Most UK neurosurgeons treat 1-4 patients with an intracranial abscess each year. Intracranial abscesses can occur at any age. Contiguous spread to the intracranial cavity may occur directly or via emissary veins from infected paranasal sinuses, the middle ear and the mastoid. Such abscesses are usually located in the frontal or temporal lobes, or in the cerebellum. Haematogenous spread of infection can occur from the skin, dental sources and the lungs. Sixty percent of patients have a pre-disposing condition including an infective source (ear, sinus, teeth, lung), diabetes or an immunocompromised state. Patients with cyanotic heart disease are also at risk since circulating blood bypasses the pulmonary bacterial filter. Abscesses with a haematogenous origin are frequently located in the middle cerebral artery territory, presumably due to haemodynamic factors. Such abscesses are sometimes multiple.
Presentation
The clinical features in patients with an intracranial abscess evolve with time and depend upon the host pathogen interactions. From a brain perspective patients have one or more of the following clinical scenarios:
- Symptoms and signs of raised intracranial pressure (headache, impaired level of consciousness, slow mentation, nausea, vomiting, papilloedema).
- Focal neurological deficits due to compression of neuronal pathways (e.g. hemiplegia, dysphasia, frontal symptoms and signs, cerebellar syndrome).
- Seizures. These may by focal, Jacksonian or Grand Mal.
Constitutional symptoms and signs (pyrexia, rigors, dehydration, neck stiffness) and clinical features due to an infected source elsewhere in the body are surprisingly uncommon at the time of presentation.
Pathology
Britt and Enzmann described a canine model of Streptococcal abscess evolution with pathological phases that correlate with the clinical presentation in man [1]. An initial acute inflammatory cerebritis (days 1-9) is followed by hyperaemic capsule formation (days 10-14) and fibroblastic maturation (after day 14). Necrotic liquifaction and inflammatory exudate accumulate in the abscess cavity. During expansion of the abscess, the medial wall is usually thinner and less resistant and may result in ventriculitis. This is a poor prognostic indicator.
Microbiology
The majority of intracranial abscesses contain several mixed pathogens. In many patients, particularly those with sinus or ear infections a variety of aerobic and microaerophilic Streptococcal species are found (e.g. Strep millari; Strep pneumoniae, Strep pyogenes), often in combination with Haemophilus influenzae and Pseudomonas aeriginosa and anaerobes such as Bacteroides. In patients with a primary skin infection or an abscess complicating recent neurosurgery, Staphylococcus aureus is prevalent.
Investigations
Serial white blood cell counts, ESR and CRP levels provide useful parameters to monitor response to treatment – although not infrequently such investigations may be normal and can result in a delayed diagnosis. Blood cultures may help determine the likely pathogen. However, a CT or MRI scan of the brain +/- contrast secures the diagnosis and should always be performed before a lumbar puncture is considered. An abscess appears as a ring-enhancing, space demanding process. The ring of enhancement is usually quite linear without the heterogeneous appearances characteristic of a malignant glioma. The most frequent abscess locations are frontal, temporal or cerebellar. They are usually sub-cortical, but small abscesses may abut the grey-white matter interface in the middle cerebral artery territory. A CT or MRI scan may also reveal an infected source such as a paranasal sinus infection or an ear infection. The diagnosis is confirmed by examination of pus obtained directly from the abscess. Once an abscess has been identified, broad-spectrum antibiotics should be commenced and urgent neurosurgical referral made.
Surgical Options
Surgery is required to obtain pus from a solitary abscess. Sometimes this is non-diagnostic particularly if antibiotics have been administered. Surgery also reduces the bulk of an abscess providing symptomatic relief and minimising the risks of abscess growth (intraventricular rupture, herniation, venous sinus thrombosis). The surgical options include aspiration, craniotomy and complete excision or craniotomy and marsupialisation. Aspiration Image guided (CT or MRI) frameless stereotactic aspiration has recently become the most commonly utilised surgical technique to treat an abscess. For small and deep abscesses (< 2cm) a stereotactic frame increases the accuracy of the localisation technique. In patients with multiple abscesses, the largest lesion is usually aspirated and other lesions monitored with post-operative imaging [2,3].
