Abstract
In a world of increasing globalisation, Neurosurgeons need to be able to diagnose and treat neurosurgical conditions which may not be common to the local population. To illustrate this, we describe the case of an intracranial tuberculoma presenting in the post-partum period. Tuberculosis (TB) is a widely recognised mimic of other conditions, including high grade gliomas, which can result in diagnostic delays. We highlight clinical features that should increase the index of suspicion for TB and create a low threshold for trial of empirical treatment. We also discuss educational partnership strategies that may help facilitate global perspectives in neurosurgical training.
Key take home points:
- Global prevalence of central nervous system tuberculosis is high but is concentrated in certain parts of the world.
- Rapid diagnosis of central nervous system tuberculosis is essential for optimal management, and requires a high index of suspicion.
- Risk factors for tuberculosis include being immunocompromised and having been born or having lived in a high TB prevalence country including the Indian subcontinent. This case report highlights pregnancy as a potential time for TB to manifest.
- Neurosurgical knowledge should be global as well as local, given trends towards international travel and globalisation; collaborative educational initiatives are encouraged to develop this.
Tuberculosis (TB) is a major global health concern. It is one of the top ten causes of death worldwide and the leading worldwide cause of death from infection [1], with approximately 10 million new cases in 2017 alone [2]. Although the majority of TB cases occur in the highest burden countries, it remains a public health issue throughout the world, particularly given the upward trend in worldwide migration rates. Intracranial involvement, either as tuberculous meningitis, tuberculoma or spinal cord tuberculosis, occurs in around 1% of TB cases [3] although the incidence of TBM varies geographically and may not always be reported [4]. Treatment with anti-tuberculosis medications is generally effective for patients with pulmonary TB, and it is estimated that between 2000 and 2017, 54 million lives were saved through correct diagnosis and treatment of TB [2]. However, CNS TB including TB meningitis (TBM), tends to have less favourable outcomes, particularly in cases of multidrug resistant disease or when associated with HIV-1 co-infection [4].
TB is well recognised as a mimic of other conditions, and an atypical presentation in a country such as the UK where TB incidence is relatively low can lead to diagnostic uncertainty. Furthermore, conventional diagnostic techniques such as CSF smear tend to have low diagnostic yield, and prolonged waiting for culture results before commencing treatment can have irreversible consequences for the patient. We describe here the post-partum presentation of an intracranial tuberculoma, which closely resembled a high grade glioma on imaging. In the discussion, we highlight risk factors for TB and discuss educational strategies to incorporate the management of TB and other globally relevant conditions into neurosurgical training programmes in regions where trainees are unlikely to gain a rich experience through their own clinical practice but nevertheless may be required to manage critical cases.
Case report
A 30-year-old female, who had emigrated from India six years previously, presented thirteen days post-partum with a two-day history of severe headache, profound short-term memory loss, fever, vomiting and intermittent bilateral limb paraesthesia. Her temperature was 38.8oC at presentation. No cardiovascular, respiratory, abdominal, perineal or neurological abnormalities were detected on examination in the Emergency Department and inflammatory markers were not significantly elevated (white cell count 8.4 x 109/L, C-reactive protein 1mg/L). Intravenous fluids and intravenous antibiotics were prescribed to cover possible obstetric-related sepsis, and, following medical review, the patient was discharged home. However, she was readmitted within hours, following a brief unexplained loss of consciousness lasting around two minutes.
