Abstract
Unilateral functional or non-organic hearing loss is a rare condition in adulthood which unlike many other functional diseases in neurology can be relatively easily identified with simple audiological assessment and investigations that target distinct parts of the auditory pathway. We describe a previously healthy 19-year-old female who presented with an acute onset of unilateral non-organic hearing loss with ipsilateral visual and sensory symptoms. We brie y review the literature on functional hearing loss and some of the tests available to investigate it.
Key Points
- Functional hearing loss is a rare manifestation of non-organic illness in adults
- Unlike other non-organic illnesses, functional hearing loss is readily amenable to objective diagnosis
- The auditory axis can be interrogated via audiological and electrophysiological investigations from the level of the tympanic membrane to the auditory cortex
Case study
A 19-year-old female presented to an emergency department with an acute onset of right sided hearing loss, mild right eye visual blurring and numbness affecting the right arm and leg.
Nine months earlier she had developed right sided ear pain with discharge diagnosed as otitis externa by an ENT specialist and treated successfully. Six weeks later, she had two further episodes of right sided tinnitus and progressive step-wise deterioration of her hearing with audiometry performed on two successive tests over 5 months yielding pure-tone averages of 48 and 51 dB HL on the right ear and 21dB and 16 dB HL on the left (normal threshold ~10-15 dB HL). These symptoms were accompanied by right mastoid process tenderness. She was diagnosed as having unilateral idiopathic sensorineural hearing loss and was treated with courses of oral steroids without benefit.
Examination in the emergency department revealed hearing loss in the right ear on bedside examination, slightly decreased visual acuity to 6/9 in the right eye and reduced pinprick and light touch sensation over the right arm and leg but not the face. Ophthalmological review revealed a normal cornea, lens, retina and visual fields with no evidence of interstitial keratitis to suggest Cogan’s syndrome. Inflammatory markers including ESR, CRP, ANA, ENA and ANCA were negative and an MRI of the brain was normal, with no evidence of abnormalities in the internal acoustic meati and the mastoid cavities.
Initial pure-tone audiometry demonstrated a normal hearing threshold for the left ear (pure tone average = 15dB HL) and severe hearing loss on the right (pure tone average = 85 dB HL). She was initially treated with a short course of oral prednisone for possible recurrent idiopathic sensorineural hearing loss (SNHL).
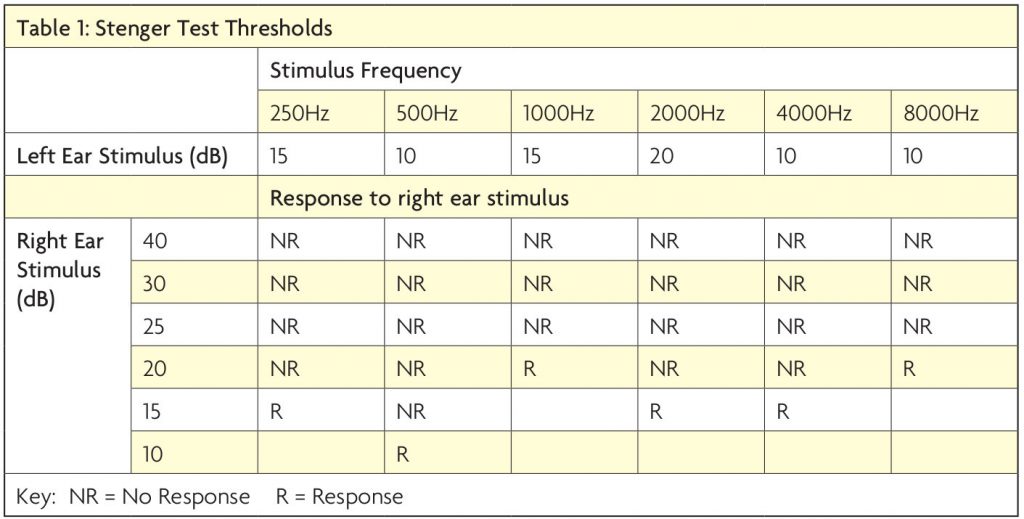
Subsequent assessment indicated that her speech audiometry for the right ear was better than that expected from her pure tone testing with a recognition score of 67% at 30 dB. Unmasked audiometry did not reveal the expected “shadow curve” on right ear testing representing transmission of auditory stimuli to the intact left ear and reported hearing thresholds showed poor reproducibility. A Stenger test was positive, indicating a non-organic pattern of hearing loss. While our patient’s reported auditory threshold on her right ear was in the range of 80 dB, Stenger testing at octave frequencies between 250-8000 Hz yielded true thresholds between 10 – 20dB (Table 1).
