Abstract
Benign positional vertigo (BPV) is well known to produce brief episodes of vertigo triggered by head movements in the plane of the affected semicircular canal. The characteristics of the positional nystagmus reflect the location of the otoconia within the semicircular canal. Here we review the nystagmus profiles of common BPV subtypes and present three mimics that could be misdiagnosed as BPV.
Introduction
Vertigo brought on by head movement is the hallmark of benign positional vertigo (BPV) in which displaced otoconia from the otolith maculae stimulate the semicircular canal afferents in response to changes in head position. Positional nystagmus with an axis orthogonal to the affected semicircular canal is a reliable physical sign that dispenses with the need for any other diagnostic tests. Less commonly, positional vertigo and nystagmus can arise from other peripheral and central vestibular disorders.
There are two theorised mechanisms of BPV: In canalithiasis, the gravitational movement of free-floating otoconia within the canal-duct is thought to cause abnormal endolymph flow;1 In cupulolithiasis, otoconia attached to the cupula are presumed to alter its density relative to the surrounding endolymph and generate gravity-dependent deflections of the cupula.2 The stimulus is transient in canalithiasis and sustained in cupulolithiasis. This is reflected in the temporal pattern of benign positional nystagmus which may be paroxysmal or persistent. The nystagmus direction reflects stimulation of the involved semicircular canal. BPV is treated with repositioning manoeuvres which use knowledge of the orientation of the canals within the head to direct the otoconia back to the utricle through a sequence of head movements.
Posterior Canal BPV
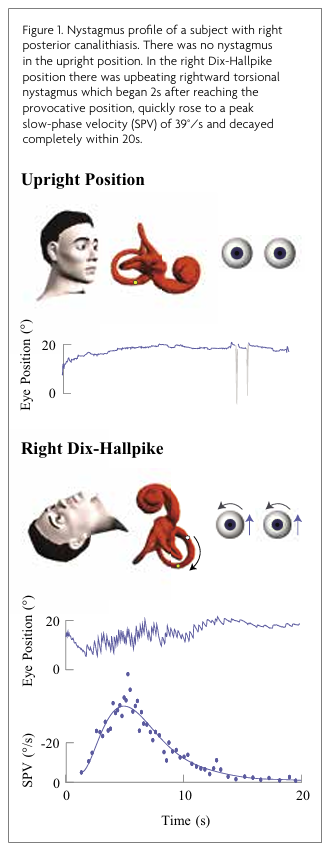
Patients with posterior canal BPV (PC-BPV) experience brief episodes of vertigo brought on by head movements such as sitting up, lying down, bending forward or looking up. Episode duration is typically less than one minute however residual symptoms may persist for hours.3 The Dix-Hallpike test causes free-floating otoconia in the posterior canal to gravitate away from the ampulla, producing excitatory nystagmus. The fast-phase of the nystagmus is upbeating and torsional with the upper pole of the eye beating towards the affected ear. Nystagmus begins after a latency of seconds, rapidly rises in velocity to a peak, and decays within one minute as the otoconia reach the lowest gravitational point and the cupula returns to a neutral position (Figure 1, Video 1).4
In our sample of 100 subjects with posterior canalithiasis, the median nystagmus onset latency was 1.4 s (range 0-14.2 s), duration was 12.5 s (range 2.5-34.5 s) and peak slow-phase velocity (SPV) was 37.3°/s (range 3.1-218.6°/s). The peak SPV was reached at 2.9 s (range 0-19.2 s) after onset and declined by half within 3.4 s (range 1.1-16.4 s).
