Recurrent amnesia and confusion associated with limbic encephalitis and complex partial seizures can be a manifestation of paraneoplastic disease and warrants urgent specialist investigation and management to prevent potentially long-term complications.
Introduction
Limbic encephalitis is a rare but important cause of progressive confusion and amnesia. The prognosis is worse if there is a delay in making the diagnosis and the clinical presentation is often misinterpreted as psychiatric. We present a patient who had symptoms for at least 18 months before being diagnosed with a paraneoplastic limbic encephalitis (PLE) secondary to a multifocal testicular seminoma and discuss recent advances in the understanding of limbic encephalitis and its management.
Case report
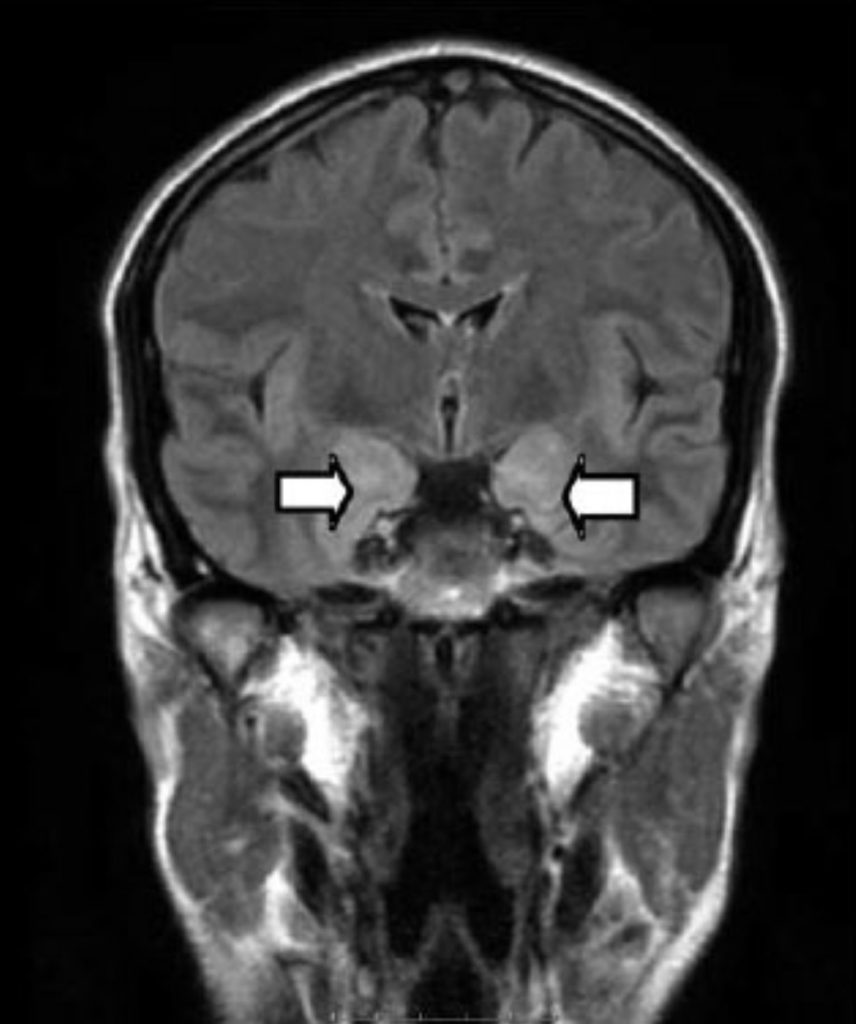
A 37-year-old gentleman presented with recurrent episodes of amnesia and confusion which was initially attributed to emotional stresses from a new job. He was referred to a psychiatrist and treated with antidepressants for anxiety and depression. In spite of treatment, the episodes of amnesia and confusion became more frequent and he was referred for neurological evaluation. On taking a detailed history, he had been having episodes of lip smacking and biting, abdominal sensations rising to the throat and feeling increasingly anxious and fearful. He had no recollection of these events and had become progressively withdrawn and uncommunicative. He was unable to continue working. On examination he had profound anterograde amnesia and patchy retrograde amnesia with relative preservation of working memory. The rest of the neurological examination was entirely normal. His EEG demonstrated intermittent periodic sharp waves which were maximal in the temprofrontal regions. His MRI scan (Figure 1) showed bilateral mesial temporal lobe high signal extending into the hippocampus compatible with limbic encephalitis.
Baseline bloods including tumour markers and chest xray were normal.
