Abstract
Multiple Sclerosis can present with various clinical manifestations depending on the anatomical location of the demyelinating lesions. We report the case of a 48-year-old woman who complained of blurred vision. Her examination documented a right homonymous hemianopia which had resulted from an active demyelinating lesion located at the origin of the left optic radiation. A first attack of multiple sclerosis was diagnosed. This case highlights the importance of a workup for demyelinating diseases in the setting of any visual dysfunction.
Introduction
Multiple Sclerosis (MS) clinical manifestations are diverse and depend on the part of the central nervous system involved in the disease.1 Ophthalmic symptoms are commonly related to optic neuritis while homonymous hemianopia is a rare presentation.2 We report the case of a 48 year old woman who presented with right homonymous hemianopia as initial manifestation of MS.
Case report
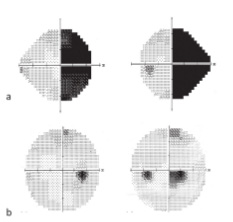
A 48-year-old woman with diabetes mellitus type 2 on metformin, presented to the ophthalmology clinic with a two-week history of binocular blurred vision. One week prior to presentation, she started seeing black spots in her right visual field. These visual symptoms were worsening gradually. Visual fields revealed a right homonymous hemianopia (Figure 1, a), so she was referred to the neurology department for admission. Patient denied any previous history of headache, sensory/motor deficit, visual, speech or gait disturbances. Neurological examination was unrevealing except for a right homonymous hemianopia.
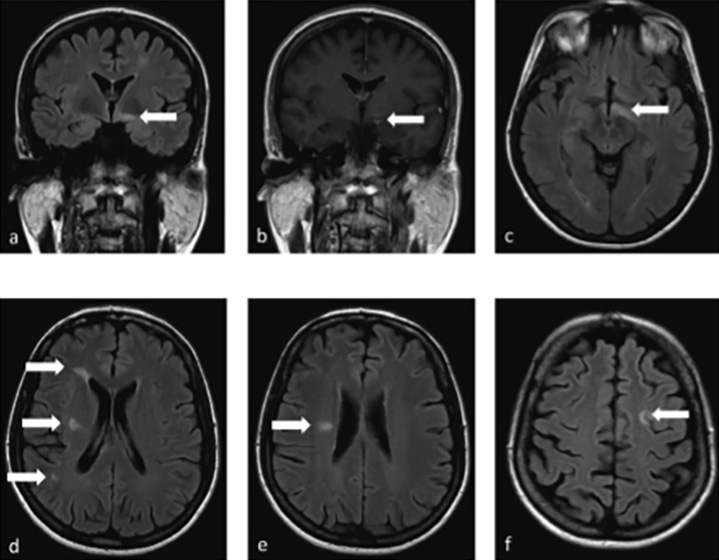
Brain MRI showed multiple lesions that are hyperintense on T2/FLAIR and hypointense on T1 sequences located in the subcortical, periventricular, and right thalamic areas, with one enhancing lesion within the left fornix posterior to the left optic tract (Figure 2).
Cervico-dorsal spine MRI was normal. Serological work up including ESR, ANA, and ACE was unremarkable. Cerebrospinal fluid analysis showed 6 white blood cells, a protein level of 42mg/dL, a glucose level of 80mg/ dL, positive oligoclonal bands and an IgG index of 1.19.
A diagnosis of relapsing remitting MS was established based on the 2017 McDonald criteria. During her hospital stay, the patient received 1g of intravenous methylprednisolone daily for five consecutive days with partial recovery of her visual deficit. Teriflunomide was initiated at a dose of 14mg daily upon discharge.
Follow up visual field testing one month after discharge revealed partial improvement in the right homonymous hemianopia (Figure 1, b).
Discussion
Multiple sclerosis is a chronic, immune-mediated, demyelinating disorder of the central nervous system.1 Early diagnosis is important since multiple disease modifying agents are now widely available.3
Common anatomical locations of symptomatic MS lesions include the optic nerve causing monocular visual loss, the spine resulting in limb weakness or sensory anomalies, the brainstem with subsequent double vision, and the cerebellum leading to ataxia.1 On the other hand, unusual presentations of MS include pain syndromes, cranial nerve abnormalities, movement disorders, paroxysmal symptoms, and homonymous hemianopia,4 the latter being reported in only 0.5%–3.5% of cases.2 More frequently, homonymous hemianopia result from a stroke (69.6%), trauma (13.6%), tumour (11.3%) or brain surgery (2.4%).5
Recovery from homonymous hemianopia secondary to a demyelinating process like MS usually carries a favourable prognosis,6 as seen in our case, where near complete recovery of visual field defect was documented as early as one month after discharge. While in cases of stroke, the recovery is usually partial and requires rehabilitative techniques.7
This case describes a rare initial presentation of MS with homonymous hemianopia related to an enhancing demyelinating lesion located at the origin of the left optic radiation. It also highlights an important reminder that patients may subjectively report homonymous hemianopia as blurred vision.
References
- Brownlee WJ, Hardy TA, Fazekas F, et al. Diagnosis of multiple sclerosis: progress and challenges. Lancet 2017; 389: 1336-46.
- Frederiksen JL, Larsson HBW, Nordenbo AM, et al. Plaques causing hemianopsia or quadrantanopsia in multiple sclerosis identified by MRI and VEP. Acta Ophthalmol 1991; 69: 169–177.
- Reich D, Lucchinetti C, Calabresi P. Multiple Sclerosis, review article. N Engl J Med 378; 2 nejm.org January 11, 2018.
- Evlice A, Demir T, Kaleagası C, et al. Rare onset symptoms in multiple sclerosis. Acta Clinica Belgica 2016, 71:3, 154-157, DOI: 10.1080/17843286.2016.1147675.
- Zhang X, Kedar S, Lynn M.J, et al. Homonymous hemianopias Clinical– anatomic correlations in 904 cases. Neurology 2006; 66; 906-910 DOI 10.1212/01.wnl.0000203913.12088.93.
- Plant GT, Kermode AG, Turano G, et al. Symptomatic retrochiasmal lesions in multiple sclerosis: Clinical features, visual evoked potentials, and magnetic resonance imaging. Neurology 1992; 42:68–76.
- Perez C and Chokron S. Rehabilitation of homonymous hemianopia: insight into blind sight. Front.Integr.Neurosci. (2014) 8:82. doi: 10.3389/fnint.2014.00082.