In posterior cupulolithiasis, the nystagmus direction is the same however there may be no latency, the nystagmus is less intense and persists for more than one minute as the heavy cupula deflects downwards, providing sustained stimulation.5
It is very rare for lesions other than BPV to present with nystagmus similar to posterior canalithiasis. Vestibular migraine (VM) can present with positional vertigo and nystagmus, however it is more likely to resemble cupulolithiasis as the nystagmus is generally without latency, persistent and lower velocity.6 The direction is most often horizontal but may be vertical or torsional.6 Unlike BPV, nystagmus in VM is not necessarily consistent with a single semicircular canal plane. The presence of migraine features such as headache, photophobia, phonophobia and visual aura, support the diagnosis of VM, however there is also a high prevalence of migraine amongst patients with BPV and the two conditions may co-occur.7
Case 1
A 48-year-old female presented with a 13 year history of recurrent positional vertigo and right-sided throbbing headaches with nausea. She had a history of motion sensitivity. Her initial examination revealed spontaneous diagonal up/right beating nystagmus. In the right Dix-Hallpike position she had vigorous upbeating rightward torsional nystagmus which persisted for more than two minutes. She underwent backward rotations on the Epley Omniax rotator, a motorised chair for the treatment of BPV, with a preliminary diagnosis of right posterior cupulolithiasis. After three treatments, she reported some improvement in her positional vertigo but continued to experience migraines and disequilibrium. Her follow up assessments revealed spontaneous diagonal up/right beating nystagmus which was enhanced during Dix-Hallpike testing (Figure 2, Video 2).
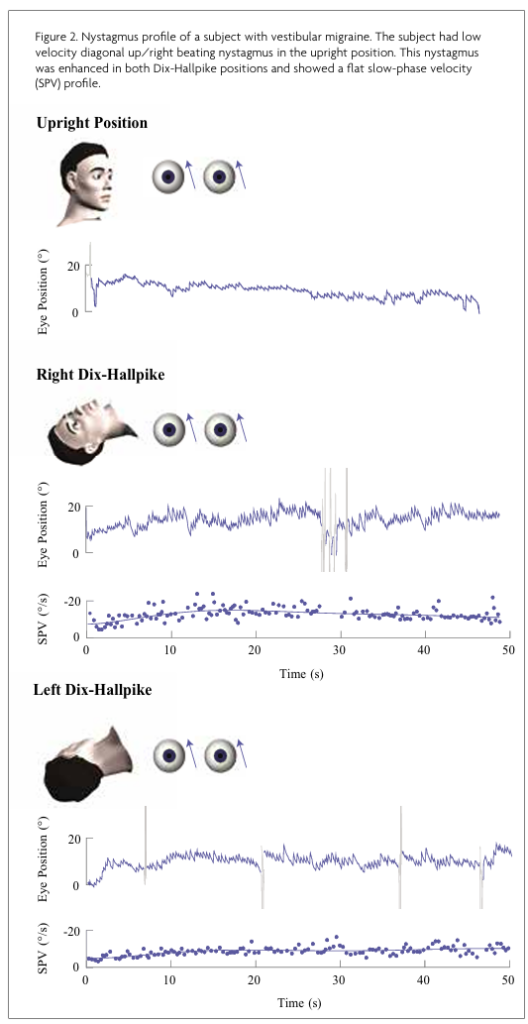
Her imaging and audio-vestibular tests were normal. VM was considered the dominant pathology and she commenced migraine preventative therapy with good effect. She continued to experience intermittent episodes of positional vertigo with some relief with repositioning manoeuvres. The final diagnosis was VM with co-occurring BPV.
Anterior Canal BPV
Anterior canal BPV (AC-BPV) can produce paroxysmal predominately downbeat nystagmus in the supine straight heading-hanging position or during the Dix-Hallpike test. The side of the Dix-Hallpike test cannot be used to lateralise AC-BPV as one or both ears down may result in mobilisation of otoconia within the anterior canal.8 If there is a visible torsional component, this should beat towards the affected ear, however it is not always apparent as the anterior canals are positioned closer to the sagittal plane than the posterior canals.8 Nystagmus onset is immediate or within a few seconds of reaching the provocative position,9 should last less than one minute and exhibit a rapid increase to a peak velocity followed by a more gradual decay (Figure 3, Video 3).
