Abstract
Vitamin B12 is an essential enzymatic cofactor in multiple cellular metabolic pathways. Deficiency states can arise as a result of both depletion of absolute systemic levels and pathological processes that block its ability to act as an enzymatic cofactor. The latter is also known as functional vitamin B12 deficiency. This can cause a variety of systemic, haematological, and neurological manifestations, some of which may be irreversible if not promptly treated. Neurological syndromes include subacute combined degeneration of the cord (SCDC), peripheral, optic, and autonomic neuropathies, and neuropsychiatric or cognitive deficits. This review presents a case series of vitamin B12 deficiencies leading to SCDC, and we include the clinical features, significant investigations, treatments, and prognoses.
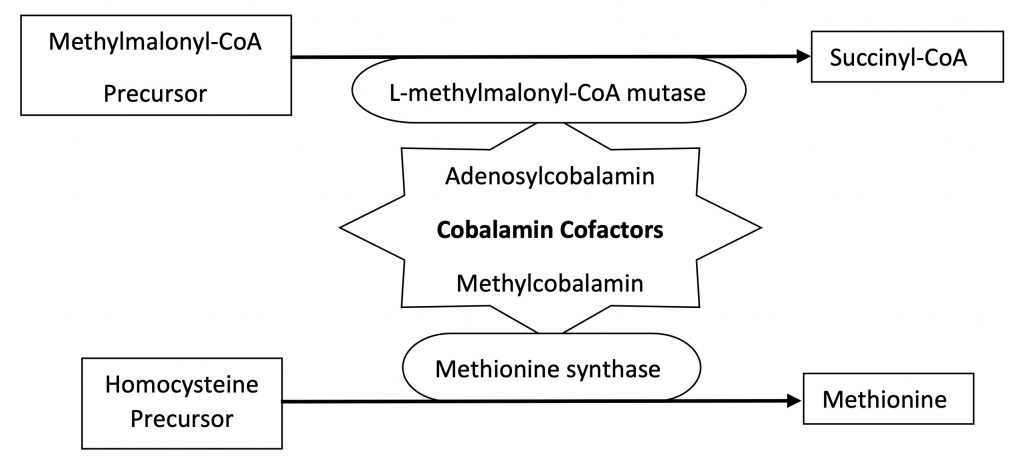
Vitamin B12 is the term for a group of structurally similar chemicals called ‘cobalamins’. The two most important biological cobalamin forms in humans are methyl-cobalamin and adenosyl-cobalamin. Methylcobalamin is a cofactor for the enzyme methionine synthetase, which converts homocysteine to methionine. Methionine can then be activated to S-adenosylmethionine which is important for myelin lipid synthesis and DNA methylation [1,2]. Adenosylcobalamin is essential for the enzyme L-methylmalonyl-CoA mutase in mitochondria. This converts L-methylmalonyl-CoA to succinyl-CoA, important for the metabolism of amino acids and fatty acids. A schematic diagram of the metabolic pathway is shown in Figure 1. Note that the precursor molecules of methylmalonic acid (MMA) and homocysteine are now available for testing. Their build up is suggestive of metabolic block at the cobalamin utilisation step and could indicate both a quantitative and qualitative deficit.
Most of the human vitamin B12 stores come from dietary sources. Vitamin B12 absorption is complex and is dependent on a series of ‘carrier’ molecules throughout the digestive system. The process begins in the oral cavity where haptocorrin, also known as R-binders, found in saliva, complexes with vitamin B12. Subsequently in the stomach, gastric parietal cells secrete intrinsic factor which binds to vitamin B12 and help its transport to and absorption from the terminal ileum. Interruptions at any point along this pathway could lead to B12 deficiency (Table 1).