Transient and distortion product otoacoustic emissions (TEOAEs and DPOAEs, respectively) were clearly present indicating intact cochlear outer hair cell function. Brainstem auditory evoked responses (BAER) using stimuli above and below reported thresholds (75 & 92 dB nHL) were normal bilaterally confirming the intact pathways from the auditory nerve to the inferior colliculus. Cortical evoked potentials recorded using 1000 Hz and 4000 Hz stimuli of 0 – 80 dB nHL at 10 dB intervals yielded thresholds of 20 dB nHL on either side, indicating symmetrical and normal or very near normal hearing at the tested frequencies (Figure 1).
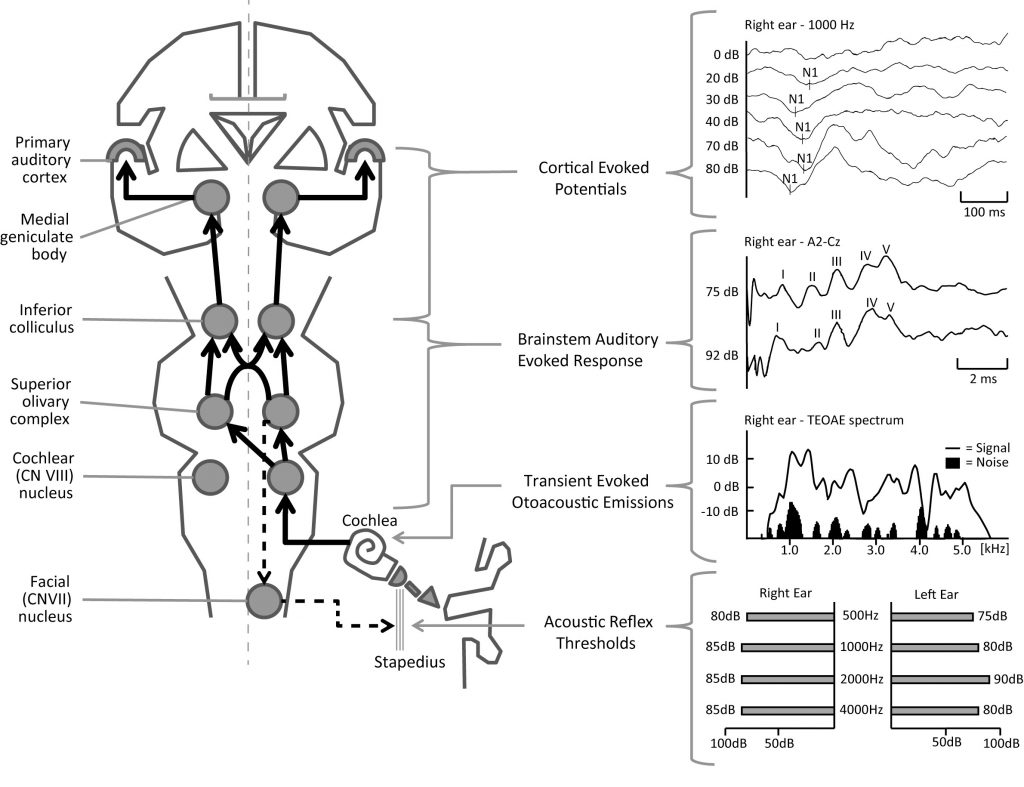
Sound waves are conducted by the ear through the ossicular chain to the cochlea where the hair cells transduce the signal into a neural impulse that is transmitted along the cochlear part of cranial nerve VIII to the ipsilateral cochlear nuclei. Auditory signals are relayed through to bilateral superior olivary complexes and rostrally through the inferior colliculi and medial geniculate bodies before connecting with the primary auditory cortex on the superior temporal gyrus bilaterally.
