The 13th Annual Oxford Neurology Course was held at St Anne’s College over 3 days, chaired by Professor Martin Turner and Dr Ursula Schulz.

The course was well organised, and the diverse range of lecture content was brilliant. Lectures were given by neurology consultants and neuropsychiatrists as well as neuroscientists.
There was also a highly enjoyable and intellectually stimulating debate, as well as fascinating cases presented in the “grand round” section.
Social events included a “fun run”, a beautiful dinner at the Ashmolean Rooftop Restaurant and a medical tour of Oxford.
Day 1
Brain Fog and other sequelae of COVID-19 – Evidence and Mechanisms – Professor Paul Harrison, Neuropsychiatrist based in Oxford
Dr Harrison discussed the cognitive sequelae of COVID-19 and the associated mechanisms and risk factors. He discussed the “C-Fog” study findings which interestingly showed two independent biomarker profiles (fibrinogen and d-dimer) at the time of COVID-19 hospitalisation which predict cognitive impairment six and twelve months later. Both biomarkers support an underlying “endotheliopathy/coagulopathy” mechanism. He discussed the concept of “big data” and how this can be used to drive research.
Recent studies have shown that up to 2-3 years after COVID-19 hospitalisation, there is worse cognitive performance (worse than expected) and 22.2% experience severe depression, fatigue and subjective cognitive decline. It was very thought provoking and important to consider, several years post pandemic.
Stroke Care in England: Cinderella to Rambo – Professor Deborah Low, Stroke Physician and National Lead for Stroke (GIRFT), and former National Clinical Director for Stroke Medicine NHS England.
Professor Low gave a comprehensive lecture on the Stroke Service in the United Kingdom, punctuated with personal anecdotes and insights from her illustrious career. Her dedication to improving stroke care for all patients in the NHS was evident and admirable. She reinforced the need to make stroke care a priority as it is the leading cause of disability in the UK. It has huge economic consequences, costing the UK economy £26 billion pounds annually and this is expected to rise. There is higher mortality in the highest deprived areas and amongst ethnic minorities. She discussed the NHS “long-term plan” and the National stroke programme within this – from prevention all the way to end of life care. She also discussed her influence and involvement with the “Getting it Right First Time” (GIRFT) stroke programme. The aim is to provide multimodal support from the level of prevention, urgent care, acute care, rehabilitation and long-term support and requires teamwork and cohesion amongst the primary, secondary and tertiary services as well as with the ambulance services, community services, social care and voluntary sector. Through this, premature deaths can be avoided and hopefully, hundreds of thousands can benefit from better “integrated person-centred care”. She discussed the key features of a good stroke service – which included amongst others: effective primary and secondary prevention, public education, hyperacute stroke care for the first 72 hours, acute stroke unit care for whole admission including in-patient rehabilitation, continuous quality improvement and research. She also discussed the National Optimal Stroke Imaging Pathway, based on GIRFT reviews – with rapid access to imaging being critical, and the use of Artificial intelligence (AI) being incorporated. I was surprised to see the national thrombolysis rate which was 10.5% – the target is to thrombolyse at least one-third of patients who arrive within 4 hours. She also discussed mechanical thrombectomy (MT) and the high level of evidence to support its use as a hyperacute treatment (NNT of 2.6). I was also shocked to know that only 4.8% of the UK has access to MT, hopefully this will improve in the next few years.
Finally, she asked us all to think if we felt self-fulfilment after our workday, and spoke of the “ABC” of core needs at work – “autonomy, belonging and contribution”, which I thought was something important to think about. I am very excited to see how stroke care continues to rapidly advance and evolve.
Basal Ganglia clinical neuroscience – Dr Ashwini Oswal, Movement Disorders Neurologist, Oxford
Dr Oswal had excellent detailed slides allowing us to visualise the various pathways within the basal ganglia circuitry. He spoke about the function of the basal ganglia and how this was discovered. He then discussed models of Parkinson’s disease and how knowledge of this circuitry (the inhibitory and excitatory pathways) led to the consideration of lesions in specific nuclei such as the subthalamic nuclei as a treatment in Parkinson’s – this was the foundation of functional neurosurgery in the 1990s. He then went on to explain deep brain stimulation (DBS) – the principles, targets and indications. With each specific target, the advantages vs disadvantages were discussed. He also discussed the role of basal ganglia not only in movement but in cognition. The future of DBS is exciting and already involves embedding AI with a lot more to look out for on the horizon.