Table 1. Causes of B12 deficiency along its metabolic pathway. | |
Metabolic pathway | Causes of deficiency |
Dietary intake (animal proteins, supplements) | Malnutrition (alcoholism, eating disorders) |
Gastric acid and pancreatic enzymes release B12 from food proteins | Malabsorption (Achlorhydria, atrophic gastritis, gastrectomy/bariatric surgery, drugs, coeliac disease) |
B12 binds to HC (stomach) | |
Proteases release HC/B12 complex (duodenum) | |
B12 attaches to IF, and the B12/IF complex binds to the receptor cubilin to be internalised (terminal ileum) | Pernicious anaemia |
B12 is detached from IF and binds to TCII (circulation) | |
Intracellular uptake of B12/TCII complex via TCII receptor | |
Intracellular action of lysosomes free B12 from TCII | |
B12 utilised for production of methionine (cytosol) and succinyl-A (mitochondria) | N2O toxicity
|
HC, Haptocorrin; GI, Gastrointestinal; IF, Intrinsic factor; TCII, Transcobalamin II; N2O, Nitrous oxide.
| |
One of the best-studied causes is pernicious anaemia, an immune-mediated process against the gastric parietal cells responsible for producing intrinsic factor (IF). Deficiency due to decreased dietary intake is uncommon in developed nations. However, those with gastrointestinal conditions, dietary restrictions, and/or polypharmacy can be at risk. Some commonly used drugs such as proton pump inhibitors, metformin, contraceptives and hormonal replacement therapies can cause malabsorption of vitamin B12 [3,4,5]. In contrast, functional B12 deficiency is caused by qualitative deficits in its ability to function as enzymatic cofactors. The inhaled anaesthetic agent Nitrous Oxide (N2O) is one such example. Awareness of N2O and its neurological complications has increased in recent years due to its use as a recreational drug. N2O interferes with the action of the central cobalt atom in B12 and inactivates methylcobalamin, thus blocking intracellular enzymic reactions [6,7].
Clinical features: subacute combined degeneration of the cord
Regardless of the mechanism of vitamin B12 deficiency, the neurological system is particularly vulnerable to deficiency states. In fact, a significant proportion of cases seem to present with only neurological syndromes, and available data support the division of neurological and haematological abnormalities [1,2]. One of the most recognised presentations is subacute combined degeneration of the spinal cord (SCDC). Pathologically, SCDC refers to the selective, but combined degeneration of the dorsal column and corticospinal white matter tracts. SCDC typically presents with sensory ataxia, with or without spastic paraparesis or a sensory level [1, 6]. Deep tendon reflexes (DTR) can be brisk or diminished [7]. B12 deficiency is thought to lead to demyelination of the dorsal columns, although the causative mechanism is not well understood [9].
Other neurological complications of Vitamin B12 deficiency
Vitamin B12 deficiency can also present with a symmetrical, sensorimotor neuropathy, which is typically axonal. However, cases of demyelinating neuropathy have been reported [11,12], manifesting similarly to Guillain Barré Syndrome (GBS). Overlap syndromes of myeloneuropathy manifesting with absent DTR and extensor Babinski’s reflexes are also well recognised.
Optic neuropathy or atrophy has also been reported, but this is less common compared to peripheral neuropathy or myelopathy [1]. Involvement of the autonomic nervous system is possible, usually presenting with urinary/bowel incontinence or erectile dysfunction [8].
Cognitive impairment and neurobehavioral changes have been observed mainly in the elderly. The cognitive decline can be fast, and improvement is expected with replacement therapy [13]. MRI of the brain can reveal subcortical hyperintensities on T2 weighted images, as well as cortical atrophy [13]. However, these findings are not specific to B12 deficiency and co-morbidities of each individual should be taken into consideration.
Diagnosis
There is increasing availability of testing for serum vitamin B12, homocysteine, and methylmalonic acid levels. Serum vitamin B12 levels can provide an indication of absolute body stores. However, a normal B12 level with elevated homocysteine and methylmalonic levels can still be indicative of a functional B12 deficiency with qualitative deficits in vitamin B12 utilisation.