Objective tests of this axis include cortical evoked potentials that correspond with responses arising from the inferior colliculus through to the cortex. The brainstem auditory evoked response has numbered waveforms that correspond with structures from the cochlear nerve to the inferior colliculus. Otoacoustic emissions are mediated by the cochlear outer hair cells in response to auditory stimuli and can
be detected in the external ear canal. Finally the acoustic reflex is triggered by suprathreshold auditory stimuli and is mediated by efferents originating from the superior olivary complex and synapsing with the facial nuclei causing contraction of the stapedius muscle and tautening of the ossicular chain which is detectable through impedance testing. Representative normal results from our patient are shown on the right side of the figure.
Her right-sided visual and sensory symptoms resolved over a few days but she reported persistent hearing loss as well as episodic true spinning vertigo lasting seconds on review one month later. She was referred to a neuro-otologist for further investigation of her auditory and vestibular function.
Neuro-otological assessment revealed no spontaneous, gaze-evoked, head-shaking or positional nystagmus. Bedside and 3D video head impulses in all six semicircular canal planes were normal, as were ocular and cervical vestibular evoked myogenic potentials, indicating that all five vestibular end organs were intact. Although plans were made for the patient to record video-oculography at home to capture nystagmus accompanying her episodic vertigo, the episodes ceased after this assessment.
Further evaluation revealed recent psychological stressors including a relationship break-down, parental pressures and recent deferment of her tertiary studies. The patient was reassured that investigations had revealed her auditory pathways were intact; non-organic hearing loss was discussed.
Whilst accepting this diagnosis, she continued to report ongoing hearing impairment. Ten months later she presented to another hospital with an acute left hemi-paresis which resolved spontaneously within two days and for which no organic cause could be found. Upon follow-up at the time of manuscript preparation, the patient agreed to see a clinical psychologist in order to further address her non-organic symptoms.
Discussion
Non-organic presentations are common in neurology and can be diagnostically challenging. In such cases, the role of the Neurologist is primarily to exclude organic disease which is attempted by a combination of thorough clinical evaluation and appropriate investigations.1 This case of adult-onset unilateral non-organic hearing loss highlights an uncommon presentation which is particularly amenable to diagnosis via audiological testing.
Functional hearing loss is more common in children and is rare in adults outside of military populations where considerations of financial compensation may skew results.2 In adults, it typically presents in 20-40 year olds with a female predominance, differentiating it from idiopathic SNHL which typically affects those beyond the 5th decade of life.3 In one Japanese case series, 24 of 31 patients were female with an age range between 7 and 39 years. Approximately 45% of these patients presented with unilateral hearing loss, 45% with bilateral loss and the remainder with a mix of organic and non-organic disease in different ears.3
In the majority of non-organic hearing loss, the diagnosis can be made by audiological techniques alone. Hallmarks of non-organic disease on audiological testing as shown in our case include inconsistencies in thresholds on repeat testing (>10dB), and speech recognition thresholds that are markedly superior to pure tone audiometric thresholds.4,5 A ‘shadow curve’ is the level at which an air conducted stimulus may be heard by the contralateral normal ear in unilateral deafness.5 The absence of a ‘shadow curve’ as evident in our case is a marker of non-organic hearing loss.
The Stenger test (Figure 2) has been in existence for more than 100 years and has good sensitivity (99%) and moderate specificity (~70%) in the evaluation of unilateral non-organic hearing loss.6 Measurement of the stapedial reflex via impedance testing is another technique to confirm the intact function of the auditory nerve, lower auditory brain-stem pathways, the middle and inner ear. This response consists of the contraction of the stapedius muscle in response to an auditory stimulus above threshold and can be detected in the compliance of the tympanic membrane5 – our patient’s stapedial reflexes were normal bilaterally (Figure 1).