Epilepsy made easy – Dr Stephan Hinze, Epileptologist, Oxford
Dr Hinze discussed key aspects of the care of patients with epilepsy. He discussed making the diagnosis, including features to differentiate functional seizures from epileptic seizures which was very useful. He spoke about how patients describe their seizures and how this also can give us clues about the seizure semiology and whether it may be functional – highlighting the importance of history taking in neurology. Key aspects of management were discussed including considerations in elderly patients (lower doses to be used generally), and then also management of status. Anti-seizure medications (ASMs) including their interactions, side effects, and mechanisms were discussed which was also very helpful. He advised for the use of pyridoxine (vitamin b6) in the treatment of the psychiatric side effects seen in levetiracetam. He also spoke about ASM withdrawal and the associated risks as well as driving advice, and considerations in pregnancy including that ASM levels can drop in pregnancy, folate supplementation (which should be done with more caution now since the JAMA article in 2022 which showed high folate supplementation doses associated with higher risk of childhood cancer) as well as the new MHRA guidance regarding valproate (expanding to men also).
The great debate – “This house believes amyloid clearance therapy is key to managing Alzheimer’s disease” Professor Malhotra AGAINST and Dr Sofia Toniolo FOR
Professor Malhotra is Head of the Division of Neurology in Department of Brain Sciences and Honorary Consultant Neurologist at Imperial College Healthcare NHS Trust, UK. His research focuses on cognitive deficits caused by neurological conditions including neurodegenerative disease. Dr Toniolo is a Neurologist with a special interest in Alzheimer’s disease, who works as a Clinical Research Fellow in cognitive neuroscience at Oxford.
This was one of my favourite sessions of the course. Both speakers were highly engaging, and informative. They argued their points very clearly and effectively. They are both extremely experienced and knowledgeable in this topic and explained the evidence as well as the controversies with current anti-amyloid treatment. Professor Malhotra won the debate and for me, it was how he carefully unpacked the moot and did not say that amyloid clearance therapy was not important, but more so that it was not “key”.
Day 2
This was a full day with another incredibly comprehensive and diverse schedule of talks.
(Re) Emerging neuro infections – Dr Davies, Neurologist with a special interest in neuro-infections, Imperial College Hospitals, London.
This was an excellent talk to start the day. Dr Davies discussed emerging vs re-emerging infections affecting the nervous system over different periods of time and emphasised the prevalence of certain infections within areas of the UK and specifically London. It was startling to see how prevalent tuberculosis and HIV are in certain areas of London. He then discussed three interesting cases with pertinent learning points – including a case of measles in an immunocompromised patient, secondary syphilis with calvarial diseases and tick born encephalitis. He emphasised the importance of vaccinations not only at an individual but also at community level, and also that many infections are vaccine preventable. He advised considering flavi viruses in meningoencephalitis even if there has been no travel outside Europe. He discussed the neurological diseases that can occur with hepatitis E infection, and that encephalitis is most frequently described in those who are immunosuppressed. He flagged invaluable resources for neurologists and indeed all medical specialists, including a review of Neurosyphilis by Hammil et al, UK adult guidelines for the management of viral encephalitis by Solomon et al, the encephalitis website [www.encephalitis.info] as well as the Queen Square Multidisciplinary encephalitis MDT amongst others.
Where CAR-T meets neurology – Dr Adam Handel, Neurologist, Head of the Oxford Autoimmune Neurology group, Oxford
Dr Handel started by explaining how CAR-T therapy works. CAR-T therapy was initially developed to be used for refractory lymphomas, especially acute lymphoblastic leukaemia in children and has shown excellent results thus far in the treatment of haematological malignancies. It is an incredible treatment, which is essentially customised for the individual by using their own T cells and reengineering them. This lecture was highly relevant as CAR-T therapy is being used more frequently and its potential for use beyond oncology is being explored. There are trials of the use of CD19-targeted CAR-T in neurological diseases such as multiple sclerosis, myasthenia gravis and in other autoimmune conditions such as systemic lupus erythematous. Dr Handel discussed the possible neurological side effects of CAR-T, and the factors that can affect the specific neurotoxicity that might manifest as well as the severity. He discussed “Immune effector cell-associated neurotoxicity syndrome” (ICANs) and the key clinical features, as well as who might be more prone to developing it and the timeline – i.e. the time of onset (usually 1 week post CAR-T) and duration. He signposted to useful grading guides and explained that this will in turn guide the therapy choice. He noted to especially look for cerebral oedema and perform fundoscopy on these patients, this will affect how you grade the severity and then in turn treatment. Tocilizumab is considered if there is evidence of cytokine storm. There can also be delayed neurological effects including movement disorders up to 1 month after. He emphasised that the role of the neurology team is to exclude alternative causes or complications such as infections. He discussed investigations used in ICANs such as MRI, FDG PET and EEG and specific findings to look out for. I thought Dr Handel explained this very complex topic of immunotherapy and associated neurotoxicity in a very detailed and comprehensible way – and made it very relevant to practicing neurologists, with several excellent papers and guidelines included throughout.