Treatment
Early replacement of vitamin B12 is essential to avoid prolonged neurological symptoms or incomplete recovery. Intramuscular hydroxocobalamin is recommended at a dose of 1mg on alternate days, usually for up to two weeks. In cases of severe neurological disease, the duration of treatment can be prolonged and the BNF suggests continuation of intensive replacement therapy until no further neurological improvement is seen [15]. Maintenance therapy with intramuscular hydroxocobalamin 1mg every 2 months should then be offered.
Oral replacement therapy could be considered in cases of dietary deficiency, however current guidelines support the use of intramuscular replacement in all cases presenting with neurological complications [2,15,16]. In cases of N2O toxicity, avoidance of further exposure from recreational or medicinal sources is as important as the replacement therapy. Patients with concurrent anaemia can develop hypokalaemia during vitamin B12 treatment and potassium replacement might be needed in such cases [16].
Case 1
A 27-year-old man presented with four weeks of progressive distal paraesthesia affecting both feet and hands. Clinical examination revealed ataxic gait, reduced tone and DTR in the upper limbs but brisk DTR in the lower limbs. Babinski’s response was negative. Vibration and joint position senses were reduced at the ankles with intact pain and temperatures sensations, and no sensory level. Power was normal.
On review of the drugs history, he admitted to daily use of N2O inhalation for recreational purposes over the preceding 6 months.
Investigations revealed low serum B12 at 148ng/L (187-883), with high levels of MMA at 2978nmol/L (0-360), and homocysteine >125μmol/L (6.7-15.2). MRI of the whole spine showed a longitudinally extensive T2 high signal change from the cervico-medullary junction to T10-11 level, affecting the dorsal columns (Figure 2, images A1 and A2).
A diagnosis of SCDC due to B12 deficiency was made based on clinical, laboratory and radiological findings. He was treated with intramuscular injections of hydroxocobalamin 1mg on alternate days for 2 months. At the current time of follow up there have been some improvements in gait but there continues to be distal paraesthesia in all limbs.
Case 2
A 67-year-old man presented with subacute progressive distal paraesthesia in all limbs and decline in mobility. He has a history of gastric adenocarcinoma treated with partial gastrectomy and chemotherapy. Examination revealed an ataxic gait, with normal tone and power. DTR were present in the upper limbs and brisk in the lower limbs, with normal Babinski’s reflex. Joint position and vibration senses were reduced to the ankles, with no sensory level and preserved pain and temperature sensations.
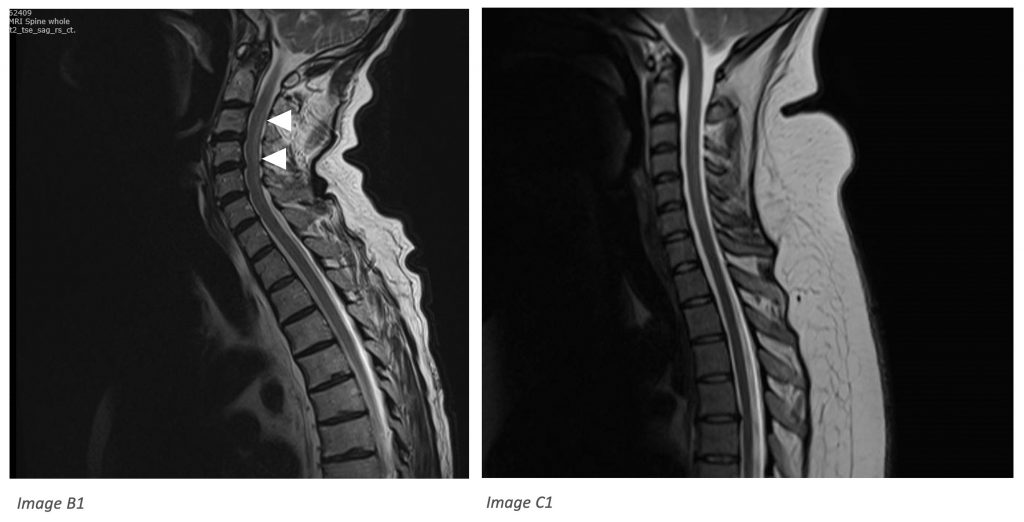
B12 was normal at 301ng/L, but there was increased homocysteine (15μmol/L) and MMA (1578nmol/L). MRI of the whole spine showed high T2 signal in the dorsal cervical spinal cord extending from the cervico-medullary junction to C6 level, in keeping with SCDC (Figure 2, image B1).