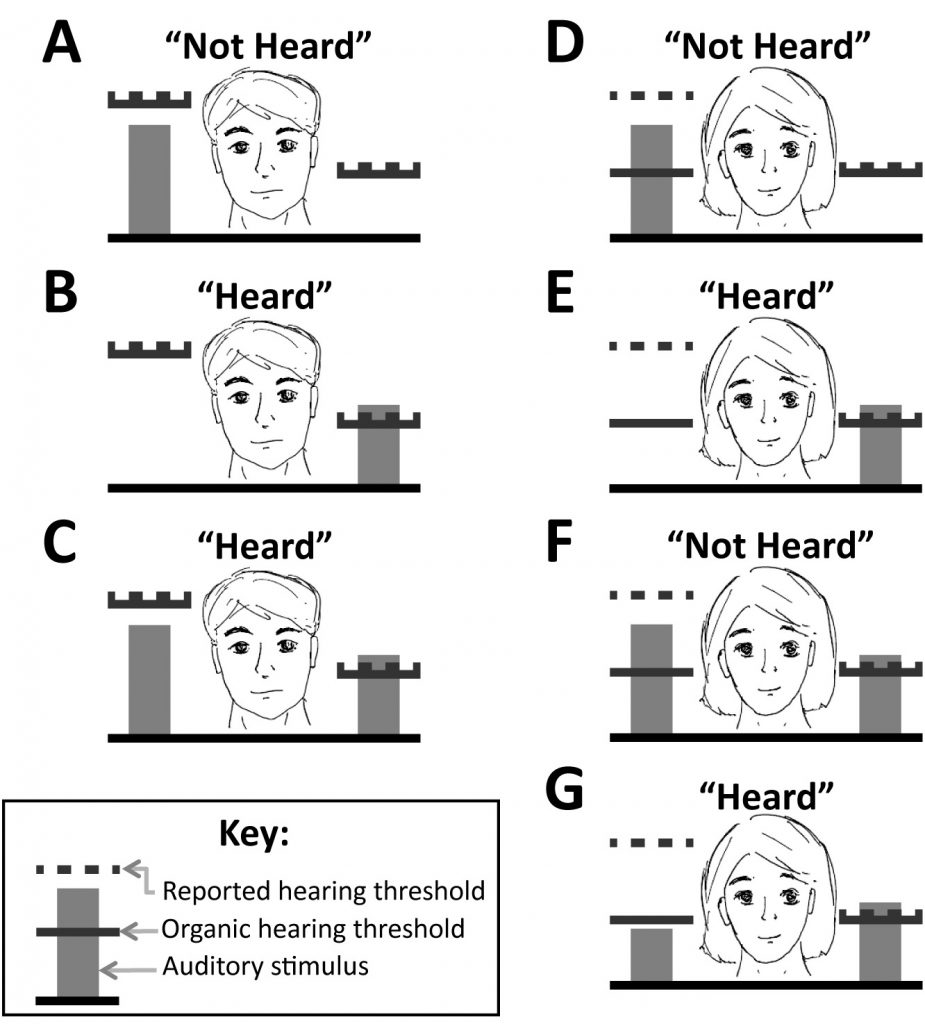
The Stenger test can be used to differentiate organic and non-organic causes of unilateral hearing loss through exploiting the binaural fusion phenomena by which a tone of the same frequency displayed to both ears simultaneously is perceived only in the ear in which it is louder.
True auditory thresholds are represented in this diagram by solid lines for each ear. Reported auditory thresholds or the level above which sound is reported as heard is represented by dotted lines. Auditory stimuli presented to each ear are displayed as vertical bars, the height of which corresponds to the intensity of the stimulus.
Consider panels (A)-(C) representing a patient with an organic cause of right sided deafness, seen as high auditory thresholds on the right. In panel (A), a subthreshold stimulus presented to the right ear is not heard whereas a suprathreshold left stimulus in (B) is heard. In panel (C) with both stimuli presented together, the subject perceives the suprathreshold left tone and gives a response of “heard”, a plausible physiological result.
Consider panels (D)-(G), representing our case, of a patient with non-organic right sided deafness and an elevated reported auditory threshold but normal organic threshold on the right. When presented in isolation, the “sub threshold” right stimulus is reported as “not heard” in (D) and the supra threshold left stimulus is heard in (E). However when these two tones are presented together in (F), the subject perceives the louder tone only on the right by virtue of fusion phenomena and gives a “not-heard” response. This result is implausible and non-physiological given that the same tone played to the left ear alone in (E) is reported as heard, strongly suggesting a non-organic hearing loss. When a tone below the subject’s true right threshold is combined with the supra threshold left stimulus in (G), the subject then lateralises to the intact left ear and provides a “heard” response.