Neuroscience of decision making – Laurence Hunt, Neuroscientist, Oxford
I found this lecture very interesting, and it was a nice break from more clinical lectures to have a scientific focus. He discussed various experiments used in the study of translational neuroscience and various models as well as modalities such as EEG and MEG used to extrapolate data. He used these experience and evidence to explain the decisions are a “dynamical process” and that that we can measure neurophysiological markers of this internal process.
My top 10 tips – Professor John Paul Leach, Epileptologist, Glasgow.
Professor John Paul Leach gave an insightful, thoughtful and truly humbling lecture accounting his career and some of the highs and lows, how he got into neurology and important life lessons applicable to all neurologists and indeed to all people. He spoke of the evolution of neurology as a growing specialty, and how it has been “humanised”. I was very moved by his words and his vulnerability and honesty in how he spoke of some of the difficult times in his career. A few of the take home messages which especially resonated for me were the need to be kind to yourself, resilient, non-judgmental and to appreciate that every experience changes you and also importantly that “you are not your job” – something that can so easily feel that way as a junior doctor in training.
How to look after people with MS – Dr Lucy Mathews, Neurology Consultant MS Specialist, Oxford/Milton Keynes
This was a very comprehensive lecture which covered essential aspects of care of patients with multiple sclerosis. Dr Mathews focused on the importance of the multidisciplinary team at the heart of achieving a high standard of patient-centred holistic care. She summarised the “Life in the day of an MS Consultant” including tasks for the MS clinic which was very helpful. She highlighted that we should always revisit the diagnosis, and offer education and support, working closely with the MDT. She discussed evidence about when to start disease modifying treatment and went through the “NHS England Treatment Algorithm for Multiple Sclerosis Disease Modifying Therapies” which was updated in 2023. She had brilliant slides with tables summarising the various DMTs including their route, mechanism, dosing frequency, efficacy, side effects and monitoring which was very helpful. She emphasised the importance of physiotherapy and encouraging maintenance of mobility wherever possible, and discussed management of spasticity including more advanced treatment options. She discussed bladder symptoms in MS, constipation, sexual dysfunction and fatigue – and importantly also the social impact the disease has on the individual which is so important to think of always.
Best of Oxford Grand Rounds (3 cases) – Dr Sam Mackrill, Neurology SpR, Dr Zaw Moe, Neurology SpR, Dr Richard Butterworth, Neurology Consultant, Oxford/Milton Keynes
The grand round was excellent and included 3 interesting and educational cases.
The first case was a 42-year-old female who presented with coryzal symptoms, and then developed bright lights in the right eye, with twitching in her right thumb. She had a background of IgA nephropathy and was immunosuppressed. On examination she had a right homonymous hemianopia and a skin lesion on her hip. The investigations were sequentially reviewed with key details of the history – including that she worked in her allotment frequently. She was found to have a ring-enhancing lesion on intracranial imaging which was later biopsied, and she was found to have Cladophialophora Bantiana which is a soil dwelling black mould.
The second case was a 51-year-old male who presented with generalised tonic-clonic seizures with episodic slurred speech. He became anarthric day 5 after his initial presentation and had bilateral facial weakness. An MRI head one month after his presentation showed T2 weighted white matter signal abnormalities with peripheral enhancement of lesions, with normal MRA. Differentials were discussed including inflammatory demyelinating plaques, atypical PML, lymphoma and vasculitis. Key aspects of the history were revisited and it was noted that the patient did have long term excessive cocaine use. In light of this – given the clinical presentation and imaging findings, the patient was diagnosed with “cocaine leukoencephalopathy and multifocal inflammatory leukoencephalopathy following levamisole consumption”.
The third case was a 28-year-old male who presented with generalised tonic-clonic seizures. These were occurring for 2 years and would wake him from his sleep. They were stereotypical attacks which would start with him hyperventilating then bending forwards. He was diagnosed with frontal lobe seizures. Frontal lobe seizure semiology was discussed, including that there is commonly integrated behaviour during seizures and stereotypies, which is a useful learning point. Depending on the anatomical structure involved, the frontal seizure semiology differs. He summarised this in a very informative table from a paper in Journal of Neurology in 2022 by Mcgonigal et al. For example, if the prefrontal cortex is involved then there is “temporally integrated goal directed action and behaviour” which may manifest as more complex patterns of gestural motor behaviour and can have emotional features.
