
Over 800 researchers, clinicians and healthcare professionals attended the MND Association’s 25th International symposium on ALS/MND held in , Belgium from 5 -7 December 2014. With nearly 100 presentations and over 300 poster presentations, the event was filled to the brim with the latest MND science and care practice news.
AAC technology
Around 80-95% of people living with MND will face communication problems as their speech deteriorates.
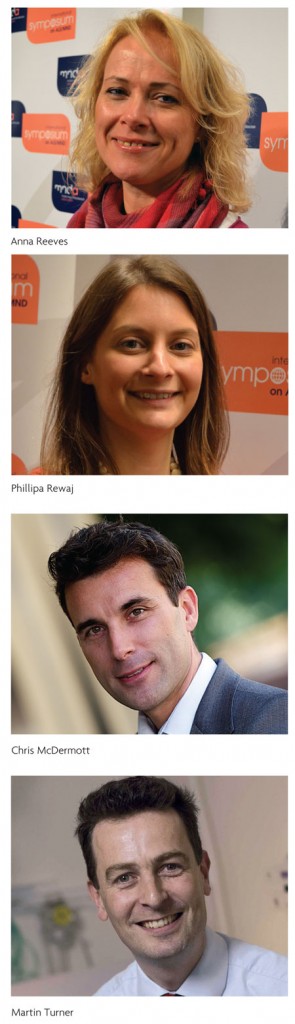
Anna Reeves, The ACE Centre, UK explained in her opening talk that twenty years ago there were just five types of communication aids. Today, there are over 200. Anna said: “All these AAC devices are a bit like a sweet shop saying – look at all these things that can change your life! However, the equipment alone is not the solution, it’s using the right device that’s best for you that is.”
In England, getting access to the right equipment at the right time can be challenging – hence the creation of the AAC referral service. Anna identified and engaged with key politicians with a personal interest in communication, including the Prime Minister, David Cameron: “Engaging with politicians was key for us moving forward. But, there’s
still a way to go – we’ve got the funding but now we need to implement it, getting all our services working together. Over time we will evaluate the AAC referral service to ensure equity across the country, so that everyone living with MND gets the AAC tech they need!”
Another key presentation was from Dr Phillipa Rewaj (University of Edinburgh). She explained that people unwilling to accept a non-individualised voice was the main reason for AAC abandonment, and the voice banking project aims to address this.
The bank has 740 donor voices, which can be ‘mixed’ to create an individualised voice. This means that the researchers can build a voice after just a short 15 minute recording session using what is known as the ‘voice cloning tool kit!’
Dr Rewaj said: “We have used voice banking on 55 people living with MND in Scotland, and have already received feedback from 15 of these.
We have received some extremely positive feedback and all said that they preferred their individual voice to already existing AAC programmed voices.”
End of life discussions
The symposium included a debate on the topic of ‘End of Life’. Dr Van Den Berg, from the Netherlands, discussed that the legal status of euthanasia may affect how physicians think about it. After issuing a survey to physicians involved in the end of life care of people living with MND, there was an 84% response rate from Dutch physicians compared with 64% in England. This shows that there is more of a discussion in Holland where euthanasia has been legal since 2002.
Dr Finlay discussed the situation in the UK, where euthanasia is illegal. 77% of GPs opposed changing the law as did 80% of neurologists and 90% of palliative care doctors. Perhaps the more death is a part of your
day to day the more this affects your moral disposition on the ending of life. Or the ethics of the physicians going into palliative care may initially be geared against it?
How can we be sure that someone has the capacity to make a valid decision given that 30% of people living with MND have mild cognitive impairment? Presence of depression may also hamper our decision as to whether a patient can make a decision relating to their death. During the discussion, Dr Finlay explained that capacity is not one thing. A person may have the ability to choose a single decision e.g. which treatment they want but they may not have the cognitive resources to make a more complex decision such as a decision to end life.
There may also be a fluctuating desire to die as patients’ mood, desires, family relationships change. To illustrate this Dr Finlay tells us to ask people who wish to die, ‘what is so terrible about today?’ and ‘what can I do to improve your day?’
Dr Borasio’s talk was fascinating with respect to what effect offering choice to patients has upon their decisions to go through their end of life treatment. Only physician assisted suicide is allowed in Switzerland. Of the people that decided to receive lethal medication, two thirds did not take it. Instead it was kept at home as a safety net if things get worse. It’s as if the availability of lethal medication is a preventative to suicide and giving people this control affects their disposition towards ending their own life.
