Faecal incontinence affects 1-10 % of adults and in 0.5-1% is severe enough to impair daily quality of life.1 The condition remains a socially stigmatising problem with considerable emotional, psychological and physical consequences. Dietary modification, laxatives, constipating agents, suppositories, enemas, bowel retraining and biofeedback are amongst the conventional methods used to address the problem, aiming to achieve a planned and predictable bowel action.1 Here we will discuss the management of an adult patient whose incontinence was only controlled with a procedure originally described for children.
Case report
A 47-year-old lady was admitted in April 2011 with sensory ataxia due to a rapidly progressive peripheral neuropathy. This was further complicated by a pulmonary embolism soon after admission. Within days she had developed double incontinence due to loss of bladder and bowel sensation. Extensive investigations led to a diagnosis of atypical Guillain–Barré syndrome (GBS).
During her stay on the ward she made gradual progress in different aspects of her rehabilitation needs. Despite paraparesis and reduced manual dexterity she was gradually able to safely transfer on a sliding board between bed and chair with minimal assistance. She could self propel in her wheelchair for short distances and later managed to safely perform car transfers when she was assessed for weekend day leave. Her urinary incontinence was successfully controlled by an indwelling catheter, whose Flip Flow valve she could manage independently.
She had a long term tendency to constipation, but as a consequence of her reduced mobility, and unaccustomed hospital diet, this became much more problematic, leading to abdominal discomfort and overflow diarrhoea. Her impaired sphincter control and manual dexterity made it impossible for her to control her bowel, or clean herself after toileting. She was extremely concerned about her erratic bowel control which greatly affected her mood and self confidence to the extent that it overshadowed all the progress she was making in other aspects of her daily activities. She was keen to be discharged, and was otherwise independent in her self care, yet realised with her faecal incontinence she would find it extremely difficult to manage at home.
Having failed to improve the situation despite high doses of oral laxatives such as macrogol and senna, glycerine suppositories and twice daily low volume phosphate enemas, and prompted by her request for a colostomy, we sought advice from a colorectal surgeon with a specialist interest in functional bowel disorders. Antegrade colonic irrigation via Percutaneous Endoscopic Colostomy (PEC) with or without anal plug was suggested as a less invasive treatment than a loop colostomy and bag. The first attempt at colonoscopy by gastroenterologist was abandoned due to inadequate bowel preparation. The second attempt at PEC failed due to inability to safely insert the percutaneous introduction cannula. A combined laparoscopic and colonoscopic approach was organised and patient also gave informed consent for colostomy formation under the same general anaesthesia if a PEC could not be safely placed.
By laparoscopic assisted PEC (LAPEC), the tube was inserted into her descending colon with the access on her left flank below the waistline conveniently within patient’s reach for ease of use. In the subsequent three weeks she learnt to irrigate her bowel independently, and became confident and continent by discharge home.
At review eight weeks after her discharge, she reported no soiling accidents and was extremely happy with the outcome of the procedure, stating that she no longer considered herself to be incontinent and that she now felt in control of her bowel management. She has established a daily routine where she starts irrigation first thing in the morning, sitting on the toilet. She reported minimal oozing of fluid for a short while after emptying her bowels for which she did not feel an anal plug or any extra protection or padding was required. The total time spent daily on the process from start to finish at that point was no more than 40-45 minutes.
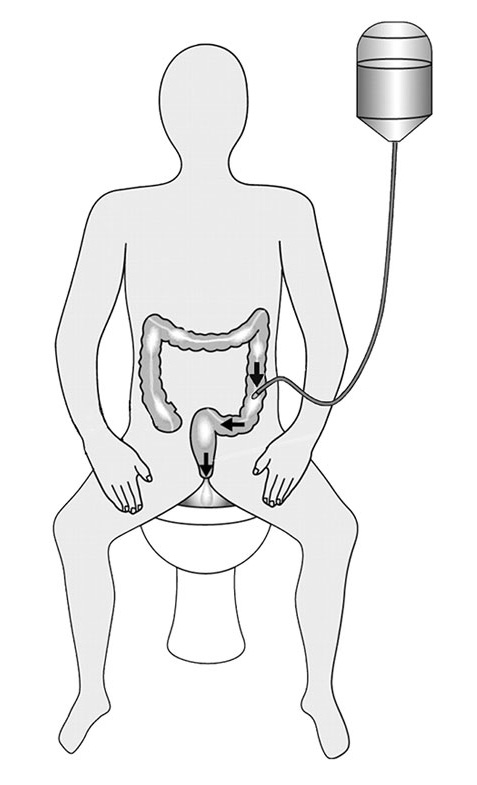
Four week later, she reported further improvement in efficiency, and she had managed to reduce the total time to approximately 30 minutes in the morning after which she can enjoy the rest of her day, confident that her bowels will not open or leak until she irrigates the next morning. She did not report any complications or issues and performed the procedure almost independently, needing assistance only for carrying and hanging up the reservoir containing 1000 ml of tepid tap water on a hook on the wall. (Figure 1).
The patient enjoys a significant improvement in her quality of life, mood and self confidence. She is now considering hydrotherapy and leisure swimming sessions and is making travel plans again. She is currently not taking any laxatives. The only consumable she uses is tap water, which costs much less than the high dose laxatives, enemas and continence pads, on which she was previously dependent.