OAE is a method employing the ability of the outer hair cells of the cochlea to generate low frequency sounds detectable within the external acoustic canal in response to auditory stimuli. They are typically present only when true hearing thresholds are ²20dB HL7 and have been described by some authors specifically in the evaluation of functional hearing loss.8 Both TEOAEs and DPOAEs were measured and present bilaterally in our patient.
The BAER is an averaged electrical response detectable from surface electrodes originating from the cochlear nerve and brainstem. BAERs have been used to infer true auditory thresholds by other authors.9 BAERs were normal in morphology and latencies bilaterally in our patient.
Non-organic hearing loss is not always a self-limiting disorder. In a case series of six adult patients with proven unilateral non-organic hearing loss for instance, only two cases had resolved twelve months after onset despite knowledge of the diagnosis.10
We thus describe an unusual case of non-organic illness presenting as an acute onset of unilateral hearing loss. It is possible that the initial episode of otitis externa served as a model for her subsequent presentation. Unlike many other non-organic illnesses in neurology, functional hearing loss is readily diagnosable via audiological techniques that include perceptual tests, objective threshold testing and tests that assess specific parts of the auditory pathways.
Authorship Statement
J Lee was involved in the initial care and assessment of the patient. He researched, drafted and reviewed the manuscript and also created and compiled the associated figures.
J Smith was involved in the audiological assessment of the patient. She participated in the drafting and reviewing of the manuscript.
R Taylor was involved in the audiological assessment of the patient and in reviewing the manuscript and figures.
M Welgampola was involved in the care and assessment of the patient. She drafted and reviewed the manuscript and figures and also provided scientific direction and guidance.
M Hayes was involved in the care and assessment of the patient. He drafted and reviewed the manuscript and figures and also provided scientific direction and guidance.
Funding
RL is supported by a University of Sydney UPA scholarship. MW is supported by the National Health and Medical Research Council of Australia.
References
- Hayes M, Thompson PD. Chapter 39: Psychogenic movement disorders. In Hallett M. Movement Disorders, Handbook of Clinical Neurophysiology, Volume 1.: Elsevier; 2003;p629-638.
- Austen S, Lynch C. Non-organic hearing loss redefined: understanding, categorizing and managing non-organic behaviour. Int J Audiol. 2004;p.43(8):449-457.
- Hiraumi H, Tsuji J, Kanemaru SI, et al. Non-organic hearing loss. Acta Otolaryngol Suppl. 2007;(557):3-7.
- Lin J, Staecker H. Nonorganic hearing loss. Semin Neurol. 2006;p. 26(3),321-330.
- Gelfand SA. Nonorganic hearing loss. In Gelfand SA. Essentials of Audiology, 3rd Edition. New York: Thieme Medical Publishers; 2009;p.404-424.
- Durmaz A, Karahatay S, Satar B, et al. Efficiency of Stenger test in confirming profound unilateral pseudo- hypacusis. J Laryngol Otol. 2009;p.123(8):840-844.
- Gorga MP, Neely ST, Berman BM, et al. A Comparison of transient-evoked and distortion product emissions in normal-hearing and hearing-impaired subjects. J Acoust Soc Am. 1993;p.94(5):2639-2648.
- Balatsouras DG, Kaberos A, Korres S, et al.
- Detection of Pseudohypacusis: A Prospective Randomized Study of the use of Otoacoustic Emissions. Ear Hear. 2003;p.24(6):518-527.
- Sanders JW, Lazenby BB. Auditory brain stem response in the assessment of pseudohypacusis. Am J Otol. 1983;p.4(4): 292-299.
- Oishi N, Kanazaki S, Kataoka C, et al. Acute-onset unilateral hearing psychogenic hearing loss in adults: Reports of six cases and diagnostic pitfalls. ORL J Otorhinolaryngol Relat Spec. 2009;p.71(5):279- 283.




