Introduction
Impulse control disorders are pathological behaviours characterised by the inability to inhibit the urge to commit acts that are harmful to ones’ self or to others.1 Intermittent explosive behaviour, compulsive gambling, pyromania, trichotillomania and kleptomania are the main examples of these behaviours. There are large variations in the incidence of the different impulse control disorders after brain injury. For example, >80% of patients with this pathology have intermittent explosive disorder.2 By contrast, only a few cases of post brain injury kleptomania have been reported to date and these occurred in patients with pre-existing psychiatric disorders. For example, Talih3 reported worsening of pre-existing kleptomania in a patient after she had traumatic brain injury. Following concussion she committed the theft almost daily compared to once every three or four weeks before the accident. Similar worsening of kleptomania after brain injury was also reported in two other patients with mental illness.4 Kleptomania occurring without previous psychiatric co-morbidity has been reported in patients with dementia5 and following resection of a brain tumour.6 We report here a case of kleptomania occurring for the first time after hypoxic brain injury in a patient with no history of mental illness or substance or alcohol abuse. Analysis of this case suggests significant differences between kleptomania occurring de novo after acquired brain injury and kleptomania associated with psychiatric illness.
Case report
A 55-year-old man with no significant past medical or family history was admitted to hospital following out-of-hospital cardiac arrest secondary to ventricular fibrillation. There was no cardiac output for 10 minutes. His blood circulation was restored after three cardiac defibrillation attempts. He then underwent therapeutic hypothermia and mechanical ventilation. When weaned off the ventilator on the fourth day post-cardiac arrest he was confused and disorientated. These symptoms continued until he was transferred to our unit eight weeks after his initial presentation. On admission to our ward the general physical examination of the patient was entirely normal. On neurological examination there was no focal neurological deficit. The bedside assessment confirmed that the patient was orientated in time, place and person. His mood appeared normal. However, there was evidence of mild to moderately severe cognitive impairment, as summarised below. A CT head scan was normal. A full blood count, renal and liver function tests were also within the normal range. Cardiac investigations confirmed significant stenosis of the coronary arteries.
The patient’s behaviour on the ward was normal except that he repeatedly stole objects from the dining room and from the bedside lockers of other patients and hid them. The objects included cutlery, cleaning products, television remote control sets, etc. When asked by the ward staff to return the stolen items he often apologised and gave them back explaining that he only took “things that other people no longer needed”. However, on other occasions he denied the theft. He did not report any sense of tension or excitement before, or a sense of relief or gratification after the theft. Nor did he feel guilt or shame as a result of his actions. No specific therapy intervention was given except to explain repeatedly to the patient that the stolen objects did not belong to him. The kleptomania lasted for about six weeks and resolved spontaneously.
Details of the neuropsychological assessment
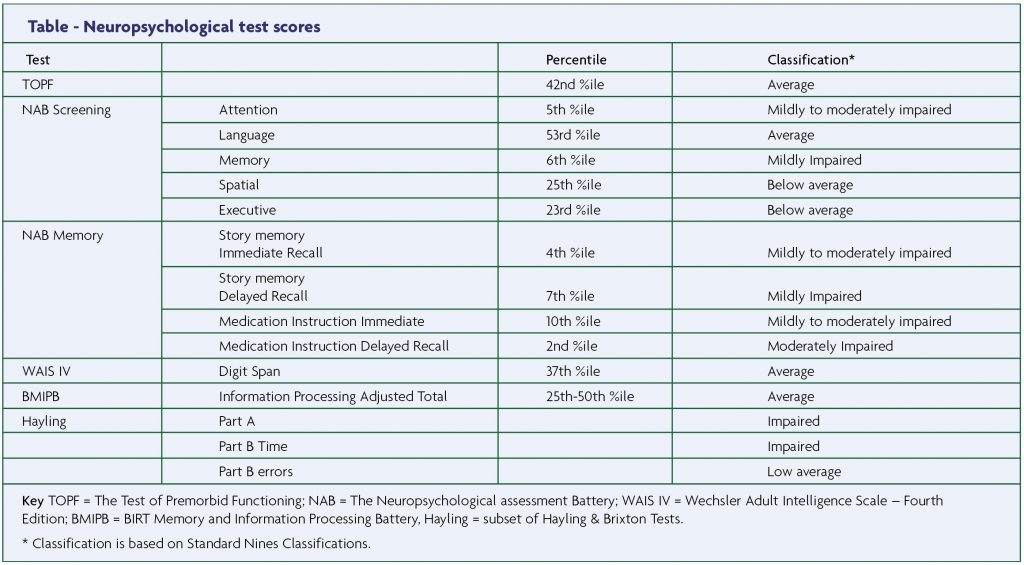
