PEARL STUDY Interim data presented at the European Academy of Neurology 2022 shows that 54.7% of patients in the study had their monthly-migraine-days reduced by 50% or more over the six-month period from the start of treatment.
25th June 2022: Teva Pharmaceuticals Europe B.V. announced promising interim results from its Pan-European Real World study (PEARL), presented for the first time at the European Academy of Neurology (EAN) Congress in Vienna, Austria.
The two-year Pan-European Real World (PEARL) prospective, observational study of AJOVY® (fremanezumab), looks at its effectiveness in patients with chronic migraine or episodic migraine, and is an ongoing study sponsored by Teva Pharmaceuticals Europe BV.[i] These findings further offer insight into the treatment of migraine in real-world clinical practice.
The interim findings were presented by Faisal Mohammad Amin, Associate Professor of Neurology at the University of Copenhagen, Denmark. Out of the total planned 1100 patients in PEARL, 389 patients are included in the interim analysis presented. These findings show that 54.7% of patients in the study had their monthly-migraine-days reduced by 50% or more, over the six-month period from the start of treatment. Additionally improvements could be seen in migraine-related disability in the six-month period after the first dose.
The study is particularly relevant to clinicians due its patient cohort, who come from 11 countries and approximately 100 study centres.1 This patient group illustrates both diverse populations and also a range of reimbursement settings which are important for treatment access in Europe.
The study will continue to capture data on effectiveness, and safety of fremanezumab, as well as the reason for and the outcomes of stopping and re-starting treatments.
Commenting on the findings, Professor Messoud Ashina, PEARL Coordinating Investigator from the Danish Headache Center and Department of Neurology in Rigshospitalet Glostrup, Denmark, said:
Patients with severe migraine could benefit from preventive therapy but usage of those treatments is far from optimal. These interim findings provide real-world evidence of how the burden of migraine can be reduced when the patient has access to monoclonal antibodies like fremanezumab – something neurologists around the world are already seeing in patients who did not respond to previous preventive treatments.
Dr. Danilo Lembo, Vice President and Head of EU Medical Affairs at Teva, said: “The PEARL study is encouraging as these findings confirm that preventive treatment of chronic and episodic migraine is appropriate with fremanezumab in a real world setting. Our commitment to real-world evidence studies helps clinicians to better understand the lived experience of people with migraine, support the evolution of best clinical practice and demonstrate the impact of migraine and what preventive treatments can achieve. ”
The real life experience of European patients being able to access preventive treatment is bleak. Beyond our own data and research, a recent study from the European Migraine and Headache Alliance showed that 40% of patients needed more than five years to access migraine treatments.[ii] We need real structural change to come from healthcare systems if we are to ultimately reduce the burden of migraine.
Dr. Danilo Lembo, Vice President and Head of EU Medical Affairs at Teva
Chronic migraine is defined as a headache occurring on 15 or more days per month for more than three months, which, on at least 8 days per month, has the features of migraine headache;[iii] episodic migraine is defined as having headaches on fewer than 15 days a month.[iv] The significant personal impact and burden of this severity of migraine has been shown in many studies including Teva’s own survey of 12,545 adults with migraine – ‘Beyond Migraine’, in which 45% said migraine impacts their ability to be a good partner and 42% to be a good parent, while 49% said migraine diminished their ability in the workplace. In terms of broader social impact, 46% reported hiding migraine from others.[v]
41 million people in Europe live with migraine[vi] and the disease is three times more common in women.[vii] Migraine is the second leading cause of disability in the world and the first among young women.[viii] Migraine often begins at puberty and mostly affects people aged between 35 and 45 years.[ix] It strikes during people’s most productive years (late teens to 50s).[x]
Further reading
A publication in the journal Headache presented data that shows, for AJOVY®, there is no reduction in efficacy over a dosing period. This means that the efficacy of AJOVY® was similar at the end of the dosing period compared to the start of the same dosing period, immediately following treatment admininistration. Patients using AJOVY® therefore experience the benefits of treatment throughout the entire dosing period. See Blumenfeld AM, Stevanovic DM, Ortega M et al. No “wearing-off effect” seen in quarterly or monthly dosing of fremanezumab: Subanalysis of a randomized longterm study. Headache 2020; 60: 2431–2443.
References:
[i]Ashina, M. et al, PEARL study protocol. Pain management, 11(6), 647–654. (v0.1) – The two year Pan-European Real
World (PEARL) prospective, observational study of AJOVY® (fremanezumab)
2. KPMG, prepared for the European Migraine and Headache Alliance (EMHA). “Access to Care” project: final assessment. July 2021. [online] Available at: https://www.emhalliance.org/wp-content/uploads/ATC-EMHA-Dossier.pdf
[iii] Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. (2018). Cephalalgia, 38(1), 1–211. https://doi.org/10.1177/0333102417738202
[iv] Lipton, R. B., & Silberstein, S. D. (2015). Episodic and chronic migraine headache: breaking down barriers to optimal treatment and prevention. Headache, 55 Suppl 2, 103–126. https://doi.org/10.1111/head.12505_2
[v] Beyond Migraine – The Real You. Survey conducted 2020. Teva Pharmaceuticals. Data on file.