The Sheffield Support Snood
Current neck supports available are often restricted. This is because they are designed for other purposes (e.g. such as immobilising the necks of individuals after trauma). This means that people living with MND who experience neck weakness are left with the wrong tool for the job.
Dr Chris McDermott from the Sheffield Institute for Translational Neuroscience (SITraN) said: “People living with MND asked us – can you do anything about this? So, we worked with local MND Association branches to design a neck support for people living with MND.”
The team trialled the new neck support, known as the Sheffield Support Snood, on 26 people living with MND, of which 20 completed the study.
Feedback from participants was that there was strong agreement that the Snood offered support, comfort and no pain compared to existing neck supports.
The next challenge for Dr McDermott is to get someone to make this and take this on, which is difficult due to the relatively small market. However, Dr McDermott stated that he is in the process of discussing this with several companies.
Biomarkers
The session featured a back-to-back presentation from Dr Andrea Malaspina (Queen Mary University of London) and Dr Martin Turner (University of Oxford), who have been pooling their expertise and resources to investigate a promising protein biomarker called neurofilament light chain (NfL).
Measuring these proteins accurately is not an easy process, because damaged neurofilaments tend to clump together in blood and CSF in the same way that they do so in dying motor neurons, so Dr Malaspina and his team have spent several years refining and optimising the technique. He showed that samples from MND cases from both the Oxford and London collections could be discriminated from non-MND controls, with a sensitivity and specificity of over 95% for CSF samples.
Dr Turner said: “Neurofilaments are the building blocks of each and every nerve and are thought to accumulate in the spinal fluid (crossing over into the blood too) as nerves degenerate across a range of conditions. We have found them to be raised in people living with MND.”
“Even though this finding in itself is not unique to MND, importantly the level seems to reflect an individual’s speed of disease progression. What my group has been able to show (as part of BioMOx) is that this level can be directly linked to the damage we see in the motor tracts using the MRI scanner. It confirms that neurofilaments are objectively linked to the disease process in MND, and is a strong candidate for a workable biomarker that we might even be able to measure using only a blood test.”
Induced pluripotent stem cells and MND
Dr Kevin Eggan started a session on induced-pluripotent stem cells (iPSCs), explaining that patients with MND have more electrically active neurones than people who are healthy. This can be shown using things like transcranial magnetic stimulation.
He wanted to investigate why motor neurones are more excitable, and he used iPSCs from two patients with a specific type of the SOD1 inherited form of MND.
When measuring the electrical activity of motor neurones from iPSCs, he found the same thing that he saw in people – that the SOD1-MND motor neurones have more activity compared to activity in healthy motor neurones.
Dr Eggan was using a new technique with an adapted pore within the motor neurones that is sensitive to blue light – when blue light is shone on the motor neurones the channels open and they become electrically active, what’s more is that in his system, the presence of electrical activity causes a tag on another part of the nerve cell to glow red. Through this work he showed that the potassium brake on electrical activity doesn’t work so well in the SOD1 form of MND.
Therapy for SOD1 MND?
With all the talk of new gene discoveries in recent years, the final day of the symposium returned to the original discovery in 1993 that mutations in the SOD1 gene were responsible for around a fifth of inherited MND cases and 2-3% of all cases of the disease.
Although much of our understanding of MND in the past two decades comes from SOD1 laboratory models of the disease, we still don’t know exactly how SOD1 kills motor neurons. But that hasn’t stopped several groups from working on a number of innovative ways of protecting motor neurons from SOD1 toxicity. Although focused on a relatively rare form of MND, some of the strategies being followed could potentially also be applicable to other forms of the disease.
Dr Loreiei Stoica from Massachusetts Medical School, explained that they are switching off the SOD1 gene by reducing the gene activity in the spinal cord of SOD1 mice by over a third, leading to a 50% increase in survival. However, some animals did show side effects that need to be explained before this approach can be considered for the clinic.
Dr Grad (University of British Columbia) has identified a part of the SOD1 protein structure that appears to be crucial for the propagation to occur. Using computers, he has started to design more ‘drug-like’ compounds for testing, based on a molecule called uridine, which he has found is able to reduce SOD1 propagation in lab studies. This is early stage work, but has the advantage that it does not necessarily rely on the drugs getting inside cells, although they still need to be designed to get from the blood into the central nervous system.
Overall the three day event covered some fantastic science, as well as some innovative developments in care practice. Next year the symposium will be held in Orlando in just under a year’s time, and who knows what will be discussed then!
Read detailed reports via the MND Association’s MND Research blog and our peer-to-peer blog ReCCoB
ACNR 2014;15(1):37. Online 15/04/15