The patient’s premorbid IQ was assessed with the Test of Premorbid Functioning.7 Attention, language, memory, spatial and executive functioning were assessed with the relevant sections of the Neuropsychological Assessment Battery.8 To further assess the patient’s executive function subsets from the Behavioural Assessment of the Dysexecutive Syndrome,9 Hayling and Brixton Test,10 the Wechsler Adult Intelligence Scale (WAIS IV)11 and BIRT Memory and Information Processing Battery12 were used. In order to diagnose and assess the severity of compulsive-obsessive behaviour the Yale-Brown obsessive-compulsive scale13 was administered.
The patient’s pre-morbid IQ was estimated to be in the average range of ability which seems to be commensurate with his previous level of functioning, e.g. employment history and leisure time interests. Overall, he scored within the mildly to moderately impaired range for the attention domain. His information processing speed, working memory and some executive functions were reasonably preserved with only occasional subtle deficits. The patient’s score on the Yale-Brown scale was zero which indicates the absence of a obsessive- compulsive disorder. Results from the neuropsychological screening are summarised in the table.
Functional assessment
An occupational therapy assessment was carried out to assess the patient’s performance in real life situations. The patient was completely independent with basic activities of daily living. His safety judgement outdoors was good. However, his slow cognitive processing was evident as he took a relatively long time to make decisions. Repeated assessments did not suggest evidence of impulsivity or risk-taking behaviour.
Discussion
The clinical presentation of the patient reported here is consistent with hypoxic brain injury. A normal CT head scan does not exclude this diagnosis as abnormalities on CT are found in less than 12% of these patients.14 The patient fulfilled the diagnostic criteria of kleptomania.1 He stole objects that had no value to him and he frequently acknowledged that he committed the theft. His actions had no clear motives and could not be explained by antisocial behaviour or mental illness. However, the clinical features of kleptomania in this patient are different in some ways from those observed in patients with psychiatric co-morbidity.
In contrast to the previously reported cases of post-brain injury kleptomania, our patient did not have the conditions that are usually associated with this disorder, such as a history of pre-existing depressive illness, hypomania, alcohol or substance abuse or treatment with selective serotonin reuptake inhibitors.15 Furthermore, there was no evidence of obsessivecompulsive behaviour in our patient whereas such behaviour would be expected in more than 60% of cases when kleptomania is associated with mental illness.16
The phenomenology and course of symptoms in the patient reported here are also different from those reported in psychiatric patients. Significantly, the patient did not report a sense of irresistible urge to steal or gratification or relief that is usually followed by a sense of guilt after the theft was committed. These are core features of kleptomania in psychiatric patients. In addition, on some occasions he denied the theft which could be due poor short term memory.17 On other occasions the patient offered rationalisations to justify the theft by saying that he took things “that other people no longer needed”. In addition, the typical course of kleptomania in those with mental illness is that the theft is repeated over a long period of time and usually does not stop without therapy interventions. This contrasts with the short course and spontaneous recovery in our patient.