The Long view of FND – Dr Christopher Bass, Neuropsychiatrist, Oxford.
Dr Bass is a very experienced Neuropsychiatrist with extensive experience in the management of functional neurological disorder and provided an insightful and educational lecture detailing the progressing of FND overtime and its evolution as well as key research findings. He included anecdotes from his own practice and discussed his current medico-legal work. He reinforced that functional disorders are not physical or psychological but rather a combination of both, which I found interesting to consider.
[ Read more: Mechanism of Functional Neurological Symptoms | ACNR Journal ]


Day 3
Neuro prognostication – Dr Anton Pick, Neurorehabilitation Consultant, Oxford
Day 3 started with a thought-provoking lecture on “Neuro prognostication” by Dr Pick. He started by discussing a case of a 28-year-old male who had a road traffic accident and was subsequently in a coma. He highlighted learning points at each stage of the case discussion – starting with discussing poor prognostic indicators such a low GCS initially, fixed pupils, abnormal motor presentation and seizures as well as widespread brain injury on MRI. He discussed relevant guidelines throughout including the Royal College of Physician’s guideline on “Prolonged disorders of consciousness (PDOC) following sudden onset brain injury”. He then defined “coma”, “vegetative state” and “minimally conscious state” – with key differentiating features to be aware of and emphasised the “emergence” from disorders of consciousness and the necessary criteria. Timeline is critical – i.e. a disorder of consciousness becomes “continuing or prolonged DOC” if it continues for more than 28 days, and then depending on further timing duration becomes “chronic”. He discussed the fascinating and complex pathophysiology of prolonged disorders of consciousness, explaining that it is a “whole brain” phenomenon rather than being able to localise the pathology to a single anatomical substrate. He advised that functional investigations are more useful (as compared to EEG) in differentiating the different disorders of consciousness.
Dr Pick discussed the RCP clinical assessment for prolonged disorders of consciousness and provided a systematic step wise approach.
He explained the importance of early specialist rehabilitation input and what it may involve including formalising the diagnosis, treating spasticity, navigating complex communication such as best interest meetings and treatment escalation, offering support and education to loved ones and helping to establish 24 hour care programmes. He spoke of current treatments (so far amantadine in severe traumatic brain injury has the most evidence) and that there are compelling treatments on the horizon. Overall, Dr Pick summarised the lecture by reiterating that prognostication is wrought with uncertainty, that thinking of the best interest of the patient is key. He advised use of the “FOUR score” instead of GCS in acute assessment of patients with disorders of consciousness. He brought us back to the case he mentioned at the start, which had a remarkably positive outcome with the patient returning essentially to their normal function – again reinforcing the need for patience, foresight and advocating for the patient – the case discussion gave a personal touch to the lecture and put everything discussed into perspective.
Sleep for Neurologists – Dr Mkael Symmonds
Dr Symmonds is a Sleep Specialist Neurologist and Neurophysiologist who runs a sleep clinic in Oxford. He spoke of the common complaints he sees in clinic regarding sleep and how he assesses aspects of sleep in a detailed and systematic way (amount, timing, quality, structure, continuity, disturbance). He discussed the objective measures he uses such as sleep diaries and then also how he uses polysomnography. He talked us through graphs of sleep cycles and the specific findings in each stage. He went on to discuss central disorders of hypersomnolence (narcolepsy and cataplexy) and their diagnosis and classification with the underlying pathophysiology. He discussed the staged treatment for narcolepsy and CNS related hypersomnias including explaining the pharmaco-mechanism of medications such as modafinil. He defined insomnia and the three types and explained that it becomes “chronic” if it occurs 3 nights per week for more than 3 months. The main focus of treatment of insomnia is cognitive behavioural therapy. His slides were excellent including having flow charts of the assessment and management in clinic as an overview, combining elements including initial assessment, initial treatment and further investigations. He went on to discuss sleep related movement disorders including restless legs syndrome (which can be divided into primary or secondary) and the treatment including iron replacement and ropinirole amongst others. He discussed the parasomnias detailing the various clinical manifestations and explained they can be related to REM vs non-REM sleep and that they are usually managed with behavioural measures. He discussed the differentiation of parasomnias with seizures and emphasised stereotypical movements are most suggestive of frontal lobe seizures. It was an excellent and comprehensive lecture and he also signposted clinical guidelines and relevant references throughout.
