A webinar was hosted by the History of Medicine Society at the Royal Society of Medicine on Wednesday 17th February, 2021.
It was a pleasure to attend, albeit remotely, the above webinar. In the virtual chair was Professor Tilli Tansey, President of the History of Medicine Society, Royal Society of Medicine.
The first talk “The autonomic nervous system and the creation of a medical specialty” was given by Professor Chris Mathias, Emeritus Professor of Neurovascular Medicine at the Queen Square Institute of Neurology, University College, London.
Professor Mathias limited his account to the time period from 1970 to the present, which encompasses his own career and his own significant, and continuing, contributions to the field.
The history of medicine appears at first glance to constitute a continuing process of fragmentation into ever narrower disciplines. Indeed, the Royal Society of Medicine was itself founded in part to bring together the large number of societies representing the core specialties, including neurology, within medicine and surgery that were in existence by the start of the 20th century. It is however the case that a sub-speciality also functions to link one sphere of clinical activity with another: this apparent fragmentation is also a process of fusion and cross-fertilisation. An exemplar of this is the study and treatment of disorders affecting the autonomic nervous system where inputs from cardiology, pharmacology and urology have been of fundamental importance.
To set the scene Professor Mathias began with a mention of the work of John Spalding (Figure 1), neurologist at the Radcliffe Infirmary in Oxford. He was involved in the early years of artificial ventilation, initially in the post-World War II polio epidemic but later also in cases of Guillain-Barré syndrome and tetraplegia (in collaboration with Hans Frankel at Stoke Mandeville). Spalding had measured circulatory reflexes and other autonomic reflexes in both disorders.

Professor Mathias joined this group as a Rhodes Scholar in 1972 (he shared with us his fond memories of arriving at Worcester College), and obtained his PhD for work on spinal cord injuries. However, to the work of these neurologists was added that of the late Professor Sir Stanley Peart, who, as a junior researcher and with the mentorship of the physician/physiologist George Pickering, had discovered that noradrenaline was released following stimulation of sympathetic nerves. That work was published in 1949 and he went on to become one of the pioneers of the study of hypertension which had until then been largely overlooked by cardiologists.
The work was now advanced by the measurement of blood chemistry. It was possible to measure noradrenaline (following the work of Neils Christensen in Aarhus), renin and aldosterone in addition to vascular pressures and flows. Dr Spalding can be heard describing this later research in a recently recorded podcast [1]. I can recommend listening to this.
It is no surprise that the epicentre of autonomic studies then moved to St Mary’s Hospital along with Professor Mathias. In addition to Peart St Mary’s also had on the staff the late Sir Roger Bannister (Figure 2). Sir Roger had trained at Oxford and St Mary’s. He acquired an interest in physiology as an undergraduate and subsequently the neurological control of blood pressure following visits to the unit at Stoke Mandeville. The need for deeper knowledge was highlighted by such phenomena as the rise in blood pressure occurring with a blocked urinary catheter, leading to a fatal cerebral haemorrhage in one patient.

The description of degenerative disorders of the nervous system associated with autonomic failure were a major feature of this next phase of study, including autonomic failure associated with multi-system atrophy – the Shy Drager syndrome, as it was then known. The Clinical Neuroscience section of the RSM has established an annual Lecture in Honour of Sir Roger and we were delighted that Professor Mathias agreed to give the inaugural lecture in 2019.
As an SHO on the Earl/Bannister/Kocen firm at Queen Square in 1980 with an interest in vision, I was encouraged by the strong links between Ophthalmology and Neurology that I observed with Bannister and Earl running clinics at Moorfields and the Western Ophthalmic. Professor Peart (who was married to an Ophthalmologist) was also in the Western clinic. I would add, however, that the application of pupillometry, which has so much to add to the study of autonomic disorders, was not furthered by this team.
Professor Mathias identifies the 1990s as the major period for the application of theory to clinical studies. This followed the development of blood pressure monitoring and the tilt table, for example, along with techniques to investigate the neural control of the bladder. The phenotyping of disorders of the autonomic nervous system, small print in my time, has since become bread and butter material for neurological trainees. He set up the Clinical Autonomic Research Unit at Queen Square and expressed pride in the fact that UCL has recognised Neurovascular Medicine as a medical specialty.
Advances in genetics, neuroimmunology and in understanding the neurological basis of functional disorders have all contributed to the growth of the specialty. There followed the founding of many national and international societies and a specialist Journal. Autonomic neurology is indeed a fully-fledged specialty, now an essential component of any Neuroscience centre.
Next up was Mark Weatherall, Neurologist at Charing Cross. We were expecting a compelling account from a neurologist who is both an expert on headache and has a PhD in the history of medicine and were not disappointed.
The emphasis of the talk was the powerful influence of some theories of the pathogenesis of migraine aura and migraine headache and the failure of others to carry forward any influence. The story begins with the publication of “On Megrim or Sick Headache, and Some Allied Disorders” by Edward Liveing and “On Nervous or Sick-Headache” by Peter Wallwork Latham, both in 1873. Many listeners to the webinar I am sure, like myself, were familiar with Dr Weatherall’s 2012 Brain paper on the topic [2].