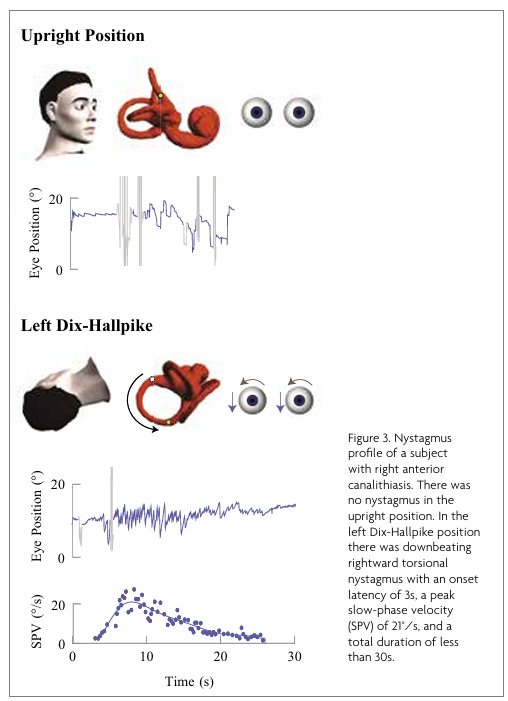
In our sample of 3 subjects with anterior canalithiasis, the nystagmus onset ranged from 0-2.8 s upon reaching the Dix-Hallpike position. The duration was 13.4-23.1 s, the peak SPV was reached within 3.0-5.4 s and decayed by half within 6.4-10.5 s.
Paroxysmal positional downbeat nystagmus may also be attributed to atypical PC-BPV, in which otoconia positioned near the common crus evoke an inhibitory response upon Dix-Hallpike testing.10
AC-BPV accounts for less than 2 percent of BPV cases and should be diagnosed with caution.11 Paroxysmal positional downbeat nystagmus, closely resembling AC-BPV, has been documented in central lesions involving the inferior cerebellar vermis.12 The co-occurrence of different types of nystagmus depending on the positioning manoeuvre and the presence of other oculomotor abnormalities may help to differentiate central positional vertigo from BPV. A small number of patients with VM may present with positional downbeat nystagmus which may be separated from AC-BPV by its sustained nature and low intensity.6 Imaging is always warranted in the presence of additional neurological signs or when the symptoms fail to resolve with repositioning.
Case 2
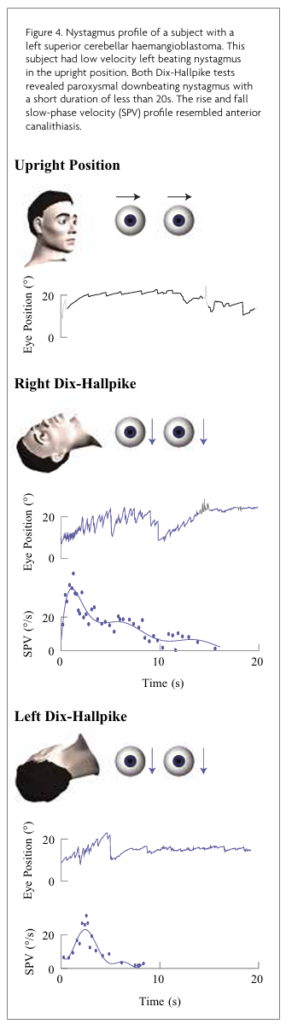
A 66-year-old male presented with a 2-3 year history of episodic vertigo, mainly when rolling over in bed. He reported a gradual decline in hearing bilaterally, a recent onset of pulsatile tinnitus and non-throbbing bilateral occipital headaches associated with nausea. He had subtle left beat spontaneous nystagmus. Both Dix-Hallpike tests showed paroxysmal downbeat nystagmus lasting less than 20 seconds (Figure 4, Video 4).
He was treated for presumed AC-BPV, without improvement. MRI with MRA/MRV revealed a lesion in the left superior cerebellar hemisphere extending into the left superior cerebellar peduncle. He underwent a complete resection of the lesion, which was confirmed to be a haemangioblastoma. The pulsatile tinnitus and unresponsiveness to repositioning were red flags pointing to a central cause.