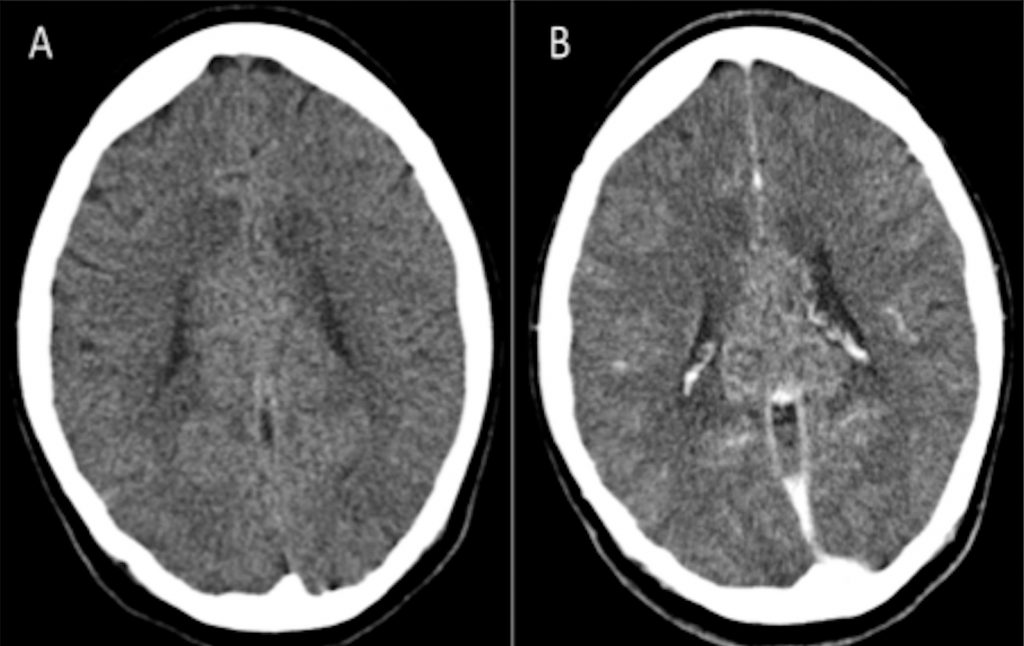
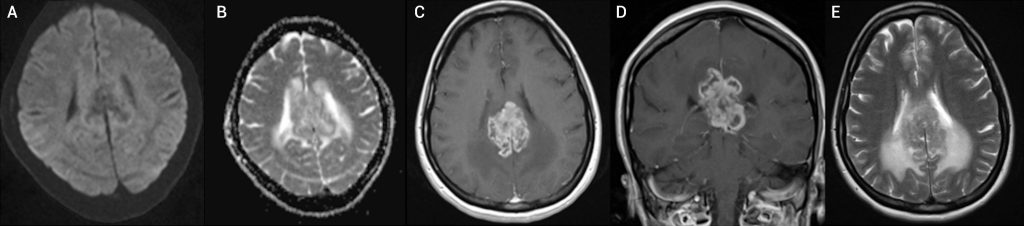
Following readmission, a CT brain scan was performed, revealing a lobulated mass arising from the corpus callosum, extending laterally into both cerebral hemispheres and inferiorly as far as the upper midbrain. There was heterogenous enhancement with contrast and extensive vasogenic oedema (Figure 1). An urgent neurosurgical referral was made. The patient was started on dexamethasone. An MRI scan demonstrated appearances strongly suggestive of a primary malignant brain tumour, with peripheral enhancement within the mass and no evidence of restricted diffusion to suggest pyogenic abscess (Figure 2). No hydrocephalus was noted but the third ventricle was deviated to the right of the midline. Plans were made to biopsy the lesion. A CT scan of the thorax, abdomen and pelvis was normal with the exception of asymmetric enlargement of the right breast and small volume lymph nodes in the mediastinum and right hilum.
A biopsy was scheduled the following week. The finalised report described non-specific chronic inflammation and reaction with no evidence of pyogenic infection, TB or neoplasia. CSF was also sent for analysis. The cytology result was negative but the sample was retained for culture.
The patient underwent marked cognitive decline 2 days post-biopsy, with no response to increased dexamethasone. Repeat CT was unremarkable. Over the next few days, she continued to decline, with hydrocephalus (requiring two EVDs), followed by diencephalic/upper brainstem swelling, which ultimately led to her death. Post-mortem identified the cause of death to be raised intracranial pressure secondary to basal tuberculous meningitis and tuberculoma, and the CSF that had been cultured revealed Mycobacterium tuberculosis after 12 days, which was after the patient’s death.