He was treated with intramuscular injections of hydroxocobalamin 1mg on alternate days for 2 months, with improvement of his mobility from wheelchair bound to walking with a stick.
Case 3
A 27-year-old female with Ehlers Danlos syndrome presented with two-months’ history of distal paraesthesia in both hands, followed by paraesthesia ascending from toes to the umbilicus. On review of the history, she had frequent Emergency Department attendances for shoulder dislocation requiring reduction at least weekly in the last year. On each occasion she used Entonox (50% N2O, 50% oxygen) as an inhalational analgesic for up to 30 minutes.
Examination revealed sensory ataxia, a sensory level to T8, reduced vibration and joint position sense to the ankles, DTR brisk at ankles, and positive Babinski’s reflex bilaterally. Tone and power were normal.
MRI of the whole spine was unremarkable (Figure 2, image C1) and the B12 level was actually elevated at >2000. However, plasma MMA was significantly elevated at 2722nmol/L, as well as homocysteine at 31μmol/L. Functional B12 deficiency was diagnosed based on history, examination and laboratory findings. She was treated with intramuscular hydroxocobalamin 1mg on alternate days for two weeks. Follow up is pending.

Case 1, Image A1: SCDC has a typical radiological appearance of a longitudinal segment of increased signal on T2-weighted images, usually extending from the cervical to the thoracic cord (arrowheads). Contrast enhancement is not usually found [6,7].
Case 1, Image A2: Axial T2 images show increased signal in the posterior columns, known as the “inverted V sign’’ (arrow) [6,9].
Case 2, Image B1: similar dorsal column T2 signal changes extending from cervico-medullary junction to C6 (arrowheads).
Case 3, Image C1: relatively unremarkable appearing T2 weighted imaging of cervical spine in case of biochemically confirmed functional B12 deficiency.
Key learning points
- Case 1 demonstrated that SCDC often has a typical radiological appearance of a longitudinal segment of increased signal on T2-weighted images, usually extending from the cervical to the thoracic cord (Figure 2 images A1, B1). Contrast enhancement is not common [6,7]. Axial T2 images show increased signal in the posterior columns, known as the ‘inverted V sign’ (Figure 2, image A2) [6,9].
- However, the extent and severity of MRI changes are not indicative of disease severity [10]. Case 3 also demonstrated that some cases of SCDC can have normal MR imaging (Figure 2, image C1). In cases where there is negative imaging investigation, but the clinical suspicion remains strong for SCDC then biochemical tests should be performed.
- Cases 2 and 3 demonstrated that normal or high levels of serum B12 do not necessarily mean efficient utilisation of B12 at a cellular level. Functional B12 deficiencies can also produce similar pathologies and symptoms. Measurements of MMA and homocysteine levels in all suspected patients is recommended. Levels should generally be measured before B12 replacements as this could potentially produce false negative results. However, once blood tests have been sent there is no need to wait for results before commencing empirical treatments if the clinical suspicion is high.
- Recreational N2O use is increasingly recognised as a cause for functional B12 deficiency and SCDC. It is important to remember that patients may not offer the history of N2O as it is a drug of abuse.
- Clinicians may forget that N2O is frequently used in anaesthetic medicine and iatrogenic exposure needs to be investigated carefully where clinical suspicion is high for a functional B12 deficiency.