Horizontal Canal BPV
Patients with horizontal canal BPV (HC-BPV) typically report short episodes of vertigo induced by rolling over in bed or head movements in the yaw plane. Horizontal nystagmus is elicited during the supine roll test and is paroxysmal geotropic (beating towards the ground) in the case of typical canalithiasis or persistent apogeotropic (beating away from the ground) in the case of cupulolithiasis.
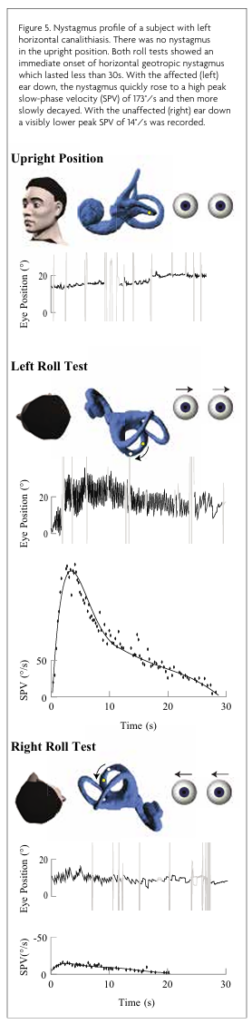
In the geotropic variant, rolling onto the affected side produces an intense excitatory nystagmus while rolling onto the unaffected side produces a less intense inhibitory nystagmus (Figure 5, Video 5).
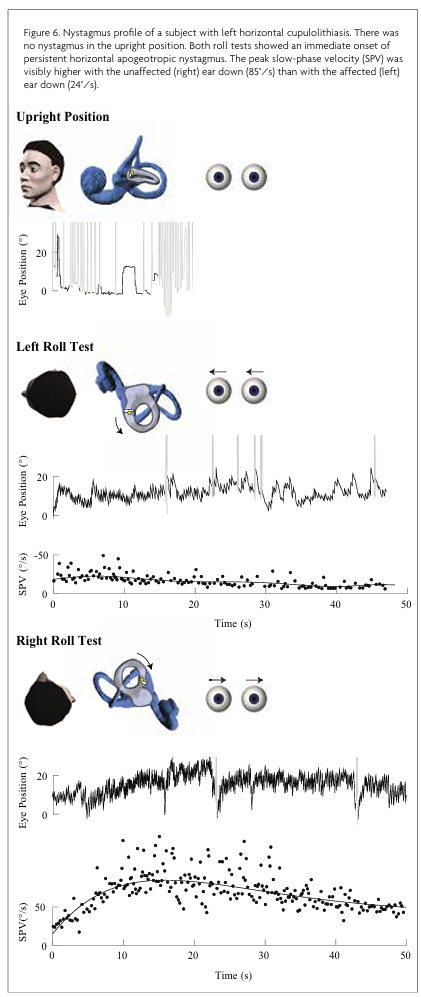
The reverse is true for apogeotropic variants, in which the affected side is identified as the side with the weaker response (Figure 6, Video 6).
In a sample of 30 subjects with horizontal canalithiasis, nystagmus onset was typically instantaneous after rolling onto the affected side (median onset latency 0 s, range 0-4.4 s) and lasted less than one minute (median duration 26.1 s, range 9.9-48.5 s). The median peak SPV was 52.2°/s (range 9.1-241.2°/s). The peak SPV was reached after 3.6 s (median, range 0.3-24.4 s) and declined by half at 7 s (median, range 2.8-24.6 s). With the unaffected ear down, a less intense paroxysm (median peak SPV 17.2°/s, range 3.6-96.7°/s) with similar temporal characteristics was seen.
In a sample of 10 subjects with horizontal cupulolithiasis, nystagmus onset was mostly immediate (median 0 s, range 0-3.0 s) during the roll test. The median peak SPV was 69.6°/s (range 9.9-105.4°/s) when lying on the unaffected side and 13.5°/s (range 4.5-61.9 °/s) with the affected ear lowermost. The time taken to reach the peak SPV was prolonged compared to canalithiasis (median peak latency with unaffected ear down 18.6 s, range 5.7-27.8 s).