Discussion
The National Institute for Health and Clinical Excellence (NICE) have recommended PEC insertion for treatment of evacuation disorders and faecal incontinence in both children and adults where conventional treatment options have failed2. The procedure is minimally invasive with similar safety data as Percutaneous Endoscopic Gastrostomy (PEG) and the tube may be left in place long term.2
Mid- to long-term follow up of PEC generally shows significant improvement in bowel management with high levels of patient and carer satisfaction and minimal morbidity. The main long-term complications are granulation tissue, localised cellulitis and accidental tube dislodgement or stoma-related problems such as infection, leakage and stenosis with some requiring surgical revision of the stoma.2,3,4,5
The procedure can be done with a pure endoscopic approach or be laparoscopic-assisted (LAPEC) as described by Rodrigez et al who used this approach for antegrade continence enema (ACE) in children with defecation disorders.6
A similar procedure has been described with good outcomes in management of combined severe constipation and urinary incontinence in children with spina bifida, where a caecostomy tube was placed under direct visualisation during appendicovesicostomy.7
The majority of antegrade colonic irrigation cases reported in the literature are in children, with a mean age of 10 years, where the procedure is used in the treatment of faecal incontinence and refractory constipation, often idiopathic but also commonly in anorectal malformations, spina bifida and Hirschprung’s disease. These often involve a caecostomy or a right bowel approach.3,4,5,8
A left colon approach or sigmoid tube insertion under sigmoidoscopy, also known as LACE, is a safe and often less invasive alternative to caecostomy or right side approach, requiring lower amount of enema fluid with very good mid and long term outcome.2,9,10,11
In adults PEC has primarily been used in treating recurrent sigmoid volvulus and colonic pseudo-obstruction. Left colonic PEC insertion with daily irrigation has been reported to be successful in the management of long-standing obstructed defecation.2,12 The pexy procedure in volvulus and pseudo-obstruction requires placement of two PEC buttons whereas PEC performed for irrigation only requires a single PEC access ideally positioned close to a fixed point within the colon such as splenic flexure, to avoid volving of the bowel around the PEC site.
One study looking at long term functional results of ACE in 69 adult patients over an average follow up period of 75 months has shown a 74% success rate for the procedure. This study identified chronic idiopathic constipation and faecal incontinence secondary to spinal cord lesions as the main indications for surgical intervention in this group of adult patients.13
The daily irrigation process is technically simple and in appropriately selected patients can be conveniently built into a daily routine requiring very little dexterity from the patient and no or minimal assistance from carer. Left colonic PEC deserves to be more widely recognised as an effective treatment for intractable incontinence, in adults with neurological disability.
References
- NICE Clinical Guideline 49, Faecal incontinence: the management of faecal incontinence in adults; Jun 2007
- NICE, Interventional Procedures Advisory Committee, Interventional procedure overview of Percutaneous endoscopic sigmoid colostomy. 2002
- Mousa HM, van den Berg MM, Caniano DA, Hogan M, Di Lorenzo C, Hayes J. Cecostomy in children with defecation disorders. Dig Dis Sci. 2006 Jan; 51(1):154-60.
- Wong AL, Kravarusic D, Wong SL. Impact of cecostomy and antegrade colonic enemas on management of faecal incontinence and constipation: ten years of experience in pediatric population. J Pediatr Surg. 2008 Aug; 43(8):1445-51.
- Sierre S, Lipsich J, Questa H, Bailez M, Solana J. Percutaneous cecostomy for management of faecal incontinence in pediatric patients. J Vasc Interv Radiol. 2007 Aug; 18(8):982-5.
- Rodriguez L, Flores A, Gilchrist BF, Goldstein AM. Laparoscopic-assisted percutaneous endoscopic cecostomy in children with defecation disorders. Gastrointest Endosc. 2011 Jan; 73(1):98-102.
- Lorenzo AJ, Chait PG, Wallis MC, Raikhlin A, Farhat WA. Minimally invasive approach for treatment of urinary and fecal incontinence in selected patients with spina bifida. Urology. 2007 Sep; 70(3):568-71.
- Sinha CK, Grewal A, Ward HC. Antegrade continence enema (ACE): current practice. Pediatr Surg Int. 2008 Jun;24(6):685-8.
- Sinha CK, Butler C, Haddad M. Left Antegrade Continent Enema (LACE): review of the literature. Eur J Pediatr Surg. 2008 Aug; 18(4):215-8.
- Gauderer MW, Decou JM, Boyle JT. Sigmoid irrigation tube for the management of chronic evacuation disorders. J Pediatr Surg. 2002 Mar; 37(3):348-51.
- Rawat DJ, Haddad M, Geoghegan N, Clarke S, Fell JM. Percutaneous endoscopic colostomy of the left colon: a new technique for management of intractable constipation in children. Gastrointest Endosc. 2004 Jul; 60(1): 39-43
- Heriot AG, Tilney HS, Simson JN. The application of percutaneous endoscopic colostomy to the management of obstructed defecation. Diseases of the Colon and Rectum 2002; 45(5):700-702.
- Worsøe J, Christensen P, Krogh K, Buntzen S, Laurberg S. Long-term results of antegrade colonic enema in adult patients: assessment of functional results. Dis Colon Rectum. 2008 Oct;51(10):1523-8