[ Read more: articles in the ACNR sleep series ]
How to look after people with MND – Professor Martin Turner, Professor of Neurology and Clinical Neuroscience, Oxford
Professor Turner has a wealth of experience in the field of Motor Neuron Disease (MND). The title of his lecture was “A New Era in MND”. He started by discussing the underlying pathophysiology of MND and the clinical phenotypes. He discussed important considerations in the assessment during clinic – including nutrition, secretion management, communication aids, helping with disability and loss of independent, cognition and behaviour amongst others.
He emphasised that MND is not a diagnosis of exclusion, and key clinical features should direct you the diagnosis, although he did recognise there is often diagnostic delay. He went on to discuss the “mimics” (reminding us that there is an excellent review in Practical Neurology which summaries the “Mimics and chameleons of Motor Neuron disease”, Martin et al 2013) including Multifocal motor neuropathy, Kennedy’s disease and Inclusion body myositis – going through each diagnosis with defining clinical features and investigation findings. He went through educational cases with learning points for each – including of cervical myeloradiculopathy which can mimic “limb-onset” MND but also might be an incidental finding in MND age group. He also discussed cases within a family of brothers who had genetic ALS FTD due to C9orff2 expansion mutation. He advised that you should be careful when sending a genetic panel and always make sure you will be able to explain the results.
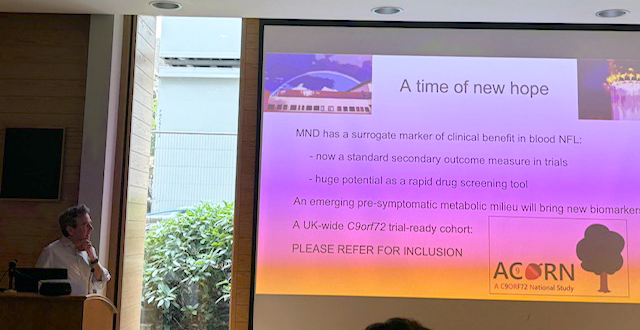
He discussed the drug trials thus far which have proved to be difficult in measuring long term survival. Neurofilament light chain is a non-specific marker of neuronal damage – it measures the rate of disease progression in the context of MND, not the extent of disease. It is currently being used to monitor therapeutic treatment in ALS which is an exciting space to keep an eye on. It allows for the progression to further phases of clinical trials and for screening and repurposing more quickly.
PD made easy – Dr Nagaraja Sarangmat, Consultant Neurologist, Oxford
Dr Nagaraja Sarangmat is a Neurologist with a special interest in movement disorders. His lecture was titled “Parkinson’s Disease Made Easy” and provided extensive practical information for the management of patients with Parkinson’s. He went through the NICE recommendations for GP referrals and important aspects of the initial clinical assessment, including relevant investigations. He also discussed when to start levodopa compared to levodopa sparing agents – and discussed this in context with the open label randomised trial in the Lancet in 2014, which gave evidence to support early initiation of treatment with levodopa. He also discussed the non-motor symptoms of PD and useful questionnaires to assess for these in the clinic setting.
Once the diagnosis is confirmed, a multidisciplinary holistic approach is encouraged including involving the Parkinson’s disease nurse and therapists. Offering advice regarding diet and exercise is also important. He advocated signposting patients to the Parkinson’s UK charity website. He then discussed the need to reassess over time for any progression of symptoms, including non-motor symptoms (such as reviewing for REM sleep disorder, impulse control disorders, orthostatic hypotension).
Dr Sarangmat discussed illustrative cases with learning points, including to be mindful of those who do not respond to levodopa and to revisit the diagnosis in those cases, look for atypical features. He summarised the clinical and radiological features of the Parkinson’s Plus syndromes and gave advice regarding management.
[ Read more: Parkinson’s Disease Archives | ACNR ]
He discussed the NICE advice for treatment of impulse control disorders including predictors to look out for and associated factors. He emphasised the need to address anxiety and depression, urogenital symptoms (noted to avoid oxybutynin), speech and language as well as the previously mentioned non-motor symptoms.
Advanced therapies including use of apomorphine and deep brain stimulation (DBS) were discussed, and the NHS England criteria for DBS referral were succinctly summarised.
Finally, Dr Sarangmat went on to discuss the future of treatment of Parkinson’s which is likely to include more focus on neuroprotection. He discussed the “Cure-GDNF” trial of Prasinezumab, which is a glial cell lined derived neurotrophic factor, and has been shown to slow motor progression in rapidly progressing early-stage Parkinson’s disease – however the mode of delivery is being explored including the use of genetic modification such as viral vectors. This will be very interesting to see if it can translate into clinical practice in the future.