Discussion
This case describes an intracranial tuberculoma with imaging features closely resembling a high grade glioma. These imaging features combined with the lower incidence of intracranial TB compared with high grade glioma tumours in the UK led to diagnostic delays. In this case the low diagnostic yield of CSF testing and prolonged culture time meant that the patient had died before a diagnosis was reached. The case highlights the importance of maintaining a high index of suspicion of TB in patients from countries where TB is endemic, and having a low threshold for obtaining an infectious disease consult and starting empiric treatment when there is suspicion of TB or biopsy results are not supportive of neoplasia. The following discussion aims to outline key aspects in the history and examination that could point to a diagnosis of TB, discuss guidance about the management of intracranial TB and consider how to integrate TB and similar conditions into the neurosurgical education of trainees who may not live in endemic areas.
Successful treatment of tuberculoma requires prompt diagnosis, initiation of anti-tubercular therapy and consideration of the need for adjunctive surgical intervention. According to the British Infection Society guidelines, tuberculoma should be suspected in any patient with risk factors for CNS TB presenting with symptoms or signs of CNS tuberculoma (including headache, seizures, focal neurological deficit, fever, vomiting or weight loss). Risk factors for TB include HIV or other form of immunocompromise, having been born or lived in a high TB prevalence country, or recent contact with pulmonary TB [3]. Pregnancy and the post-partum may also represent a vulnerability to CNS tuberculoma, and the post-partum period is a particularly common window in which TB manifests in peri-partum females [5]. Modulation of the host proinflammatory response occurs during pregnancy [6] followed by rapid reversal of these changes after delivery, which can result in accelerated progression of previously latent or quiescent infections, including TB [7]. Presentation of TB at extra-pulmonary sites may be more prominent in pregnancy and the post-partum period, including the CNS [8,9].
In 2018, the WHO recorded approximately 10 million new cases of TB. Two thirds of these cases were in six countries (India, China, Indonesia, the Philippines, Pakistan, Nigeria, Bangladesh and South Africa), while only 3% of cases were in the WHO European region and the Americas respectively (https://tbfacts.org/tb-statistics/). Mycobacterium tuberculosis infection of the central nervous system (CNS) occurs in around 1% of all cases of TB [3], and tuberculomas (parenchymal granulomas) occur in up to 50% of patients with CNS tuberculosis according to a recent case series [9]. Based on the WHO statistics for 2018, this would equate to about 1500 new cases of CNS tuberculoma annually in each of the WHO European and Americas regions, compared with 135,000 in India alone.
In the UK, between 2000 and 2016 there were on average 236 new cases of CNS TB reported per year, of which approximately 119 per year were classified as having CNS involvement without meningitis (i.e. tuberculoma or other CNS involvement). According to NHS statistics, there are approximately 4500 new cases of primary brain tumours each year in the UK, of which 70-80% are high grade gliomas, thus, statistically, at least 20 high grade gliomas are seen for every case of tuberculoma (far more if it is considered that many tuberculomas will not present to neurosurgery), making glioma the most likely diagnosis given the scan appearances demonstrated in the present case.
Based on this information, CNS tuberculoma is a rare but important diagnosis in the UK, one that neurosurgical trainees in low incidence regions should know how to manage but are unlikely to be able to become competent in managing through experience based learning.
Different approaches could add a global perspective to neurosurgical training programmes in high income countries (HIC) which lack exposure to TB and certain other pathologies. Many neurosurgical departments in the UK have visiting fellows from low- and middle-income countries (LMIC), either employed directly by Trusts, or on specific training fellowships such as through the International Surgical Training Programme (ISTP), part of the wider MTI programme (Medical Training Initiative). Similar schemes are operational in other HIC [10]. One approach would be to encourage visiting international fellows from LMIC to deliver case-based teaching based on neurosurgical practice in their home countries, selecting important pathologies that are rare but nonetheless relevant to HIC, but are that are seen more commonly in the LMIC setting. This would benefit the fellow as it would develop their teaching experience, as well as bringing a global perspective to routine departmental teaching.