[vi] Stovner, L. J., Andrée, C., & Eurolight Steering Committee (2008). Impact of headache in Europe: a review for the Eurolight project. The journal of headache and pain, 9(3), 139–146. https://doi.org/10.1007/s10194-008-0038-6
[vii] Al-Hassany L, Haas J, Piccininni M, Kurth T, Maassen Van Den Brink A and Rohmann J.L. (2020) Giving Researchers a Headache – Sex and Gender Differences in Migraine. Front. Neurol. 11:549038. https://doi:10.3389/fneur.2020.549038
[viii] Steiner, T.J., Stovner, L.J., Jensen, R. et al. Migraine remains second among the world’s causes of disability, and first among young women: findings from GBD2019. J Headache Pain 21, 137 (2020). https://doi.org/10.1186/s10194-020-01208-0
[ix] Who.int. 2016. Headache disorders. [online] Available at: https://www.who.int/news-room/fact-sheets/detail/headache-disorders
[x] EMHA. 2021. Migraine in the EU – Bringing women out of the shadows. [online] Available at: https://www.emhalliance.org/wp-content/uploads/Women-M-Policy-Paper-FINAL23MARCH.pdf
About PEARL
The Pan-European Real World (PEARL) study will generate important information about real-world effectiveness of fremanezumab in adult patients with chronic migraine or episodic migraine (EM). PEARL is an ongoing, 24-month, multicentre, prospective, observational, Phase IV study.
PEARL will evaluate:
- Effectiveness
- Treatment adherence and persistence
- Effectiveness in patients switching from another mAb targeting the CGRP pathway
- Concomitant preventive and acute migraine medication use
About AJOVY  (fremanezumab-vfrm) injection
(fremanezumab-vfrm) injection
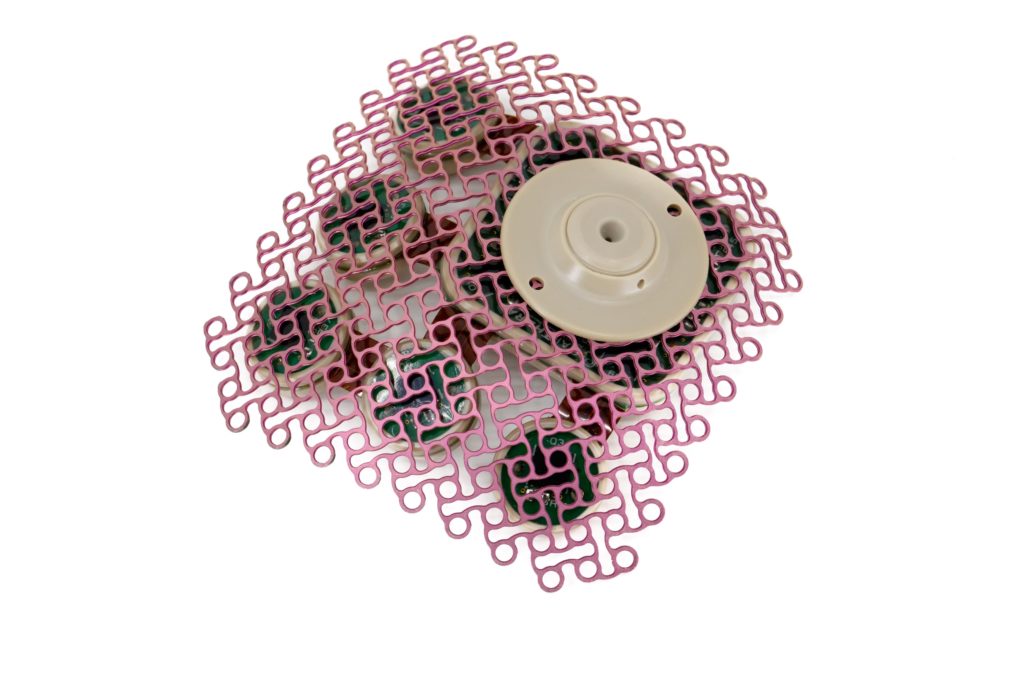
AJOVY is indicated for prophylaxis of migraine in adults who have at least 4 migraine days per month. AJOVY is available as a 225 mg/1.5 mL single dose injection in a pre-filled syringe or, in some countries, in a pre-filled pen. Two dosing options are available: 225 mg once monthly administered as one subcutaneous injection (monthly dosing), or 675 mg every three months (quarterly dosing), which is administered as three subcutaneous injections.
AJOVY can be administered either by a healthcare professional or at home by a patient or caregiver. No starting dose is required to begin treatment.
Information for Europe about AJOVY can be found here.
 This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse events. Information can be found at https://www.hpra.ie.
This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse events. Information can be found at https://www.hpra.ie.
About Teva
Teva Pharmaceutical Industries Ltd. (NYSE and TASE: TEVA) has been developing and producing medicines to improve people’s lives for more than a century. We are a global leader in generic, biosimilar and specialty medicines with a portfolio consisting of over 3,500 products in nearly every therapeutic area. Around 200 million people around the world take a Teva medicine every day and are served by one of the largest and most complex supply chains in the pharmaceutical industry. Along with our established presence in generics, we have significant innovative research and operations supporting our growing portfolio of specialty and biopharmaceutical products. Learn more at http://www.tevapharm.com