Due to the 30-degree incline of the horizontal canals with respect to earth-horizontal, pseudo-spontaneous nystagmus may be seen in some patients with HC-BPV.13 Pseudo-spontaneous nystagmus beats towards the affected ear for the apogeotropic variant and away from the affected ear for the geotropic variant, although this may vary depending on the starting position of the otoconia.13,14 Leaning the head back or lying down in a supine position further elevates the ampulla and should produce nystagmus in the same direction as the pseudo-spontaneous nystagmus, while bowing the head forward should produce nystagmus in the opposite direction.15
Horizontal geotropic positional nystagmus has been described in acute VM and central lesions of the cerebellar peduncle and lateral medulla. This nystagmus is persistent rather than paroxysmal, making it easy to separate from canalithiasis.16-18 Horizontal apogeotropic nystagmus has been reported in central lesions typically of the cerebellar vermis and nodulus,16-19 VM, and more rarely in Ménière’s Disease and vestibular schwannomas.18 The nystagmus can closely resemble cupulolithiasis and differential diagnosis may rely on the presence of other neurological or aural signs and the response to repositioning manoeuvres. Choi et al.19 suggested comparing the intensity of sitting and supine nystagmus. They found that a more intense nystagmus when supine compared to sitting is consistent with HC-BPV while a symmetrical response between sitting and supine is more indicative of a central lesion.
Case 3
A 41-year-old female presented with a two-month history of episodic unsteadiness and left lateropulsion when walking, accompanied by nausea and occipital pressure. Separately, she reported episodes of spontaneous and positional vertigo lasting seconds. She had no auditory symptoms. She had a history of migraine and motion sensitivity. She had no spontaneous or gaze evoked nystagmus. Head shaking provoked up beating nystagmus. In either Hallpike position, she had persistent low velocity up beating nystagmus. In either roll position she had persistent horizontal geotropic nystagmus (Figure 7, Video 7).
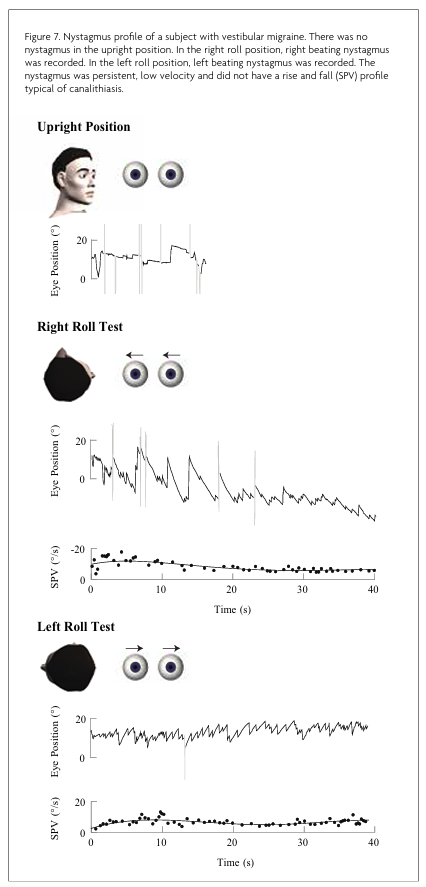
Her audiogram and vestibular function tests were normal. Her MRI scan showed diffuse white matter hyperintensities. The patient was diagnosed with VM and treated with migraine preventative therapy. Repeat MRI scan one year later showed white matter hyperintensities were stable.
Conclusion
A history of brief episodes of positional vertigo and characteristic nystagmus upon positional testing are fundamental to the diagnosis of BPV. Alternative diagnoses must be investigated when the nystagmus is atypical, unresponsive to repositioning manoeuvres or when there are additional otologic or neurological signs incompatible with a diagnosis of BPV.3
References
- Hall S, Ruby R, McClure J. The mechanics of benign paroxysmal vertigo. J Otolaryngol 1979;8(2):151-158.
- Schuknecht HF. Cupulolithiasis. Arch Otolaryngol 1969;90(6):765-778.