As a Downing College alumnus myself I can appreciate that it was Latham who should be considered the “modernist” of the pair. He had after all been appointed to the fellowship of what was and is still today (relatively speaking) a young college. Not only had the endowment of the college created the first new medical professorship in Cambridge since the reign of Henry VIII, but the incumbent at this time was an experimental physiologist: William Webster Fisher.
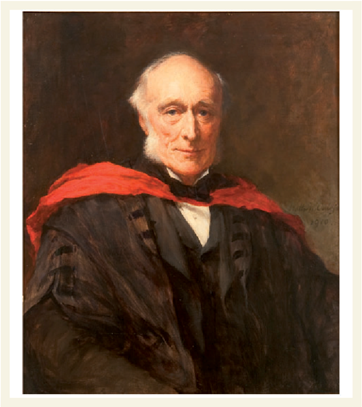
Liveing (Figure 3), on the other hand, had followed the path through Gonville and Caius College, well-trodden by many successful medical men since William Harvey. In accord with this distinction between the two writers was the traditional method of Liveing’s research. It was an analysis of clinical cases which led to his conclusion that migraine was a similar disorder to epilepsy, introducing the theoretical concept of “nerve-storms” as the common factor. Latham proposed vasoconstriction as the cause of the “prodrome” and vasodilation as underlying the headache. This theory was derived from experimental work: most specifically he was influenced by work carried out in Fisher’s Downing College laboratory.
We next heard how the two theories fared over the course of the ensuing 100 years. At University College London and Queen Square the influential William Gowers was lukewarm about both theories but found too many differences between migraine and epilepsy to accept the connection proposed by Liveing. It was an ENT surgeon, Edward Woakes, who had already in 1868 described the treatment of migraine with the vasoconstrictor ergot which had been used in obstetrics for several centuries. Although use was limited until the development of the ergotamine derivative, the fact that this was an effective therapy led to wide recognition. This was also support for Latham’s theory of vasodilatation as the cause for the headache, but the fact that his complete account included vasoconstriction was “left hanging”.
The story jumped forward to 1938 when Graham showed reversal of dilatation of the temporal arteries and Harold Wolff’s demonstration in the 1940s that arteries of both the scalp and the dura were pain sensitive. The theory that originated with Latham and others was gathering strength and was certainly still dominant when I was a medical student.
In the 1970s it was studies carried out by a group working on the nerve supply of cerebral circulation led by Murray Harper that identified CGRP as a potent vasodilator. Louis Edvinson from this group later collaborated with Peter Goadsby in establishing the role of the trigeminal nerve in CRGP release. The efferent arm of the migraine headache was now vulnerable to therapy.
The drift back towards Liveing was influenced by Richard Peatfield’s demonstration in the 1980s that the intensity of pain did not correlate with the degree of vasodilatation: other things needed to be going on around the blood vessel to generate pain. The role of serotonin was established using Wolff’s model by the team at the Allen and Hanbury laboratory led by Patrick Humphrey. The development of sumatriptan was a major outcome of the work.
A further line of research that supported Liveing was emerging from cerebral blood flow studies in Denmark (Olesen, Lassen and Paulson) which demonstrated a slowly spreading oligaemia. This was unlike vasoconstriction and could be the result of the cortical spreading depression of Leão, which also accounted well for many features of some forms of migraine sensory aura. Also weakening the monolithic “vasoconstriction-vasodilatation” model was the increasing recognition of the lack of a consistent link between aura and headache.
Following Dr Weatherall’s excellent talk I am moved to read again the late Nat Blau’s book [3] which, as Dr Weatherall pointed out, gives a clear account of the state of thinking in the 1980s.
Dr Weatherall also directed us to a wonderful paper by Roy and Sherrington of 1890 [4] where the system rediscovered recently as the “glymphatics” of the brain is clearly described. Of relevance to migraine is the authors’ conclusion that: “the lymph which bathes the walls of the arterioles of the brain” provides an intrinsic mechanism by which the calibre of the vessels can be varied locally in response to local functional activity. Had it been appreciated, then earlier recognition that this hypothesis provided the “missing link” between Latham’s nerve storm and Liveing’s vascular theories might not have taken a full century.
References
1Interview with John Spalding, former consultant and research neurologist for Oxford United Hospitals | University of Oxford Podcasts – Audio and Video Lectures
2 Liveing, Edward. On megrim, sick-headache, and some allied disorders: a contribution to the pathology of nerve-storms. Churchill, 1873.
3Blau, Joseph Norman, ed. Migraine: clinical and research aspects. Johns Hopkins University Press, 1987. https://doi.org/10.1002/ana.410240623
4Roy, C.S. and Sherrington, C.S., 1890. On the regulation of the blood‐supply of the brain. The Journal of physiology, 11(1-2), pp.85-158. DOI: 10.1113/jphysiol.1890.sp000321