References
- Reynolds E. Vitamin B12, folic acid, and the nervous system. Lancet Neurology 2006;5:949-960. https://doi.org/10.1016/S1474-4422(06)70598-1
- Wolffenbuttel BHR, Wouters HJCM, Heiner-Fokkema MR, Van der Klauw MM. The many faces of cobalamin (vitamin B12) deficiency. Mayo Clinic Proceedings, 2019;3(2):200-214. https://doi.org/10.1016/j.mayocpiqo.2019.03.002
- Shipton MJ, Thachil J. Vitamin B12 – A 21st century perspective. Clinical Medicine 2015;15(2):145-150. https://doi.org/10.7861/clinmedicine.15-2-145
- Kumar N. Nutrients and Neurology. Continuum 2017;23(3):822-861. https://doi.org/10.1212/01.CON.0000520630.69195.90
- Juhasz-Poscine K, Rudnicki SA, Archer RL, Harik AI. Neurologic complications of gastric bypass surgery for morbid obesity. Neurology 2007;68(21):1843-1850.https://doi.org/10.1212/01.wnl.0000262768.40174.33
- Ramalho J, Nunes RH, Da Rocha AJ, Castillo M. Toxic and metabolic myelopathies. Seminars in Ultrasound, CT and MRI 2016;37:448-465. https://doi.org/10.1053/j.sult.2016.05.010
- Keddie S, Adams A, Kelso ARC, Turner B, Schmierer K, Gnanapavan S, Malaspina A, Giovannoni G, Basnett I, Noyce A. No laughing matter: subacute degeneration of the spinal cord due to nitrous oxide inhalation. Journal of Neurology 2018;265:1089-1095. https://doi.org/10.1007/s00415-018-8801-3
- Patel KK, Munne JCM, Gunness VRN, Hersey D, Alshafai N, Sciubba D, Nasser R, Gimbel D, Cheng J, Nouri A. Subacute combined degeneration of the spinal cord, following nitrous oxide anaesthesia: A systematic review of cases. Clinical Neurology and Neurosurgery, 2018;173:163-168. https://doi.org/10.1016/j.clineuro.2018.08.016
- Xiao CP, Ren CP, Cheng JL, Zhang Y, Li Y, Li BB, Fam YZ. Conventional MRI for the diagnosis of subacute combined degeneration of the spinal cord due to vitamin B12 deficiency. Asia Pac J Clin Nutr 2016;25(1):34-38.
- Li J, Ren M, Dong A, Wu Y, Han N, Deng B, Bi X. A retrospective study of 23 cases with subacute combined degeneration. International Journal of Neuroscience 2016;126(10):872-877. https://doi.org/10.3109/00207454.2015.1077331
- Thompson AG, Leite MI, Lunn MP, Bennett DLH. Whippits, nitrous oxide and the dangers of legal highs. Practical Neurology 2015;15:207-209. https://doi.org/10.1136/practneurol-2014-001071
- Kalita J, Chandra S, Bhoi SK, Misra UK, Shankar SK, Mahadevan A. Clinical, nerve conduction and nerve biopsy study in vitamin B12 deficiency neurological syndrome with a short-term follow-up. Nutritional Neuroscience 2014;17(4):156-163. https://doi.org/10.1179/1476830513Y.0000000073
- Kalita J, Misra UK. Vitamin B12 deficiency neurological syndromes: correlation of clinical, MRI and cognitive evoked potential. Journal of Neurology 2008;255:353-9. https://doi.org/10.1007/s00415-008-0660-x
- Cao J, Xu S, Liu C. Is serum vitamin B12 decrease a necessity for the diagnosis of subacute combined degeneration? A meta- analysis. Medicine 2020;99:14. https://doi.org/10.1097/MD.0000000000019700
- Joint Formulary Committee. British National Formulary (online) London: BMJ Group and Pharmaceutical Press. {http://www.medicinescomplete.com} [Accessed on 10/10/2021].
- Devalia V, Hamilton MS, Molloy M. Guidelines for the diagnosis and treatment of cobalamin and folate disorders. British Journal of haematology 2014; 166: 496-513. https://doi.org/10.1111/bjh.12959