- von Brevern M, Bertholon P, Brandt T, Fife T, Imai T, Nuti D, Newman-Toker D. Benign paroxysmal positional vertigo: Diagnostic criteria. J Vestib Res 2015;25:105-117. doi:10.3233/VES-150553
- Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). Can Med Assoc J 2003;169(7):681-693.
- Hain TC, Squires TM, Stone HA. Clinical implications of a mathematical model of benign paroxysmal positional vertigo. Ann N Y Acad Sci 2005;1039(1):384-394. doi:10.1196/annals.1325.036
- Polensek SH, Tusa RJ. Nystagmus during attacks of vestibular migraine: An aid in diagnosis. Audiol Neurotol 2010;15(4):241-246. doi:10.1159/000255440
- von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, Neuhauser H. Epidemiology of benign paroxysmal positional vertigo: A population based study. J Neurol Neurosurg Psychiatry 2007;78(7):710-715. doi:10.1136/jnnp.2006.100420
- Bertholon P, Bronstein AM, Davies RA, Rudge P, Thilo KV. Positional down beating nystagmus in 50 patients: Cerebellar disorders and possible anterior semicircular canalithiasis. J Neurol Neurosurg Psychiatry 2002;72(3):366-372. doi:10.1136/jnnp.72.3.366
- Lopez-Escamez JA, Molina MI, Gamiz MJ. Anterior semicircular canal benign paroxysmal positional vertigo and positional downbeating nystagmus. Am J Otolaryngol 2006;27(3):173-178. doi:10.1016/j.amjoto.2005.09.010
- Vannucchi P, Pecci R, Giannoni B. Posterior semicircular canal benign paroxysmal positional vertigo presenting with torsional downbeating nystagmus: An apogeotropic variant. Int J Otolaryngol 2012:1-9. doi:10.1155/2012/413603
- Korres S, Balatsouras DG, Kaberos A, Economou C, Kandiloros D, Ferekidis E. Occurrence of semicircular canal involvement in benign paroxysmal positional vertigo. Otol Neurotol 2002;23(6):926-932.
- Choi J-Y, Kim JH, Kim HJ, Glasauer S, Kim J-S. Central paroxysmal positional nystagmus: Characteristics and possible mechanisms. Neurology 2015;84(22):2238-2246. doi:10.1212/WNL.0000000000001640
- Asprella-Libonati G. Pseudo-spontaneous nystagmus: A new sign to diagnose the affected side in lateral semicircular canal benign paroxysmal positional vertigo. Acta Otorhinolaryngol Ital 2008;28(2):73-78.
- Lee S-U, Kim H-J, Kim J-S. Pseudo-spontaneous and head-shaking nystagmus in horizontal canal benign paroxysmal positional vertigo. Otol Neurotol 2014;35(3):495-500. doi:10.1097/MAO.0000000000000250
- Choung YH, Shin YR, Kahng H, Park K, Choi SJ. ‘Bow and lean test’ to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope 2006;116(10):1776-1781. doi:10.1097/01.mlg.0000231291.44818.be
- Lee HJ, Kim ES, Kim M, Chu H, Ma HI, Lee JS, Koo JW, Kim HJ, Hong SK. Isolated horizontal positional nystagmus from a posterior fossa lesion. Ann Neurol 2014;76(6):905-910. doi:10.1002/ana.24292
- von Brevern M, Radtke A, Clarke AH, Lempert T. Migrainous vertigo presenting as episodic positional vertigo. Neurology 2004;62(3):469-472. doi:10.1212/01.wnl.0000106949.55346.cd
- Lechner C, Taylor RL, Todd C, Macdougall H, Yavor R, Halmagyi GM, Welgampola MS. Causes and characteristics of horizontal positional nystagmus. J Neurol 2014;261(5):1009-1017. doi:10.1007/s00415-013-7223-5
- Choi J-Y, Glasauer S, Kim JH, Zee DS, Kim J-S. Characteristics and mechanism of apogeotropic central positional nystagmus. Brain 2018;141(3):762-775. doi:10.1093/brain/awx381