Craniotomy
A craniotomy can be performed as a primary procedure or if abscess re-growth occurs after initial aspiration. In the majority of patients brain swelling is prominent and mannitol should be administered intraoperatively to minimise this problem. If the abscess is located in non-eloquent brain the abscess wall is dissected from the surrounding brain permitting enucleation of the lesion. If the abscess is in an eloquent region a trans-cortical approach can be made through a 2 cm incision. An intersulcal approach shortens the distance to the lesion compared with the more traditional transgyral corticotomy. The operative microscope is used to visualise and preserve cortical vessels within the sulcus. The abscess wall is then encountered and opened widely (marsupialisation) to permit complete aspiration of all pus (Figure 1a). The cavity is thoroughly irrigated with saline (some surgeons use a dilute solution of hydrogen peroxide). The use of haemostatic matrices (e.g. Surgicel) is limited to avoid colonisation of such materials. Following evacuation or open drainage the brain swelling has usually improved considerably permitting replacement of the bone flap during closure.

Peri-Operative Care
Several factors need to be addressed. These include the choice and duration of antibiotic treatments, the role of surveillance imaging, the treatment of any primary focus, the use of steroids and the use of prophylactic anticonvulsants.
Antibiotic Treatment
The choice of antibiotics is governed by several factors including the appearances on an initial Gram stain, the potential for mixed aerobic and anaerobic pathogens, and antibiotic penetration. Expert microbiological advice is invaluable when selecting antimicrobials. For the majority of primary abscesses initial intravenous treatment with a third generation cephalosporin and metronidazole is appropriate. Cultures may subsequently refine the choice of antibiotics.
Some antibiotics can be safely instilled during surgery (e.g. Gentamicin 10mg), but direct instillation of penicillin is unsafe and can cause seizures. The duration of antibiotic treatment is controversial. If antibiotics are administered for a short period (e.g. 2 weeks) there does appear to be an increased risk of recurrence. Provided surveillance imaging is satisfactory a 4-week course of intravenous antibiotics, supplemented by a further 2 weeks of oral treatment is recommended.
Surveillance Imaging
MRI is preferred to CT scanning to abolish the risks of radiation exposure. A post-operative MRI scan performed within 48 hours of surgery serves as a useful baseline for subsequent imaging. Provided the patient remains stable, repeating the scan at weekly intervals for 2 weeks and then at fortnightly intervals for a further 1-month enables reaccumulation of the abscess to be detected at a pre-clinical phase (Figures 1b, 1c).
Treatment of Primary Focus
To minimise the risk of recurrent or non-responsive intracranial infection any identifiable primary source requires aggressive treatment [4]. This may include surgery for paranasal, middle ear or dental sepsis, physiotherapy and antibiotics for pulmonary infection and surveillance echocardigrams in patients with a cardiac source. The timing of such interventions does not need to coincide with intracranial surgery but should be undertaken in an expert, timely fashion.
Steroid Therapy
In general, steroids are not used in brain abscess patients due to the immunosuppression associated with these drugs. However, extensive oedema may surround the abscess and contribute to raised intracranial pressure. In a deteriorating clinical situation steroids can improve the clinical status of patients when there appear to be few options remaining. This is probably due to a reduction in the inflammatory process reducing concomitant oedema.
Prophylactic Anticonvulsants
Between 40-50% of patients who suffer from an intracranial abscess will develop epilepsy. Prophylactic anticonvulsants should therefore be seriously considered. Patients should contact the DVLA and refrain from driving.
Prognosis
In the pre-CT era the mortality of cerebral abscesses was in the region of 30-40%. CT scanning and improved localisation techniques have reduced this to less than 5%. The use of modern treatment regimes with image-directed neurosurgery may reduce this further. Risk factors for a poor outcome include deep-seated location, intraventricular abscess rupture causing ventriculitis and a poor neurological status [5]. Many patients with a neurological deficit achieve significant recovery during the rehabilitative phase of care.