Online platforms and social media feeds are increasingly contributing to neurosurgical learning. For example, educational resources such as The Neurosurgical Atlas are available for trainees to access around the world, and many training systems have an online component to supplement face-to-face learning, such as the UK ebrain learning system (http://www.ebrain.net). Developing the global health components to these learning interfaces to reflect the workload of the global neurosurgical workforce would allow key information and case studies to be accessible to learners around the world, and enable the developers of the learning programmes to gain recognition as leaders in health education and innovation.
Finally, some neurosurgical units have developed twinning ventures or partnerships with a unit in a different part of the world, either holding clinical exchanges or carrying out collaborative research. Traditionally the direction is from an HIC to an LMIC. Building case-based-teaching into twinning ventures, via online platforms such as Skype or Zoom would allow the entire units to benefit from the connection, rather than the smaller number of surgeons directly engaged in the exchange. It would be likely to result in bilateral transfer of knowledge; enhancing training in both participating units, at relatively low cost. Traditionally the development of these collaborations has been challenging due to various factors including lack of institutional support, lack of funding and lack of recognition for academic aspects of global surgery [10]. However, prioritising mutual development and shared learning across national and international boundaries follows the directive of the UN Sustainable Development Goals (SDGs), and in an increasingly interconnected world we suggest that intentionally developing international and globally focused neurosurgical learning communities will enhance both surgical training and patient care.
References
- Hargreaves S, Rustage K, Nellums LB, Powis J, Milburn J, Severoni S, Dara M, Puthoopparambil SJ, Friedland JS. Health Evidence Network Synthesis Report 56. What constitutes an effective and efficient package of services for the prevention, diagnosis, treatment and care of tuberculosis among refugees and migrants in the WHO European Region? Themed issues on migration and health, VII. World Health Organization, Europe.
- World Health Organisation Tuberculosis Factsheet found at: https://www.who.int/news-room/fact-sheets/detail/tuberculosis.
- Thwaites G, Fisher M, Hemingway C, Scott G, Solomon T, Innes J. British Infection Society guidelines for the diagnosis and treatment of tuberculosis of the central nervous system in adults and children. Journal of Infection 2009;59:167-87. https://doi.org/10.1016/j.jinf.2009.06.011
- Wilkinson RJ, Rohlwink U, Misra UK, van Crevel R, Mai NTH, Dooley KE, Caws M, Figaji A, Savic R, Solomons R, Thwaites GE. Tuberculous meningitis. Nature Reviews Neurology 2017;13:581-98. https://doi.org/10.1038/nrneurol.2017.120
- Kalk E, et al. Safety and Effectiveness of Isoniazid Preventive Therapy in HIV-Positive Pregnant Women on Art: An Observational Study using Linked Population Data. Clinical infectious diseases: an official publication of the Infectious Disease of America. https://doi.org/10.1093/cid/ciz1224
- Pearson H. Reproductive immunology: Immunity’s pregnant pause. Nature. 2002 Nov 21;420(6913):265-6. https://doi.org/10.1038/420265a
- Singh N & Perfect JR. Immune Reconstitution Syndrome and Exacerbation of Infections after Pregnancy. Clin Infect Dis. 2007:1192-99. https://doi.org/10.1086/522182
- Cheng VCC, Woo PCY & Lau SKP. Peripartum tuberculosis as a form of immunorestitution disease. Eur J Clin Microbiol Infect Dis 2003:313-7. https://doi.org/10.1007/s10096-003-0927-1
- Wasay M, Moolani K, Zaheer J, Kheleani BA, Smego A, Sarwari R. Prognostic indicators in patients with intracranial tuberculoma: a review of 102 cases. JPMA 2004;54:83.
- Almeida JP, Velasquez C, Karekezi C, Marigil M, Hodaie M, Rutka JT, Bernstein M. Global neurosurgery: models for international surgical education and collaboration at one university. Neurosurgical focus 2018;45(4):E5. https://doi.org/10.3171/2018.7.FOCUS18291