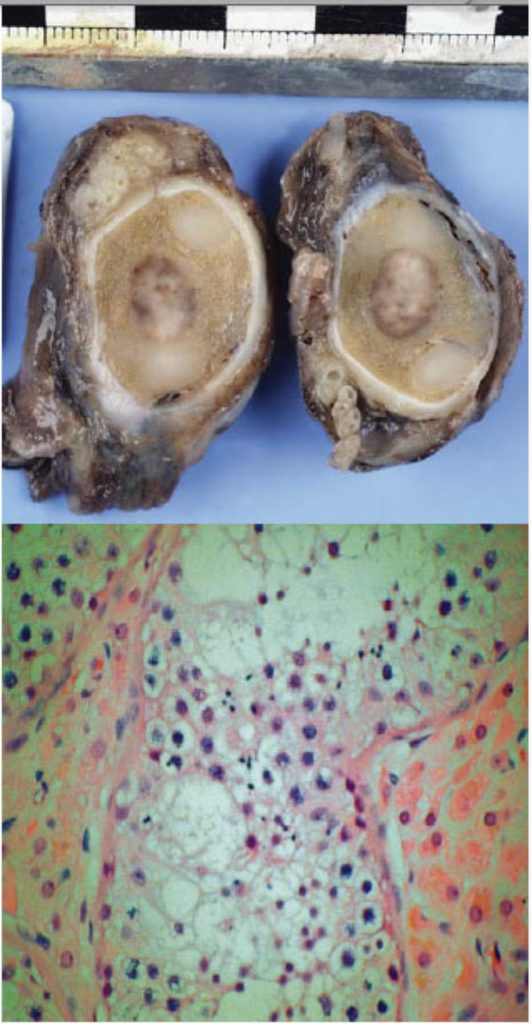
The cerebrospinal fluid (CSF) examination was normal including cytology. An ultrasound scan (USS) of the abdomen and testes revealed a multifocal high signal in the right testis, consistent with a multifocal seminoma. Anti-neuronal antibodies, including anti – Hu, Ri and Yu were normal but the serum was positive for anti-Ma antibodies. A diagnosis of complex partial seizures secondary to PLE was made. The patient underwent right orchidectomy and a histological diagnosis of a multifocal seminoma associated with intratubular germ cell neoplasia stage.
pT1 was confirmed (Figure 2a and 2b). His seizures partially responded to treatment with three anticonvulsants and he was in addition treated with intravenous immunoglobulins (IVIg, 0.4g/kg/day) for five days and intravenous methylprednisolone (1g/day) for three days. His anterograde memory was improving slowly on discharge to a cognitive rehabilitation centre but he still remained profoundly amnesic.
Discussion
Complex partial seizures should be considered in the differential diagnosis of any patient with recurrent episodes of confusion and amnesia. Limbic encephalitis is an important and potentially treatable cause of complex partial seizures.
There is a broad differential diagnosis of pathologies associated with limbic encephalitis including:
- Paraneoplastic limbic encephalitis (PLE)
- Non-paraneoplastic or autoimmune limbicencephalitis
- Viral (herpes simplex, varicella zoster, HSV6) encephalitis
- Toxic e.g. doxifluridine
- Wernicke-Korsakoff ’s encephalopathy
- Systemic lupus erythematosus
Our patient was diagnosed with paraneoplastic limbic encephalitis with secondary complex partial seizures associated with a multifocal seminoma. Tumours that have been described in the literature in association with PLE include: lung (non-small cell and small cell) in 50% of cases; testis (all types) in 20%; and breast in 8% of cases.2 The diagnosis can be difficult to make because recurrent amnesia and confusion can be mistaken for psychiatric disease and these symptoms usually precede the diagnosis of the cancer, sometimes by several years.2 The serum of patients with PLE and testicular cancer often contains antibodies (anti- Ma2) against a protein found in normal brains and in the testicular tumour. Detection of these antibodies in the serum supports the paraneoplastic origin and is of diagnostic significance.1 A retrospective study of 50 patients with PLE has demonstrated that 60% were anti-neuronal antibody positive. All patients who had testicular tumours were positive for the anti-neuronal antibody anti-Ma2. Anti- Ma2 encephalitis can be associated with widespread neurological involvement and should be suspected in patients with limbic, diencephalic or brainstem dysfunction.3 PLE is associated with a poorer prognosis if there is a delay in the diagnosis, anti-Ma2 antibodies are present or if the primary tumour is testicular in origin.2 Immunosuppressants including IVIg and intravenous methylprednisolone have been used empirically with variable objective success. The removal of the tumour burden is probably the most effective treatment and one study has demonstrated a 73% improvement of the neurological syndrome with treatment of the primary cancer.2
A potentially reversal form of limbic encephalitis has been described in association with voltage-gated potassium channels antibodies.4 The neurological manifestations are indistinguishable from PLE. It is important to consider autoimmune limbic encephalitis as a possible cause of recurrent amnesia especially when a primary neoplasm is not found as patients demonstrate substantial clinical improvement following immunosuppression.5
In summary, limbic encephalitis in association with complex partial seizures should be considered in any patient with recurrent amnesia and confusion as a delay in the diagnosis is associated with a poorer prognosis in a potentially curable condition.
References
- Voltz R, Gultekin SH, Rosenfeld MR, Gerstner E, Eichen J, Posner J, Dalmau J. A serological marker of paraneoplastic limbic and brain-stem encephalitis in patients with testicular cancer. N Engl J Med 1999;340(23):1788-95.
- Gultekin SH, Rosenfeld MR, Voltz R, Eichen J, Posner J,DAlmau J. Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings and tumour association in 50 patients. Brain 2000;123:1481-94.
- Dalmau J, Graus F, Villarejo A, Posner JB, Blumenthal D, Thiessen B, Saiz A, Meneses P, Rosenfeld MR. Clinical analysis of anti-Ma2-associated encephalitis. Brain 2004;127:1831-44.
- Buckley C, Oger J, Clover L, Tuzun E, Carpenter K, Jackson M. Potassium channel antibodies in two patients with reversible limbic encephalitis. Ann Neurol 2001;50:73-8.
- Vincent A, Buckley C, Schott JM, Baker I, Dewar BK, Detert N, Clover L, Parkinson A, Bien CG, Omer S, Lang B, Rossor MN, Palace J. Potassium channel antibody-associated encephalopathy: a potentially immunotherapy-responsive form of limbic encephalitis. Brain 2004;127:701-12.