Rare Intracranial Infections
Subdural empyema and extradural abscesses
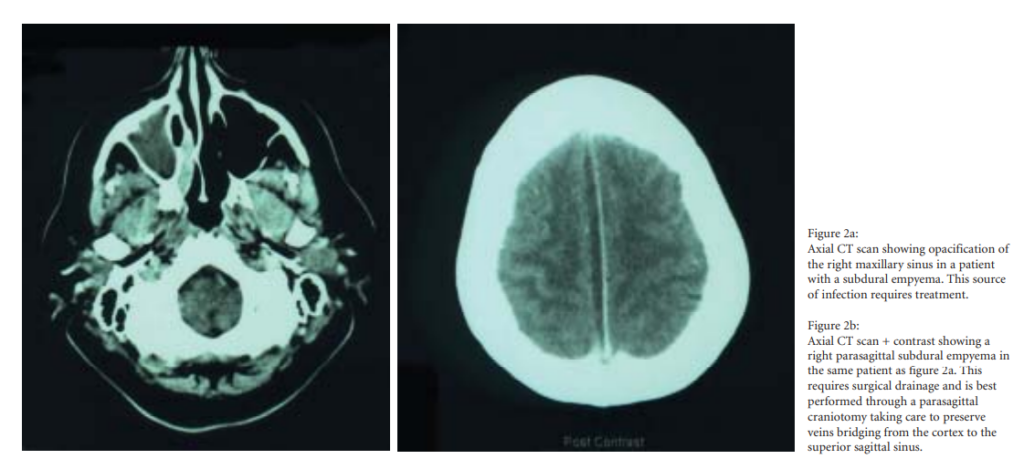
These are both rare. They are usually associated with contiguous otological or sinus pathology and are identified on CT scans (Figure 2a). While extradural abscesses are readily detected, subdural empyemas typically have a subtle appearance on CT scans (Figure 2b). They are characterised by a relatively thin, low attenuation mass with minimal enhancement associated with a profound clinical picture (impaired level of consciousness, neurological deficit and fits). Symptoms and signs of infection may not be present. Early aggressive surgery targeted at the intracranial mass and any source of infection is recommended. A craniotomy is the preferred option for an empyema due to the viscous nature of the pus that is not readily washed out of the subdural space. Indeed, a fibrinous layer of tissue usually adheres to the arachnoid and is best left undisturbed after thorough irrigation under direct vision. The risk of a neurological deficit and epilepsy in patients with a subdural empyema exceeds 60%, probably due to multiple small cortical venous infarctions [6].
Tuberculosis
TB remains common in the Indian sub-continent and cases of intracranial TB are seen in the UK. Symptoms of raised ICP and/or epilepsy should lead to the suspicion of a tuberculoma. This is a calcified parenchymal lesion with central caeseating necrosis. TB only rarely causes a typical brain abscess appearance. Treatment options depend on the clinical status of the patient and lie between clinical surveillance, empirical anti-tuberculous treatment with follow-up scans, image-guided aspiration combined with medical treatment and rarely surgical excision.
Neurocysticercosis
This disease is endemic in most developing parts of the world. The larvae of this ingested intestinal tapeworm hatch from eggs in the intestine and migrate to a variety of tissues including brain parenchyma, muscles, subcutaneous tissues and the eye. In many cases the host immune system eliminates the parasite expeditiously. However, CT and MRI indicate that small-calcified parenchymal cystic lesions can persist. These may be multiple and may contain a mural “scolex” of larvae. Neurocysticercosis may be asymptomatic, cause epilepsy or result in a focal neurological deficit. Management is directed at seizure control [7]. Empirical treatment with the anti-helminthic agents albendazole or praziquantel is not mandatory in the late “burnt-out” phase of the disease. Surgery is only required if seizures are not controlled medically or in rare instances when space occupation is problematic.
Summary
Although the incidence of intracranial abscesses has decreased over the past 100 years the surgical principles expostulated by MacEwen in 1881, namely debridement and drainage, remain of paramount importance. Advances in neuronavigation techniques make stereotactic drainage a simple procedure that can be performed expeditiously for the majority of abscesses. The appropriate use of effective antibiotic therapy adds to the therapeutic armamentarium. Surveillance imaging with MRI scans is now the follow-up modality of choice. These changes in management have seen a significant reduction in the mortality of brain abscesses in the last 20 years.
References
- Britt RH, Enzmann DR. Clinical stages of human brain abscesses on serial CT scans after contrast infusion. J.Neurosurg. 1983;59:972-989. https://doi.org/10.3171/jns.1983.59.6.0972
- Boviatsis EJ, Kouyialis AT, Stranjalis G, Korfias S, Sakas DE. CT-guided stereotactic aspiration of brain abscesses. Neurosurgical Review. 2003;26:206-209.
- Barlas O, Sencer A, Erkan K, Eraksoy H, Sencer S, Bayindir C. Stereotactic surgery in the management of brain abscess. Surgical Neurology. 1999;52:404-410.https://doi.org/10.1016/S0090-3019(99)00118-4
- Sennaroglu L, Sozeri B. Otogenic brain abscess: review of 41 cases. Otolaryngology – Head and Neck Surgery. 2000;123:751-755. https://doi.org/10.1067/mhn.2000.107887
- Takechita M, Kagawa M, Izawa M, Takakura K. Current treatment strategies and factors influencing outcome in patients with bacterial brain abscess. Acta Neurochirurgica 1998;140:1263-1270. https://doi.org/10.1007/s007010050248
- Cowie R, Williams B. Late seizures and morbidity after subdural empyema. J.Neurosurg. 1983;58:569-573. https://doi.org/10.3171/jns.1983.58.4.0569
- Sotelo J. Neurocysticersosis. Br Med J 2003;326:511-512. https://doi.org/10.1136/bmj.326.7388.511
