitate faster recovery. Lumbar decompression has been reported as equally successful in achieving significant pain relief and improvement in activities of daily living [8].
The risk of recurrent symptoms after microdiscectomy is reported between 5 and 12%, although the risk decreases with time post surgery [9].
Inadvertent durotomy (CSF leak) occasionally occurs but rarely causes long-term problems. It is frequently managed by a period of horizontal immobility (1-3 days) whilst the durotomy heals under reduced hydrostatic pressure. On occasion repeat surgery to achieve dural closure is necessary. The risk of neurological damage, either at the time of surgery or post operatively secondary to haematoma formation is usually quoted as less than 1%.
Destabilisation of the spine following microdiscectomy is very rare. Stability following laminectomy, facetectomy or intersegmental decompression is dependent on maintaining the integrity of the facet joints. Whilst there is some concern about the outcome after simple laminectomy there is recent evidence that it provides a good long-term outcome for 87% of patients with minimal complications [10].
References
- Frymoyer JW. Back pain and sciatica. N Engl J Med 1988;318:291-300. https://doi.org/10.1056/NEJM198802043180506
- Frost H, Lamb S, Doll H A et al. Randomised controlled trial of physiotherapy compared with advice for low back pain. BMJ 2004;329:708-11. https://doi.org/10.1136/bmj.38216.868808.7C
- Riew KD, Yin Y, Gibula L, et al. The effect of nerve-root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomized, controlled, double-blinded study. J Bone Joint Surg Am 2000;82:1589-93. https://doi.org/10.2106/00004623-200011000-00012
- Gleave JR, Macfarlane R. Cauda equina syndrome: what is the relationship between timing of surgery and outcome? Br J Neurosurg 2002;16(4):325-8. https://doi.org/10.1080/0268869021000032887
- Detweiler PW, Spetzler CB,Taylor SB, et al. Biochemical Comparison of facet-sparing laminectomy and Christmas tree laminectomy. J Neurosurg: Spine 2003;99:214-20. https://doi.org/10.3171/spi.2003.99.2.0214
- Tulberg T, Isacson J, Weidenhielm L. Does microscopic removal of lumbar disc herniation lead to better results than the standard procedure? Results of a one-year randomized study. J Neurosurg 1993;70:869-75. https://doi.org/10.1097/00007632-199301000-00005
- Weber H. Lumbar disc herniation. A controlled prospective study with ten years of observation. Spine 1989;14:431-7. https://doi.org/10.1097/00007632-198904000-00018
- Spengler DM. Degenerative stenosis of the lumbar spine. J Bone Joint Surg Am 1987;69A:305-8. https://doi.org/10.2106/00004623-198769020-00027
- Williams RW. Microdiscectomy: a twelve year statistical review. Spine 1986;11:851-2. https://doi.org/10.1097/00007632-198610000-00023
- Wilby MJ, Seeley H, Laing RJ. Laminectomy for Lumbar Canal Stenosis: Safe and Effective (abstract). Br J Neurosurg 2004 (in press).