The reasons for the above-reported differences in the phenomenology of kleptomania in our patient and that in psychiatric patients is not clear. A possible explanation is the severity and extent of the lesion. Extensive damage to the fronto-orbital lobes and the caudate nucleus and disruption of dopaminergic neurotransmission have been demonstrated in cases of persistent ICDs18,19 and the location and extent of damage to these structures appear to correlate with antisocial behaviour, decision-making deficits and risk-taking.20 The mild and transient cognitive deficits in our patient and the normal CT head scan suggest limited brain damage. Further observations are required to elucidate the aetio-pathogenesis of kleptomania following brain injury.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC, 2013.
- Kessler RC, Coccaro EF, Fava M, Jaeger S, Jin R, Walters E. The prevalence and correlates of DSM-IV intermittent explosive disorder in the National Comorbidity Survey Replication. Archives of General Psychiatry 2006;63:669-78.
- Talih FR. Kleptomania and potential exacerbating factors: A review and case report.Innovation in Clinical Neuroscience 2011;8:35-9.
- Aizer A, Lowengrub K, Dannon PN. Kleptomania after head trauma: two case reports and combination treatment strategies. Clinical Neuropharmacology. 2004;27:211-15.
- Mendez MF. Pathological stealing in dementia. Journal of the American Geriatrics Society 1988;36:825-6.
- Nyffler T, Regard M. Kleptomania in a patient with fronto-limbic lesion. Neuropsychiatry Neuropsychology & Behavioural Neurology 2001;14:73-6.
- Wechsler D. Test of Premorbid Functioning. San Antonio, TX: The Psychological Corporation; 2009
- Stern RA, White T. Neuropsychological Assessment Battery: Administration, Scoring, and Interpretation Manual. Lutz, Fla: Psychological Assessment Resources, Inc., 2003
- Wilson BA, Alderman N, Burgess PW, Emslie H, Evans JJ. Behavioural Assessment of the Dysexecutive Syndrome. Bury St. Edmunds, England: Thames Valley test Company, 1996
- Burgess P, Shallice T. The Hayling and Brixton Tests. Test manual. Bury St Edmunds, UK: Thames Valley Test Company, 1997
- The Psychological Corporation.WAIS-IV. WMSIV Technical Manual. San Antonio, TX, 2008
- Coughlan AK, Oddy M, & Crawford JR. BIRT Memory and Information Processing Battery. The Brain Injury Rehabilitation Trust, 2007
- Goodman WK, Price LH, ,Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-Brown obsessive compulsive scale. I. Development, use, and reliability. Archives of General Psychiatry 1989;46:1006-111.
- Cocchi NM, Lucas JM, Salciccioli J, Carney E, Herman S, Zimetbaum P, et al. The role of cranial computed tomography in the immediate post-cardiac arrest period. Internal & Emergency Medicine 2010;5:533-8.
- McElroy SL, Pope HG Jr, Hudson JI, Keck PE, White KL. Kleptomania: a report of 20 cases. American Journal of Psychiatry 1991;148:652-7.
- Presta S, Marazziti D, Dell’Osso L, Pfanner C, Pallanti S, Cassano GB. Kleptomania: clinical features and comorbidity in an Italian sample. Comparative Psychiatry 2002;43:7–12
- Grant JE. Clinical Manual of Impulse Control Disorders. Hollander E & Stein DJ (Eds), American Psychiatric Publishing, Arlington, VA, 2006
- Clark L, Manes F, Antoun N, Sahakian BJ, Robbins TW. The contributions of lesion laterality and lesion volume to decision-making impairment following frontal lobe damage. Neuropsychologia 2003;41:1474-83.
- Clark L, Bechara A, Damasio H, Aitken MR, Sahakian BJ, Robbins TW. Differential effects of insular and ventromedial prefrontal cortex lesions on risky decision-making. Brain 2008;131:1311–22.
- Newcombe VFJ, Outtrim JG, Chatfield DA, et al. Parcellating the neuroanatomical basis of impaired decision-making in traumatic brain injury. Brain 2011;134:759-68.

